Abstract
Objective
To characterize infants who underwent autopsy in regional neonatal intensive care units (NICUs) and examine inter-center variability in autopsy completion.
Study design
Retrospective cohort study of infants who died between 2010 and 2016 from 32 participating hospitals in the Children’s Hospital Neonatal Database (CHND). Maternal/infant demographics and hospital stay data were collected, along with autopsy rates by center, year, and region. Data analysis utilized bivariate and multivariable statistics.
Result
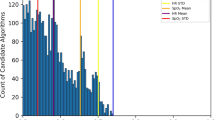
Of 6299 deaths, 1742 (27.7%) completed autopsy. Infants who underwent autopsy had higher median birth weight (2 124 g vs. 1 655 g) and gestational age (34 vs. 32 weeks). No differences were seen in sex, length of stay, or primary cause of death. Marked inter-center variability was observed, with 17-fold adjusted difference (p < 0.001) in autopsy rates.
Conclusion
Patient characteristics do not account for variability in autopsy practices across regional NICUs. Factors such as provider practices and parental preferences should be investigated.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Ely DM, Driscoll AK. Infant Mortality in the United States, 2017: Data From the Period Linked Birth/Infant Death File. Natl Vital Stat Rep. 2019;68:1–20.
Feudtner C, Feinstein JA, Satchell M, Zhao H, Kang TI. Shifting place of death among children with complex chronic conditions in the United States, 1989-2003. JAMA. 2007;297:2725–32.
Custer JW, Winters BD, Goode V, Robinson KA, Yang T, Pronovost PJ, et al. Diagnostic errors in the pediatric and neonatal ICU: a systematic review. Pediatr Crit Care Med. 2015;16:29–36.
Brodlie M, Laing IA, Keeling JW, McKenzie KJ. Ten years of neonatal autopsies in tertiary referral centre: retrospective study. BMJ. 2002;324:761–3.
Kabra NS, Udani RH. Correlation between clinical diagnoses at the time of death and autopsy findings in critically sick neonates at a regional neonatal intensive care unit in India. J Trop Pediatr. 2001;47:295–300.
Leadbetter KZ, Vesoulis ZA, White FV, Schmidt RE, Khanna G, Shimony JS, et al. The role of post-mortem MRI in the neonatal intensive care unit. J Perinatol. 2017;37:98–103.
Straumanis JP. The autopsy: still valuable in the 21st century for identifying diagnostic errors. Pediatr Crit Care Med. 2015;16:79–80.
Nese N, Bulbul Y. Diagnostic value of perinatal autopsies: analysis of 486 cases. J Perinat Med. 2018;46:175–81.
Sullivan J, Monagle P. Bereaved parents’ perceptions of the autopsy examination of their child. Pediatrics. 2011;127:e1013–20.
Blokker BM, Weustink AC, Hunink MGM, Oosterhuis JW. Autopsy rates in the Netherlands: 35 years of decline. PLoS One. 2017;12:e0178200.
Burton JL, Underwood J. Clinical, educational, and epidemiological value of autopsy. Lancet. 2007;369:1471–80.
Tsitsikas DA, Brothwell M, Chin Aleong JA, Lister AT. The attitudes of relatives to autopsy: a misconception. J Clin Pathol. 2011;64:412–4.
Khong TY. Improving perinatal autopsy rates: who is counseling bereaved parents for autopsy consent? Birth. 1997;24:55–7.
Murthy K, Dykes FD, Padula MA, Pallotto EK, Reber KM, Durand DJ, et al. The Children’s Hospitals Neonatal Database: an overview of patient complexity, outcomes and variation in care. J Perinatol. 2014;34:582–6.
Fry JT, Matoba N, Datta A, DiGeronimo R, Coghill CH, Natarajan G, et al. Center, Gestational Age, and Race Impact End-of-Life Care Practices at Regional Neonatal Intensive Care Units. J Pediatr. 2020;217:e1.
Bureau USC Census Regions and Divisions of the United States 2019 [updated April 22, 2019. Available from: https://www2.census.gov/geo/pdfs/maps-data/maps/reference/us_regdiv.pdf.
Bureau USC MEDIAN HOUSEHOLD INCOME IN THE PAST 12 MONTHS (IN 2013 INFLATION-ADJUSTED DOLLARS). In: Office USCBsACS, editor. 2013.
American Academy of Pediatrics Committee on F, Newborn. Levels of neonatal care. Pediatrics. 2012;130:587–97.
VanMarter LJ, Taylor F, Epstein MF. Parental and physician-related determinants of consent for neonatal autopsy. Am J Dis Child. 1987;141:149–53.
Kumar P, Angst DB, Taxy J, Mangurten HH. Neonatal autopsies: a 10-year experience. Arch Pediatr Adolesc Med. 2000;154:38–42.
Hickey L, Murphy A, Devaney D, Gillan J, Clarke T. The value of neonatal autopsy. Neonatology. 2012;101:68–73.
Shojania KG, Burton EC. The vanishing nonforensic autopsy. N Engl J Med. 2008;358:873–5.
Cartlidge PH, Dawson AT, Stewart JH, Vujanic GM. Value and quality of perinatal and infant postmortem examinations: cohort analysis of 400 consecutive deaths. BMJ. 1995;310:155–8.
Mjornheim B, Rosendahl A, Eriksson LC, Takman C. Attitudes of Nurses and Physicians About Clinical Autopsy in Neonatal and Adult Hospital Care: A Survey in Sweden. Nurs Res. 2015;64:264–71.
McPhee SJ, Bottles K, Lo B, Saika G, Crommie D. To redeem them from death. Reactions of family members to autopsy. Am J Med. 1986;80:665–71.
Rose C, Evans M, Tooley J. Falling rates of perinatal postmortem examination: are we to blame? Arch Dis Child Fetal Neonatal Ed. 2006;91:F465.
Gordijn SJ, Erwich JJ, Khong TY. Value of the perinatal autopsy: critique. Pediatr Dev Pathol. 2002;5:480–8.
Elder DE, Zuccollo JM. Autopsy after death due to extreme prematurity. Arch Dis Child Fetal Neonatal Ed. 2005;90:F270–2.
Durning S, Cation L. The educational value of autopsy in a residency training program. Arch Intern Med. 2000;160:997–9.
Swinton CH, Weiner J, Okah FA. The neonatal autopsy: can it be revived? Am J Perinatol. 2013;30:739–44.
Mercier CE, Dunn MS, Ferrelli KR, Howard DB, Soll RF. Vermont Oxford Network EIF-USG. Neurodevelopmental outcome of extremely low birth weight infants from the Vermont Oxford network: 1998-2003. Neonatology. 2010;97:329–38.
Verhagen AA, Janvier A, Leuthner SR, Andrews B, Lagatta J, Bos AF, et al. Categorizing neonatal deaths: a cross-cultural study in the United States, Canada, and The Netherlands. J Pediatr. 2010;156:33–7.
Weiner J, Sharma J, Lantos J, Kilbride H. How infants die in the neonatal intensive care unit: trends from 1999 through 2008. Arch Pediatr Adolesc Med. 2011;165:630–4.
Assaad MA, Lapointe A, Thivierge E, Janvier A. Mortality and Morbidity rounds in neonatology: Providers’ experiences and perspectives. Acta Paediatr. 2021;110:2737–44.
Carter BS, Guthrie SO. Utility of morbidity and mortality conference in end-of-life education in the neonatal intensive care unit. J Palliat Med. 2007;10:375–80.
Acknowledgements
We are indebted to the institutions that serve the infants and their families, and these institutions also have invested in and continue to participate in the Children’s Hospital’s Neonatal Database (CHND). A full list is located in the Supplementary Information.
Funding
This study was conducted without specific funding support
Author information
Authors and Affiliations
Consortia
Contributions
A.D., J.N., and J.W. wrote the manuscript. I.Z. provided statistical analysis and methodological review. All authors designed the project, reviewed the data, edited the manuscript, and approved the final submitted version.
Corresponding author
Ethics declarations
Competing interests
Dr. Murthy is a Board member and Chair of the CHNC (Kansas City, MO). Dr. Zaniletti is an employee of Children’s Hospitals Association, Inc (Overland Park, KS). The other authors report no conflicts of interest relevant to this article and have no financial relationships relevant to this article to disclose.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Datta, A., Niehaus, J.Z., Weiner, J. et al. Inter-center variation in autopsy practices among regional neonatal intensive care units (NICUs). J Perinatol 41, 2820–2825 (2021). https://doi.org/10.1038/s41372-021-01286-1
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41372-021-01286-1