Abstract
Objective
To assess stabilization, respiratory care and survival of extremely low birth weight (ELBW, <1000 g at birth) infants requiring emergency transfer to tertiary NICUs on the first day of life.
Study design
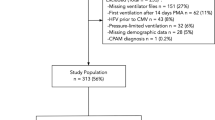
Retrospective cohort study of 55 ELBW infants transported by a dedicated neonatal transport service over a 65-month period. Ventilator data were downloaded computationally.
Results
95% of infants were intubated and received surfactant prior to transfer. Median expired tidal volume was 5.0 mL/kg (interquartile range: 4.6–6.2 mL/kg). Infants ventilated with SIPPV had significantly higher mean airway pressure and minute ventilation, but similar FiO2 compared to babies on SIMV. Blood gases showed significant improvement during transport. 55% of infants survived to discharge from NICU.
Conclusion
Most ELBW infants transferred on the first day of life require mechanical ventilation and can be ventilated with 5 mL/kg tidal volume.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
Datasets generated during the current study are available from the corresponding author on reasonable request. Analysis steps can be accessed via GitHub code repository at https://github.com/belteki/transport_ELBW.
References
Doyle LW, Ford G, Davis N. Health and hospitalizations after discharge in extremely low birth weight infants. Semin Neonatol. 2003;8:137–45.
Cheong JLY, Wark JD, Cheung MM, Irving L, Burnett AC, Lee KJ, et al. Impact of extreme prematurity or extreme low birth weight on young adult health and wellbeing: the Victorian Infant Collaborative Study (VICS) 1991–1992 Longitudinal Cohort study protocol. BMJ Open. 2019;9:e030345.
Saigal S, Doyle LW. An overview of mortality and sequelae of preterm birth from infancy to adulthood. Lancet. 2008;371:261–9.
Doyle LW, Victorian Infant Collaborative Study Group. Evaluation of neonatal intensive care for extremely low birth weight infants in Victoria over two decades: I. Effectiveness. Pediatrics. 2004;113:505–9.
Marlow N, Bryan Gill A. Establishing neonatal networks: the reality. Arch Dis Child Fetal Neonatal Ed. 2007;92:F137–42.
Marlow N, Bennett C, Draper ES, Hennessy EM, Morgan AS, Costeloe KL. Perinatal outcomes for extremely preterm babies in relation to place of birth in England:the EPICure 2 study. Arch Dis Child Fetal Neonatal Ed. 2014;99:F181–8.
Mohamed MA, Aly H. Transport of premature infants is associated with increased risk for intraventricular haemorrhage. Arch Dis Child Fetal Neonatal Ed. 2010;95:F403–7.
Gajendragadkar G, Boyd JA, Potter DW, Mellen BG, Hahn GD, Shenai JP. Mechanical vibration in neonatal transport: a randomized study of different mattresses. J Perinatol. 2000;20:307–10.
Levene MI, Fawer CL, Lamont RF. Risk factors in the development of intraventricular haemorrhage in the preterm neonate. Arch Dis Child. 1982;57:410–7.
Brennan G, Colontuono J, Carlos C. Neonatal Respiratory Support on Transport. Neoreviews. 2019;20:e202–12.
Costa JD, Sadashiv S, Hesler J, Locke RG, Blackson TJ, Mackley AB. Tidal volume monitoring during emergency neonatal transport. J Perinatol. 2018;38:1631–5.
Belteki G, Szell A, Lantos L, Kovacs G, Szanto G, Berenyi A, et al. Volume Guaranteed Ventilation During Neonatal Transport. Pediatr Crit Care Med. 2019;20:1170–6.
Morley CJ, Davis PG, Doyle LW, Brion LP, Hascoet JM, Carlin JB, et al. Nasal CPAP or intubation at birth for very preterm infants. N Engl J Med. 2008;358:700–8.
Escrig-Fernández R, Zeballos-Sarrato G, Gormaz-Moreno M, Avila-Alvarez A, Toledo-Parreño JD, Vento M. The Respiratory Management of the Extreme Preterm in the Delivery Room. Child. 2023;10:351.
Massirio P, De Paolis FM, Calevo MG, Cardiello V, Andreato C, Minghetti D, et al. Intubation Rate Evaluation of Inborn Versus Outborn Premature Newborns Affected by Respiratory Distress Syndrome: Impact of Neonatal Transport. Air Med J. 2022;41:346–9.
Williams E, Dassios T, Dixon P, Greenough A. Physiological dead space and alveolar ventilation in ventilated infants. Pediatr Res. 2022;91:218–22.
Keszler M, Nassabeh-Montazami S, Abubakar K. Evolution of tidal volume requirement during the first 3 weeks of life in infants <800 g ventilated with Volume Guarantee. Arch Dis Child Fetal Neonatal Ed. 2009;94:F279–82.
Keszler M, Montaner MB, Abubakar K. Effective ventilation at conventional rates with tidal volume below instrumental dead space: a bench study. Arch Dis Child Fetal Neonatal Ed. 2012;97:F188–92.
Hurley EH, Keszler M. Effect of inspiratory flow rate on the efficiency of carbon dioxide removal at tidal volumes below instrumental dead space. Arch Dis Child Fetal Neonatal Ed. 2017;102:F126–30.
Klingenberg C, Wheeler KI, McCallion N, Morley CJ, Davis PG. Volume-targeted versus pressure-limited ventilation in neonates. Cochrane Database Syst Rev. 2017;10:CD003666.
Vervenioti A, Fouzas S, Tzifas S, Karatza AA, Dimitriou G. Work of Breathing in Mechanically Ventilated Preterm Neonates. Pediatr Crit Care Med. 2020;21:430–6.
Batra D, Jaysainghe D, Batra N. Supporting all breaths versus supporting some breaths during synchronised mechanical ventilation in neonates: a systematic review and meta-analysis. Arch Dis Child Fetal Neonatal Ed. 2023;108:408–15.
Lantos L, Széll A, Chong D, Somogyvári Z, Belteki G. Acceleration during neonatal transport and its impact on mechanical ventilation. Arch Dis Child Fetal Neonatal Ed. 2023;108:38–44.
Acknowledgements
We thank to Rainer Kühner (Vyaire) for help with exporting data from the fabian +nCPAP evolution™ and fabian HFO ventilators. We thank to Miklos Szabo (Semmelweis University, Budapest, Hungary) for sharing national statistics on ELBW infants.
Author information
Authors and Affiliations
Contributions
VB participated in the conception of the study, collected clinical information, participated in interpretation of results, and edited the manuscript. LL participated in acquisition and interpretation of clinical data and revising the article. AV participated in interpretation of clinical data. AJ participated in interpretation of clinical data and revising the article. ZsS participated ins interpretation of clinical data and revising the article. GB was responsible for the conception of the study, the outline of statistical analysis and interpretation of data, and wrote the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
GB is a consultant to Vyaire Medical (Mettawa, IL, US) and Dräger Medical (Lübeck, Germany). Vyaire Medical did not participate in this research and did not provide any payment for it. The other authors declare no conflict of interest.
Ethics approval
The study was approved by the Scientific and Medical Research Council Ethics Committee of Hungary (reference: 40158-2/2018/EKU). Parental consent was waived. The study was performed in accordance with the Declaration of Helsinki.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Balog, V., Lantos, L., Valek, A. et al. Stabilization, respiratory care and survival of extremely low birth weight infants transferred on the first day of life. J Perinatol 45, 500–505 (2025). https://doi.org/10.1038/s41372-024-02043-w
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41372-024-02043-w