Abstract
Importance
Transcatheter closure of the patent ductus arteriosus (PDA) is being increasingly adopted as an alternative to surgical PDA closure in preterm infants.
Objective
To develop rigorous clinical practice guideline recommendations on procedural PDA closure in preterm infants.
Methods
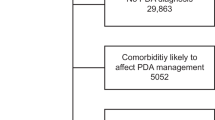
The principles of the GRADE (Grading of Recommendations Assessment, Development and Evaluation) Evidence-to-Decision (EtD) framework were used to develop the guideline recommendations. An e-Delphi survey of 45 experts was conducted and recommendations that reached ≥75% agreement were accepted as consensus.
Main recommendations
Procedural PDA closure may be considered in extremely preterm infants (<28 weeks gestational age) requiring invasive mechanical ventilation >10 postnatal days and confirmed to have a large hemodynamically significant PDA, at centers with high local rates of death and/or bronchopulmonary dysplasia (conditional recommendation). If sufficient institutional expertise is available and patient characteristics are suitable, transcatheter PDA closure may be considered as the preferred approach over PDA ligation (conditional recommendation).
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Horbar JD, Edwards EM, Greenberg LT, Morrow KA, Soll RF, Buus-Frank ME, et al. Variation in performance of neonatal intensive care units in the United States. JAMA Pediatr. 2017;171:e164396.
Benitz WE, Committee on Fetus and Newborn, American Academy of Pediatrics. Patent ductus arteriosus in preterm infants. Pediatrics. 2016;137:e20153730.
Mitra S, de Boode WP, Weisz DE, Shah PS. Interventions for patent ductus arteriosus (PDA) in preterm infants: an overview of cochrane systematic reviews. Cochrane Database Syst Rev. 2023;4:CD013588.
Ohlsson A, Walia R, Shah SS. Ibuprofen for the treatment of patent ductus arteriosus in preterm or low birth weight (or both) infants. Cochrane Database Syst Rev. 2020;11:CD003481.
Evans P, O’Reilly D, Flyer JN, Soll R, Mitra S. Indomethacin for symptomatic patent ductus arteriosus in preterm infants. Cochrane Database Syst Rev. 2021;1:CD013133.
Jasani B, Mitra S, Shah PS. Paracetamol (acetaminophen) for patent ductus arteriosus in preterm or low birth weight infants. Cochrane Database Syst Rev. 2022;12:CD010061.
Altit G, Saeed S, Beltempo M, Claveau M, Lapointe A, Basso O. Outcomes of extremely premature infants comparing patent ductus arteriosus management approaches. J Pediatr. 2021;0. https://www.jpeds.com/article/S0022-3476(21)00335-8/abstract.
Chinawa JM, Chukwu BF, Chinawa AT, Duru CO. The effects of ductal size on the severity of pulmonary hypertension in children with patent ductus arteriosus (PDA): a multi-center study. BMC Pulm Med. 2021;21:79.
Gentle SJ, Travers CP, Clark M, Carlo WA, Ambalavanan N. Patent ductus arteriosus and development of bronchopulmonary dysplasia-associated pulmonary hypertension. Am J Respir Crit Care Med. 2023;207:921–8.
Weisz DE, More K, McNamara PJ, Shah PS. PDA ligation and health outcomes: a meta-analysis. Pediatrics. 2014;133:e1024–1046.
Weisz DE, Mirea L, Rosenberg E, Jang M, Ly L, Church PT, et al. Association of patent ductus arteriosus ligation with death or neurodevelopmental impairment among extremely preterm infants. JAMA Pediatr. 2017;171:443–9.
Bischoff AR, Jasani B, Sathanandam SK, Backes C, Weisz DE, McNamara PJ. Percutaneous closure of patent ductus arteriosus in infants 1.5 kg or less: a meta-analysis. J Pediatr. 2021;230:84–92.e14.
Shah ZS, Clark RH, Patt HA, Backes CH, Tolia VN. Trends in procedural closure of the patent ductus arteriosus among infants born at 22 to 30 weeks’ gestation. J Pediatr. 2023;263:113716.
Lai KC, Richardson T, Berman D, DeMauro SB, King BC, Lagatta J, et al. Current trends in invasive closure of patent ductus arteriosus in very low birth weight infants in United States Children’s Hospitals, 2016-2021. J Pediatr. 2023;263:113712.
Backes CH, Rivera BK, Bridge JA, Armstrong AK, Boe BA, Berman DP, et al. Percutaneous patent ductus arteriosus (PDA) closure during infancy: a meta-analysis. Pediatrics. 2017;139:e20162927.
Hamrick SEG, Sallmon H, Rose AT, Porras D, Shelton EL, Reese J, et al. Patent ductus arteriosus of the preterm infant. Pediatrics. 2020;146:e20201209.
Mitra S, Weisz D, Jain A, Jong G‘T. Management of the patent ductus arteriosus in preterm infants. Paediatr Child Health 2022;27:63–63.
Moberg J, Alonso-Coello P, Oxman AD. GRADE evidence to decision (EtD) frameworks guidance. Version 1.1 [updated May 2015]. The GRADE Working Group; 2015. https://ietd.epistemonikos.org/#/help/guidance.
Piggott T, Brozek J, Nowak A, Dietl H, Dietl B, Saz-Parkinson Z, et al. Using GRADE evidence to decision frameworks to choose from multiple interventions. J Clin Epidemiol. 2021;130:117–24.
Qaseem A, Wilt TJ, Clinical Guidelines Committee of the American College of Physicians. Disclosure of interests and management of conflicts of interest in clinical guidelines and guidance statements: methods from the Clinical Guidelines Committee of the American College of Physicians. Ann Intern Med. 2019;171:354–61.
Jensen EA, Dysart K, Gantz MG, McDonald S, Bamat NA, Keszler M, et al. The diagnosis of bronchopulmonary dysplasia in very preterm infants. an evidence-based approach. Am J Respir Crit Care Med. 2019;200:751–9.
Bouck Z, Straus SE, Tricco AC. Systematic versus rapid versus scoping reviews. Methods Mol Biol. 2022;2345:103–19.
Malviya MN, Ohlsson A, Shah SS. Surgical versus medical treatment with cyclooxygenase inhibitors for symptomatic patent ductus arteriosus in preterm infants. Cochrane Database Syst Rev. 2013;2013:CD003951.
Lingappan K, Malviya MN, Pammi M, Mitra S. Invasive management for patent ductus arteriosus in preterm infants. Cochrane Database Syst Rev. 2023;2023:CD014862.
Barcroft M, McKee C, Berman DP, Taylor RA, Rivera BK, Smith CV, et al. Percutaneous closure of patent ductus arteriosus. Clin Perinatol. 2022;49:149–66.
Mitchell CC, Rivera BK, Cooper JN, Smith CV, Berman DP, Slaughter JL, et al. Percutaneous closure of the patent ductus arteriosus: opportunities moving forward. Congenit Heart Dis. 2019;14:95–9.
Scerbo D, Cua CL, Rivera BK, Marzec LC, Smith CV, Slaughter JL, et al. Percutaneous closure of the patent ductus arteriosus in very-low-weight infants. Neoreviews. 2020;21:e469–78.
Alonso-Coello P, Schünemann HJ, Moberg J, Brignardello-Petersen R, Akl EA, Davoli M, et al. GRADE evidence to decision (EtD) frameworks: a systematic and transparent approach to making well informed healthcare choices. 1: Introduction. BMJ. 2016;353. https://www.bmj.com/content/353/bmj.i2016.
Clyman RI, Kaempf J, Liebowitz M, Erdeve O, Bulbul A, Håkansson S, et al. Prolonged tracheal intubation and the association between patent ductus arteriosus and bronchopulmonary dysplasia: a secondary analysis of the PDA-TOLERATE trial. J Pediatr. 2021;229:283–8.
Clyman RI, Hills NK, Cambonie G, Debillon T, Ligi I, Gascoin G, et al. Patent ductus arteriosus, tracheal ventilation, and the risk of bronchopulmonary dysplasia. Pediatr Res. 2022;91:652–8.
Wickremasinghe AC, Rogers EE, Piecuch RE, Johnson BC, Golden S, Moon-Grady AJ, et al. Neurodevelopmental outcomes following two different treatment approaches (early ligation and selective ligation) for patent ductus arteriosus. J Pediatr. 2012;161:1065–72.
Krishnappa S, Shah PS, Jain A, Resende MHF, McNamara PJ, Weisz DE. Predictors of early extubation after patent ductus arteriosus ligation among infants born extremely preterm dependent on mechanical ventilation. J Pediatr. 2019;214:222–226.e3.
Sathanandam SK, Gutfinger D, O’Brien L, Forbes TJ, Gillespie MJ, Berman DP, et al. Amplatzer Piccolo Occluder clinical trial for percutaneous closure of the patent ductus arteriosus in patients ≥700 grams. Catheter Cardiovasc Inter. 2020;96:1266–76.
Morray BH, Sathanandam SK, Forbes T, Gillespie M, Berman D, Armstrong AK, et al. 3-year follow-up of a prospective, multicenter study of the Amplatzer PiccoloTM Occluder for transcatheter patent ductus arteriosus closure in children ≥700 grams. J Perinatol. 2023;43:1238–44.
Duboue PM, Padovani P, Bouteiller XP, Martin-Kabore F, Benbrik N, Gronier CG, et al. Post-ligation cardiac syndrome after surgical versus transcatheter closure of patent ductus arteriosus in low body weight premature infants: a multicenter retrospective cohort study. Eur J Pediatr. 2024;183:2193–2201.
Malekzadeh Milani SG, Lefort B, Dauphin C, Douchin S, Akhavi A, Bakloul M, et al. Early and mid-term results of transcatheter PDA closure in extremely low birth weight patient: a nationwide prospective series. Arch Cardiovasc Dis. 2024;117:S126.
Kuntz MT, Staffa SJ, Graham D, Faraoni D, Levy P, DiNardo J, et al. Trend and outcomes for surgical versus transcatheter patent ductus arteriosus closure in neonates and infants at US Children’s Hospitals. J Am Heart Assoc. 2022;11:e022776.
da Costa RN, Ribeiro MS, da Silva AF, Ribeiro RA, Berwanger O, Biasi A, et al. Incremental cost-effectiveness of surgical vs. percutaneous treatment of patent ductus arteriosus with the amplatzerTM duct occluder in children: a systematic review. Rev Bras Cardiol Invasiva. 2014;22:168–79.
McMaster University > CE&B Grade > Guideline Development Checklist. https://cebgrade.mcmaster.ca/guidecheck.html.
Brouwers MC, Kerkvliet K, Spithoff K, AGREE Next Steps Consortium. The AGREE reporting checklist: a tool to improve reporting of clinical practice guidelines. BMJ. 2016;352:i1152.
Liebowitz M, Katheria A, Sauberan J, Singh J, Nelson K, Hassinger DC, et al. Lack of equipoise in the PDA-TOLERATE trial: a comparison of eligible infants enrolled in the trial and those treated outside the trial. J Pediatr. 2019;213:222–226.e2.
Relangi D, Somashekar S, Jain D, Vanbuskirk S, Bancalari E, Sosenko I, et al. Changes in patent ductus arteriosus treatment strategy and respiratory outcomes in premature infants. J Pediatr. 2021;235:58–62.
Kikuchi N, Goto T, Katsumata N, Murakami Y, Shinohara T, Maebayashi Y, et al. Correlation between the closure time of patent ductus arteriosus in preterm infants and long-term neurodevelopmental outcome. J Cardiovasc Dev Dis. 2024;11:26.
Engeseth MS, Olsen NR, Maeland S, Halvorsen T, Goode A, Røksund OD. Left vocal cord paralysis after patent ductus arteriosus ligation: a systematic review. Paediatr Respir Rev. 2018;27:74–85.
Backes CH, Kennedy KF, Locke M, Cua CL, Ball MK, Fick TA, et al. Transcatheter occlusion of the patent ductus arteriosus in 747 infants <6 kg: insights from the NCDR IMPACT registry. JACC Cardiovasc Interv 2017;10:1729–37.
Bischoff AR, Kennedy KF, Backes CH, Sathanandam S, McNamara PJ. Percutaneous closure of the patent ductus arteriosus in infants ≤2 kg: IMPACT registry insights. Pediatrics. 2023;152:e2023061460.
Hundscheid T, Onland W, Kooi EMW, Vijlbrief DC, de Vries WB, Dijkman KP, et al. Expectant management or early ibuprofen for patent ductus arteriosus. N Engl J Med. 2023;388:980–90.
Gupta S, Subhedar NV, Bell JL, Field D, Bowler U, Hutchison E, et al. Trial of selective early treatment of patent ductus arteriosus with ibuprofen. N Engl J Med. 2024;390:314–25.
Author information
Authors and Affiliations
Contributions
SM developed the clinical practice guideline outline, summarized the evidence, co-chaired the panel meetings, prepared the draft recommendations, wrote the manuscript draft. ARB created and distributed the e-Delphi survey, collated and analyzed the results, participated in the panel meetings, reviewed all drafts, and approved the final version of the manuscript. SS participated in the panel meetings, reviewed all drafts, and approved the final version of the manuscript. SL participated in the panel meetings, created the summary of recommendations figure, reviewed all drafts, and approved the final version of the manuscript. PJM conceived the project, chaired the panel meetings, reviewed all drafts, and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
S. Sathanandam: proctor/consultant Abbott. Other authors do not have any conflicts to disclose.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Mitra, S., Bischoff, A.R., Sathanandam, S. et al. Procedural closure of the patent ductus arteriosus in preterm infants: a clinical practice guideline. J Perinatol 44, 1402–1408 (2024). https://doi.org/10.1038/s41372-024-02052-9
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41372-024-02052-9
This article is cited by
-
Hemodynamically significant PDA impacts adverse outcomes in infants with BPD: a multicenter study
Pediatric Research (2026)
-
Management of the patent ductus arteriosus among infants born at 23 to 32 weeks’ gestation between 2011 to 2022: a report from in the Children’s Hospitals Neonatal Consortium
Journal of Perinatology (2025)
-
Diagnosis of patent ductus arteriosus by different echocardiographic methods in very preterm infants
European Journal of Pediatrics (2025)