Abstract
Objective
To assess the usefulness of time to positivity (TTP) to distinguish between sepsis and contamination in coagulase-negative staphylococci (CoNS) isolates.
Study design
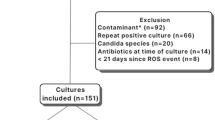
Unicentric retrospective observational. Medical records of 168 patients with suspected sepsis and positive blood culture for CoNS were reviewed. Patients were subdivided into sepsis (29%) and probable contamination (71%). Logistic regression analyses were performed to evaluate different risk factors and clinical signs and symptoms associated with sepsis.
Results
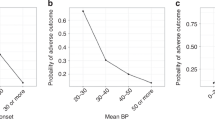
TTP cut-off value that best discriminated sepsis from contamination was found to be 18 h. Regression analysis revealed that TTP ≤ 18 h, gestational age ≤32 weeks, taquycardia/bradycardia and hypoactivity/lethargy were independent predictors of sepsis.
Conclusion
TTP is useful in distinguishing sepsis from contamination, especially in neonates with lower gestational age (<32 weeks). The clinical signs that most increase the discriminatory power of TTP are the presence of tachycardia/bradycardia or hypoactivity.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author, SC-S, upon reasonable request.
References
Shane AL, Sánchez PJ, Stoll BJ. Neonatal sepsis. Lancet. 2017;390:1770–80.
Speier RL, Cotten CM, Benjamin DK, Lewis K, Keeler K, Kidimbu G, et al. Late-onset sepsis evaluation and empiric therapy in extremely low gestational age newborns. J Pediatr Infect Dis Soc. 2023;12:S37–43.
Cantey JB, Pyle AK, Wozniak PS, Hynan LS, Sánchez PJ. Early antibiotic exposure and adverse outcomes in preterm, very low birth weight infants. J Pediatr. 2018;203:62–7.
Healy CM, Baker CJ, Palazzi DL, Campbell JR, Edwards MS. Distinguishing true coagulase-negative Staphylococcus infections from contaminants in the neonatal intensive care unit. J Perinatol. 2013;33:52–8.
Struthers S, Underhill H, Albersheim S, Greenberg D, Dobson S. A comparison of two versus one blood culture in the diagnosis and treatment of coagulase-negative staphylococcus in the neonatal intensive care unit. J Perinatol. 2002;22:547–9.
López Sastre JB, Coto Cotallo D, Fernández Colomer B, Grupo de Hospitales Castrillo. Neonatal sepsis of nosocomial origin: an epidemiological study from the ‘Grupo de Hospitales Castrillo’. J Perinat Med. 2002;30:149–57.
Hajjar N, Ting JY, Shah PS, Lee K-S, Dunn MS, Srigley JA, et al. Blood culture collection practices in NICU; A national survey. Paediatr Child Health. 2023;28:166–71.
Ryder JH, Van Schooneveld TC, Diekema DJ, Fabre V. Every crisis is an opportunity: advancing blood culture stewardship during a blood culture bottle shortage. Open Forum Infect Dis 2024;11. https://doi.org/10.1093/ofid/ofae479.
Mukhopadhyay S, Briker SM, Flannery DD, Dhudasia MB, Coggins SA, Woodford E, et al. Time to positivity of blood cultures in neonatal late-onset bacteraemia. Arch Dis Child Fetal Neonatal Ed. 2022;107:583–8.
Gastmeier P, Geffers C, Schwab F, Fitzner J, Obladen M, Rüden H. Development of a surveillance system for nosocomial infections: the component for neonatal intensive care units in Germany. J Hospital Infect. 2004;57:126–31.
Piening BC, Geffers C, Gastmeier P, Schwab F. Pathogen-specific mortality in very low birth weight infants with primary bloodstream infection. PLoS One. 2017;12. https://doi.org/10.1371/journal.pone.0180134.
Wójkowska-Mach J, Gulczyńska E, Nowiczewski M, Borszewska-Kornacka M, Domańska J, Merritt TA et al. Late-onset bloodstream infections of Very-Low-Birth-Weight infants: Data from the Polish Neonatology Surveillance Network in 2009-2011. BMC Infect Dis. 2014;14. https://doi.org/10.1186/1471-2334-14-339.
Singh J, Jain S, Chawla D, Randev S, Khurana S. Peripheral perfusion index as a marker of sepsis in preterm neonates. J Trop Pediatr. 2022;68. https://doi.org/10.1093/tropej/fmac014.
Cantey JB, Baird SD. Ending the culture of culture-negative sepsis in the neonatal ICU. Pediatrics. 2017;140. https://doi.org/10.1542/peds.2017-0044.
Fernandez Colomer B, Cernada Badia M, Coto Cotallo D, Lopez Sastre J. The Spanish National Network Grupo Castrillo: 22 Years of Nationwide Neonatal Infection Surveillance. Am J Perinatol. 2020;37:S71–75.
Kuzniewicz MW, Mukhopadhyay S, Li S, Walsh EM, Puopolo KM. Time to positivity of neonatal blood cultures for early-onset sepsis. Pediatr Infect Dis J. 2020;39:634–40.
Arias-Felipe A, Ramírez-Berrios J, Recio-Martinez R, Orellana-Miguel MA, Fontiveros-Escalona D, Bergón-Sendín E, et al. Determining time to positivity of blood cultures in a neonatal unit. J Pediatr Infect Dis Soc. 2022;11:510–3.
Craft A, Finer N. Nosocomial coagulase negative staphylococcal (CoNS) catheter-related sepsis in preterm infants: definition, diagnosis, prophylaxis, and prevention. J Perinatol. 2001;21:186–92.
Flannery DD, Edwards EM, Coggins SA, Horbar JD, Puopolo KM. Late-onset sepsis among very preterm infants. Pediatrics. 2022;150. https://doi.org/10.1542/PEDS.2022-058813.
Sarkar S, Bhagat I, DeCristofaro JD, Wiswell TE, Spitzer AR. A study of the role of multiple site blood cultures in the evaluation of neonatal sepsis. J Perinatol. 2006;26:18–22.
Freeman J, Goldmann DA, Smith NE, Sidebottom DG, Epstein MF, Platt R. Association of intravenous lipid emulsion and coagulase-negative staphylococcal bacteremia in neonatal intensive care units. N. Engl J Med. 1990;323:301–8.
Schelonka RL, Chai MK, Yoder BA, Hensley D, Brockett RM, Ascher DP. Volume of blood required to detect common neonatal pathogens. J Pediatr. 1996;129:275–8.
Connell TG, Rele M, Cowley D, Buttery JP, Curtis N. How reliable is a negative blood culture result? Volume of blood submitted for culture in routine practice in a children’s hospital. Pediatrics. 2007;119:891–6.
Miller JM, Binnicker MJ, Campbell S, Carroll KC, Chapin KC, Gilligan PH, et al. A guide to utilization of the microbiology laboratory for diagnosis of infectious diseases: 2018 update by the infectious diseases society of america and the american society for microbiology. Clin Infect Dis. 2018;67:e1–94.
Garcia-Prats JA, Cooper TR, Schneider VF, Stager CE, Hansen TN. Rapid detection of microorganisms in blood cultures of newborn infants utilizing an automated blood culture system. Pediatrics. 2000;105:523–7.
Jardine L, Davies MW, Faoagali J. Incubation time required for neonatal blood cultures to become positive. J Paediatr Child Health. 2006;42:797–802.
Huggard D, Powell J, Kirkham C, Power L, O’Connell NH, Philip RK. Time to positivity (TTP) of neonatal blood cultures: a trend analysis over a decade from Ireland. J Matern-Fetal Neonatal Med. 2021;34:780–6.
Author information
Authors and Affiliations
Contributions
Study design (SC-S, BO, JE-C, JC, DN), data collection (SC-S, RP-S, JC), analyses (BO, EG), first manuscript draft (SC-S, BO, JE-C). All authors revised the manuscript critically for substantive content and approved the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Carbonell-Sahuquillo, S., Olea, B., Pérez-Suárez, R. et al. Time to positivity of Coagulase Negative Staphylococcus In Neonatal Blood Cultures as an adjunct tool to help discriminate between sepsis and contamination. J Perinatol 45, 111–115 (2025). https://doi.org/10.1038/s41372-024-02158-0
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41372-024-02158-0
This article is cited by
-
MedTransNet: a transformer-based clinical decision support framework for early infectious disease prognosis and antimicrobial stewardship
Network Modeling Analysis in Health Informatics and Bioinformatics (2025)