Abstract
Objective
To analyze the approach to cardiovascular care and long-term outcomes in infants undergoing hypothermia for neonatal encephalopathy (NE).
Study design
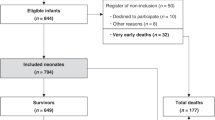
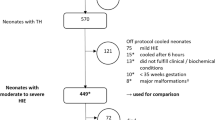
This is a retrospective cohort study of 152 infants with NE [SickKids Hospital (Center A, n = 74) or Semmelweis University (Center B, n = 78)], who developed hypotension and underwent neonatal follow-up. Primary outcome was defined as death or neurodevelopmental impairment (<70 on Bayley-II or <85 points on Bayley-III test).
Result
The presence of hypoxic injury in the brain MRI increased the odds of adverse outcome by 10.5 fold. In addition, for every 24 h increase in the duration of cardiovascular support the odds of adverse outcome increased by 12%. In a subgroup of patients with detailed echocardiography evaluation lower tricuspid annulus plane systolic excursion was noted in the non-survivors.
Conclusion
Hypoxic brain injury and longer cardiovascular therapy are independently associated with the adverse long-term outcome in patients with NE.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Shah P, Riphagen S, Beyene J, Perlman M. Multiorgan dysfunction in infants with post-asphyxial hypoxic-ischaemic encephalopathy. Arch Dis Child Fetal Neonatal Ed. 2004;89:F152–5.
Giesinger RE, Bailey LJ, Deshpande P, McNamara PJ. Hypoxic-Ischemic Encephalopathy and Therapeutic Hypothermia: The Hemodynamic Perspective. J Pediatr. 2017;180:22–30.e2.
Kovacs K, Giesinger RE, Lakatos A, Szabo AJ, Szabo M, Jermendy A, et al. Comparative evaluation of approach to cardiovascular care in neonatal encephalopathy undergoing therapeutic hypothermia. J Perinatol. 2022;42:1637–43.
Giesinger RE, Levy PT, Ruoss JL, El Dib M, Mohammad K, Wintermark P, et al. Cardiovascular management following hypoxic-ischemic encephalopathy in North America: need for physiologic consideration. Pediatr Res. 2020;90:600–7.
Pang R, Mintoft A, Crowley R, Sellwood M, Mitra S, Robertson NJ. Optimizing hemodynamic care in neonatal encephalopathy. Semin Fetal Neonatal Med. 2020;25:101139.
Giesinger RE, El Shahed AI, Castaldo MP, Bischoff AR, Chau V, Whyte HEA, et al. Neurodevelopmental outcome following hypoxic ischaemic encephalopathy and therapeutic hypothermia is related to right ventricular performance at 24-hour postnatal age. Arch Dis Child Fetal Neonatal Ed. 2022;107:70–5.
Giesinger RE, El Shahed AI, Castaldo MP, Breatnach CR, Chau V, Whyte HE, et al. Impaired Right Ventricular Performance Is Associated with Adverse Outcome after Hypoxic Ischemic Encephalopathy. Am J Respir Crit Care Med. 2019;200:1294–305.
Azzopardi DV, Strohm B, Edwards AD, Dyet L, Halliday HL, Juszczak E, et al. Moderate Hypothermia to Treat Perinatal Asphyxial Encephalopathy. N Engl J Med. 2009;361:1349–58.
Baker CF, Barks JD, Engmann C, Vazquez DM, Neal CR Jr, Schumacher RE, et al. Hydrocortisone administration for the treatment of refractory hypotension in critically ill newborns. J Perinatol. 2008;28:412–9.
Barkovich AJ, Hajnal BL, Vigneron D, Sola A, Partridge JC, Allen F, et al. Prediction of neuromotor outcome in perinatal asphyxia: evaluation of MR scoring systems. AJNR Am J Neuroradiol. 1998;19:143–9.
Chau V, Poskitt KJ, Sargent MA, Lupton BA, Hill A, Roland E, et al. Comparison of computer tomography and magnetic resonance imaging scans on the third day of life in term newborns with neonatal encephalopathy. Pediatrics. 2009;123:319–26.
Tabban HA HI, ABHS-R, Salem KY, Salem TA, Ibrahim S. Hypoxic Ischemic Encephalopathy MRI Findings and Patterns Review, Revisited. OMICS J Radiol. 2022;11:415.
Mertens L, Seri I, Marek J, Arlettaz R, Barker P, McNamara P, et al. Targeted Neonatal Echocardiography in the Neonatal Intensive Care Unit: practice guidelines and recommendations for training. Writing Group of the American Society of Echocardiography (ASE) in collaboration with the European Association of Echocardiography (EAE) and the Association for European Pediatric Cardiologists (AEPC). J Am Soc Echocardiogr. 2011;24:1057–78.
Jain A, El-Khuffash AF, Kuipers BCW, Mohamed A, Connelly KA, McNamara PJ, et al. Left Ventricular Function in Healthy Term Neonates During the Transitional Period. J Pediatr. 2017;182:197–203.e2.
Jain A, Mohamed A, El-Khuffash A, Connelly KA, Dallaire F, Jankov RP, et al. A comprehensive echocardiographic protocol for assessing neonatal right ventricular dimensions and function in the transitional period: normative data and z scores. J Am Soc Echocardiogr. 2014;27:1293–304.
Slama M, Susic D, Varagic J, Ahn J, Frohlich ED. Echocardiographic measurement of cardiac output in rats. Am J Physiol Heart Circ Physiol. 2003;284:H691–7.
Levy PT, El Khuffash A, Woo KV, Singh GK. Right Ventricular-Pulmonary Vascular Interactions: An Emerging Role for Pulmonary Artery Acceleration Time by Echocardiography in Adults and Children. J Am Soc Echocardiogr. 2018;31:962–4.
Jary S, Whitelaw A, Walloe L, Thoresen M. Comparison of Bayley-2 and Bayley-3 scores at 18 months in term infants following neonatal encephalopathy and therapeutic hypothermia. Dev Med Child Neurol. 2013;55:1053–9.
Joynt C, Cheung PY. Cardiovascular Supportive Therapies for Neonates With Asphyxia - A Literature Review of Pre-clinical and Clinical Studies. Front Pediatr. 2018;6:363.
Giesinger RE, McNamara PJ. Hemodynamic instability in the critically ill neonate: An approach to cardiovascular support based on disease pathophysiology. Semin Perinatol. 2016;40:174–88.
Gluckman PD, Wyatt JS, Azzopardi D, Ballard R, Edwards AD, Ferriero DM, et al. Selective head cooling with mild systemic hypothermia after neonatal encephalopathy: multicentre randomised trial. Lancet. 2005;365:663–70.
Shankaran S, Laptook AR, Ehrenkranz RA, Tyson JE, McDonald SA, Donovan EF, et al. Whole-body hypothermia for neonates with hypoxic-ischemic encephalopathy. N Engl J Med. 2005;353:1574–84.
Al Balushi A, Barbosa Vargas S, Maluorni J, Sanon PN, Rampakakis E, Saint-Martin C, et al. Hypotension and Brain Injury in Asphyxiated Newborns Treated with Hypothermia. Am J Perinatol. 2018;35:31–8.
Pryds O, Greisen G, Lou H, Friis-Hansen B. Vasoparalysis associated with brain damage in asphyxiated term infants. J Pediatr. 1990;117:119–25.
Balog V, Vatai B, Kovacs K, Szabo AJ, Szabo M, Jermendy A. Time series analysis of non-invasive hemodynamic monitoring data in neonates with hypoxic-ischemic encephalopathy. Front Pediatr. 2023;11:1112959.
Tsuda K, Iwata S, Mukai T, Shibasaki J, Takeuchi A, Ioroi T, et al. Body Temperature, Heart Rate, and Short-Term Outcome of Cooled Infants. Ther Hypothermia Temp Manag. 2019;9:76–85.
Tsuda K, Shibasaki J, Isayama T, Takeuchi A, Mukai T, Ioroi T, et al. Body temperature, heart rate and long-term outcome of cooled infants: an observational study. Pediatr Res. 2022;91:921–8.
Goulding RM, Stevenson NJ, Murray DM, Livingstone V, Filan PM, Boylan GB. Heart rate variability in hypoxic ischemic encephalopathy: correlation with EEG grade and 2-y neurodevelopmental outcome. Pediatr Res. 2015;77:681–7.
Goulding RM, Stevenson NJ, Murray DM, Livingstone V, Filan PM, Boylan GB. Heart rate variability in hypoxic ischemic encephalopathy during therapeutic hypothermia. Pediatr Res. 2017;81:609–15.
Presacco A, Chirumamilla VC, Vezina G, Li R, Du Plessis A, Massaro AN, et al. Prediction of outcome of hypoxic-ischemic encephalopathy in newborns undergoing therapeutic hypothermia using heart rate variability. J Perinatol. 2024;44:521–7.
Mohammad K, Hicks M, Buchhalter J, Esser MJ, Irvine L, Thomas S, et al. Hemodynamic instability associated with increased risk of death or brain injury in neonates with hypoxic ischemic encephalopathy. J Neonatal Perinat Med. 2017;10:363–70.
Bashir RA, Vayalthrikkovil S, Espinoza L, Irvine L, Scott J, Mohammad K. Prevalence and Characteristics of Intracranial Hemorrhages in Neonates with Hypoxic Ischemic Encephalopathy. Am J Perinatol. 2018;35:676–81.
Kovacs K, Szakmar E, Meder U, Cseko A, Szabo AJ, Szabo M, et al. Serum cortisol levels in asphyxiated infants with hypotension. Early Hum Dev. 2018;120:40–5.
Kovacs K, Szakmar E, Meder U, Szakacs L, Cseko A, Vatai B, et al. A Randomized Controlled Study of Low-Dose Hydrocortisone Versus Placebo in Dopamine-Treated Hypotensive Neonates Undergoing Hypothermia Treatment for Hypoxic-Ischemic Encephalopathy. J Pediatr. 2019;211:13–9.e3.
Sehgal A, Wong F, Menahem S. Speckle tracking derived strain in infants with severe perinatal asphyxia: a comparative case control study. Cardiovasc Ultrasound. 2013;11:34.
Simovic AM, Prijic SM, Knezevic JB, Igrutinovic ZR, Vujic AJ, Kosutic J. Predictive value of biochemical, echocardiographic and electrocardiographic markers in non-surviving and surviving asphyxiated full-term newborns. Turk J Pediatr. 2014;56:243–9.
More KS, Sakhuja P, Giesinger RE, Ting JY, Keyzers M, Sheth JN, et al. Cardiovascular Associations with Abnormal Brain Magnetic Resonance Imaging in Neonates with Hypoxic Ischemic Encephalopathy Undergoing Therapeutic Hypothermia and Rewarming. Am J Perinatol. 2018;35:979–89.
Bos AF. Bayley-II or Bayley-III: what do the scores tell us? Dev Med Child Neurol. 2013;55:978–9.
Lowe JR, Erickson SJ, Schrader R, Duncan AF. Comparison of the Bayley II Mental Developmental Index and the Bayley III Cognitive Scale: are we measuring the same thing? Acta Paediatr. 2012;101:e55–8.
Moore T, Johnson S, Haider S, Hennessy E, Marlow N. Relationship between test scores using the second and third editions of the Bayley Scales in extremely preterm children. J Pediatr. 2012;160:553–8.
Sharp M, DeMauro SB. Counterbalanced Comparison of the BSID-II and Bayley-III at Eighteen to Twenty-two Months Corrected Age. J Dev Behav Pediatr. 2017;38:322–9.
Acknowledgements
KK was supported by the Hungarian Scientific Research Fund, Postdoctoral excellence programme (OTKA PD 142288). AJ was supported by OTKA FK 135222 and TKP2021-EGA25 grants of the National Research, Development and Innovation Office, Hungary. Project no. RRF-2.3.1-21-2022-00011, titled National Laboratory of Translational Neuroscience has been implemented with the support provided by the Recovery and Resilience Facility of the European Union within the framework of Programme Széchenyi Plan Plus. The funding agencies had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript. Previous presentation: Some parts of our study results were presented at the Pediatric Academic Societies 2024 Meeting in Toronto.
Author information
Authors and Affiliations
Contributions
KK was responsible for designing the work that led to the submission, analyzing data, interpreting results and drafting the manuscript. REG played an important role in acquiring data and interpreting the results. ZsV, MSz and AJSz contributed to conception, design and interpretation of data and revised the manuscript critically. AJ had substantial contributions to conception and design, acquisition of data, revising the article critically for important intellectual content. PJM, as the corresponding author had full access to the data in the study and had final responsibility for the decision to submit for publication. He also had substantial contributions to conception and design and critically revised the manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kovacs, K., Giesinger, R.E., Varga, Z. et al. Association between cardiovascular care and neurodevelopmental outcomes in infants with neonatal encephalopathy and hemodynamic instability. J Perinatol 45, 1073–1080 (2025). https://doi.org/10.1038/s41372-025-02230-3
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41372-025-02230-3