Abstract
Objective
To compare pulmonary function tests (PFTs), specifically passive respiratory system compliance (Crs), in infants of mothers positive for COVID-19 during pregnancy compared to PFTs from a historical cohort of matched, healthy reference infants.
Study design
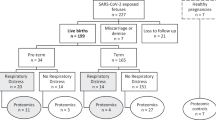
A prospective cohort study of infants born to COVID-19 positive mothers. Crs was measured with the single breath occlusion technique. Historical cohort data was obtained from a pre-COVID-19 data repository. Respiratory questionnaires were done at 1-year postnatal age.
Results
Twenty-four PFTs in the COVID-19 cohort were compared with PFTs from 24 reference subjects. Infants of the COVID-19 positive mothers had a Crs of 3.57 ml/cmH2O versus 3.76 mL/cmH2O in the reference group (p > 0.05). The remaining PFT outcomes were comparable between groups. The COVID-19 infants reported more allergic symptoms and conditions through 1-year.
Conclusion
We found no difference in Crs in infants of mothers with COVID-19 during pregnancy compared to a historical pre-COVID reference cohort.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
Datasets that support the findings of this study are available from the corresponding author, upon reasonable request.
References
WHO Coronavirus (COVID-19) dashboard (2020). Accessed: 29th Sept 2024: https://covid19.who.int
Allotey J, Stallings E, Bonet M, Yap M, Chatterjee S, Kew T, et al. Clinical manifestations, risk factors, and maternal and perinatal outcomes of coronavirus disease 2019 in pregnancy: living systematic review and meta-analysis. BMJ. 2020;370:m3320.
Angelidou A, Sullivan K, Melvin PR, Shui JE, Goldfarb IT, Bartolome R, et al. Association of Maternal Perinatal SARS-CoV-2 Infection With Neonatal Outcomes During the COVID-19 Pandemic in Massachusetts. JAMA Netw Open. 2021;4:e217523.
Chen H, Guo J, Wang C, Luo F, Yu X, Zhang W, et al. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records. Lancet. 2020;395:809–15.
DeBolt CA, Bianco A, Limaye MA, Silverstein J, Penfield CA, Roman AS, et al. Pregnant women with severe or critical coronavirus disease 2019 have increased composite morbidity compared with nonpregnant matched controls. Am J Obstet Gynecol. 2021;224:510.
Gurol-Urganci I, Jardine JE, Carroll F, Draycott T, Dunn G, Fremeaux A, et al. Maternal and perinatal outcomes of pregnant women with SARS-CoV-2 infection at the time of birth in England: national cohort study. Am J Obstet Gynecol. 2021;225:522.
Villar J, Ariff S, Gunier RB, Thiruvengadam R, Rauch S, Kholin A, et al. Maternal and Neonatal Morbidity and Mortality Among Pregnant Women With and Without COVID-19 Infection: The INTERCOVID Multinational Cohort Study. JAMA Pediatr. 2021;175:817–26.
Lindsay L, Calvert C, Shi T, Carruthers J, Denny C, Donaghy J, et al. Neonatal and maternal outcomes following SARS-CoV-2 infection and COVID-19 vaccination: a population-based matched cohort study. Nat Commun. 2023;14:5275.
Faure-Bardon V, Isnard P, Roux N, Leruez-Ville M, Molina T, Bessieres B, et al. Protein expression of angiotensin-converting enzyme 2, a SARS-CoV-2-specific receptor, in fetal and placental tissues throughout gestation: new insight for perinatal counseling. Ultrasound Obstet Gynecol. 2021;57:242–7.
Letko M, Marzi A, Munster V. Functional assessment of cell entry and receptor usage for SARS-CoV-2 and other lineage B betacoronaviruses. Nat Microbiol. 2020;5:562–9.
Li M, Chen L, Zhang J, Xiong C, Li X. The SARS-CoV-2 receptor ACE2 expression of maternal-fetal interface and fetal organs by single-cell transcriptome study. PLoS One. 2020;15:e0230295.
Manjili RH, Zarei M, Habibi M, Manjili MH. COVID-19 as an Acute Inflammatory Disease. J Immunol. 2020;205:12–9.
Gappa M, Colin AA, Goetz I, Stocks J. Passive respiratory mechanics: the occlusion techniques. Eur Respir J. 2001;17:141–8.
McEvoy CT, Schilling D, Clay N, Jackson K, Go MD, Spitale P, et al. Vitamin C supplementation for pregnant smoking women and pulmonary function in their newborn infants: a randomized clinical trial. JAMA. 2014;311:2074–82.
McEvoy C, Venigalla S, Schilling D, Clay N, Spitale P, Nguyen T. Respiratory function in healthy late preterm infants delivered at 33-36 weeks of gestation. J Pediatr. 2013;162:464–9.
Dong Y, Mo X, Hu Y, Qi X, Jiang F, Jiang Z, et al. Epidemiology of COVID-19 Among Children in China. Pediatrics. 2020;16:e20200702.
Stoicescu ER, Iacob R, Iacob ER, Ghenciu LA, Oancea C, Manolescu DLTiny Lungs, Big Differences: Navigating the Varied COVID-19 Landscape in Neonates vs. Infants via Biomarkers and Lung Ultrasound. Biomedicines. 2024;12:425.
Doratt BM, Sureshchandra S, True H, Rincon M, Marshall NE, Messaoudi I Mild/asymptomatic COVID-19 in unvaccinated pregnant mothers impairs neonatal immune responses. JCI Insight. 2023;8:e172658.
Camporota L, Cronin JN, Busana M, Gattinoni L, Formenti F. Pathophysiology of coronavirus-19 disease acute lung injury. Curr Opin Crit Care. 2022;28:9–16.
Ozturk GK, Beken B, Dogan S, Akar HH. Pulmonary function tests in the follow-up of children with COVID-19. Eur J Pediatr. 2022;181:2839–47.
Ishqeir A NAAIGM. Increased Incidence of Persistent Pulmonary Hypertension of the Newborn Following Third Trimester Matrenal COVID-19 Infection. Eur Heart J. 2021. https://doi.org/10.1093/eurheartj/ehab724.1843.
Iovine E, Di MG, Nenna R, La Regina DP, Mancino E, Petrarca L, et al. Lung function after SARS-CoV-2 infection: A prospective cohort study in children. Pediatr Pulmonol. 2023;58:2009–16.
Rigby FB, Pastorek JG. Pneumonia during pregnancy. Clin Obstet Gynecol. 1996;39:107–19.
Benedetti TJ, Valle R, Ledger WJ. Antepartum pneumonia in pregnancy. Am J Obstet Gynecol. 1982;144:413–7.
Man OM, Azamor T, Cambou MC, Fuller TL, Kerin T, Paiola SG, et al. Respiratory distress in SARS-CoV-2 exposed uninfected neonates followed in the COVID Outcomes in Mother-Infant Pairs (COMP) Study. Nat Commun. 2024;15:399.
Wroblewska-Seniuk K, Basiukajc A, Wojciechowska D, Telge M, Miechowicz I, Mazela J. Clinical Characteristics of Newborns Born to Mothers with COVID-19. J Clin Med. 2021;10:4383.
Pawar R, Gavade V, Patil N, Mali V, Girwalkar A, Tarkasband V, et al. Neonatal Multisystem Inflammatory Syndrome (MIS-N) Associated with Prenatal Maternal SARS-CoV-2: A Case Series. Children. 2021;8:572.
Jordan BK, McEvoy CT. Trajectories of Lung Function in Infants and Children: Setting a Course for Lifelong Lung Health. Pediatrics. 2020;146:e20200417.
McEvoy CT, Spindel ER. Pulmonary Effects of Maternal Smoking on the Fetus and Child: Effects on Lung Development, Respiratory Morbidities, and Life Long Lung Health. Paediatr Respir Rev. 2017;21:27–33.
Owens L, Laing IA, Zhang G, Turner S, Le Souef PN. Airway function in infancy is linked to airflow measurements and respiratory symptoms from childhood into adulthood. Pediatr Pulmonol. 2018;53:1082–8.
Olsen SJ, Winn AK, Budd AP, Prill MM, Steel J, Midgley CM, et al. Changes in Influenza and Other Respiratory Virus Activity During the COVID-19 Pandemic - United States, 2020-2021. MMWR Morb Mortal Wkly Rep. 2021;70:1013–9.
Oregon Wildfire Response and Recovery-2020 Labor Day Wildfires After Action Report. 2024. https://wildfire-auth.oregon.gov/Documents/DMTF%20After%20Action%20Report.pdf
Goshen S, Novack L, Erez O, Yitshak-Sade M, Kloog I, Shtein A, et al. The effect of exposure to particulate matter during pregnancy on lower respiratory tract infection hospitalizations during first year of life. Environ Health. 2020;19:90.
Acknowledgements
The authors would like to thank the families who participated in this study and the neonatologists, obstetricians, neonatal fellows, and the staff of our Neonatal Intensive Care Unit for their help with the study.
Funding
Support from the Oregon Clinical and Translational Research Institute funded by grant UL1TR000128 from the National Center for Advancing Translational Sciences (CTM, KR) and the Pratt Family Foundation (KR).
Author information
Authors and Affiliations
Contributions
KR: Data collection, data interpretation, primary author, KDM: Assisted in drafting the manuscript, KP, DS & MO: PFT data collection, KM: Assisted in study design & data collection, SM: Statistical analysis, CM: Principle investigator, study design, data interpretation, assisted in drafting the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This study protocol was approved by the OHSU Institutional Review Board (IRB). Informed consent was obtained by the parent of each infant enrolled. This study was performed in accordance with the Declaration of Helsinki.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ruch, K., MacDonald, K.D., Parkhotyuk, K. et al. Neonatal pulmonary function tests in infants born to COVID-19 positive mothers. J Perinatol 45, 1431–1437 (2025). https://doi.org/10.1038/s41372-025-02237-w
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41372-025-02237-w