Abstract
Objective
To assess whether Family Integrated Care (FICare) model including Family-Centered Rounds (FCR) reduces parental stress in neonatal wards.
Study Design
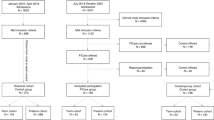
A multicenter, stepped-wedge cluster-randomized trial was conducted in ten level II neonatal wards in The Netherlands (March 2022–December 2023). Participants included parents of 613 infants hospitalized for ≥7 days. The primary outcome was parental stress at discharge (PSS:NICU scale). Secondary outcomes included parental participation, anxiety, trauma, depression, shared decision-making, and bonding.
Results
FICare significantly increased parental participation (P < 0.001) but did not reduce overall stress at discharge (FICare 61.2 vs. SNC 62.5, P = 0.21). Trauma symptoms in partners decreased (P = 0.03), and parents of transferred infants showed reduced stress (P = 0.01).
Conclusion
While FICare improved parental involvement, overall stress reduction was limited, with benefits seen in reduced trauma symptoms in partners and a reduction of stress in parents of transferred infants.
Trial registration
The trial has been registered at Clinical Trials.gov under registration number NCT05343403.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Flacking R, Lehtonen L, Thomson G, Axelin A, Ahlqvist S, Moran VH. et al. Closeness and separation in neonatal intensive care. Acta Paediatr. 2012;101:1032–7. https://pubmed.ncbi.nlm.nih.gov/22812674/.
Serlachius A, Hames J, Juth V, Garton D, Rowley S, Petrie KJ. Parental experiences of family-centred care from admission to discharge in the neonatal intensive care unit. J Paediatr Child Health. 2018;54:1227–33. https://pubmed.ncbi.nlm.nih.gov/29874396/.
Lasiuk GC, Comeau T, Newburn-Cook C. Unexpected: an interpretive description of parental traumas’ associated with preterm birth. BMC Pregnancy Childbirth. 2013. https://pubmed.ncbi.nlm.nih.gov/23445715/.
Karam F, Sheehy O, Huneau MC, Chambers C, Fraser WD, Johnson D. et al. Impact of maternal prenatal and parental postnatal stress on 1-year-old child development: results from the OTIS antidepressants in pregnancy study. Arch Womens Ment Health. 2016;19:835–43. https://pubmed.ncbi.nlm.nih.gov/26957509/.
Mclean MA, Scoten OC, Yu W, Ye XY, Petrie J, Church PT, et al. Lower maternal chronic physiological stress and better child behavior at 18 months: follow-up of a cluster randomized trial of Neonatal Intensive Care Unit Family Integrated Care. J Pediatrics. 2022;243:107–115.e4.
Woodward LJ, Bora S, Clark CAC, Montgomery-Hönger A, Pritchard VE, Spencer C. et al. Very preterm birth: maternal experiences of the neonatal intensive care environment. J Perinatol. 2014;34:555–61. https://pubmed.ncbi.nlm.nih.gov/24651730/.
Franck LS, Waddington C, O’Brien K. Family integrated care for preterm infants. Crit Care Nurs Clin North Am. 2020;32:149–65. https://pubmed.ncbi.nlm.nih.gov/32402313/.
Toivonen M, Lehtonen L, Löyttyniemi E, Ahlqvist-Björkroth S, Axelin A. Close Collaboration with Parents intervention improves family-centered care in different neonatal unit contexts: a pre-post study. Pediatr Res. 2020;88:421–8. https://pubmed.ncbi.nlm.nih.gov/32380505/.
O’Brien K, Bracht M, Robson K, Ye XY, Mirea L, Cruz M, et al. Evaluation of the Family Integrated Care model of neonatal intensive care: a cluster randomized controlled trial in Canada and Australia. BMC Pediatr. 2015;15:1–9. https://bmcpediatr.biomedcentral.com/articles/10.1186/s12887-015-0527-0.
O’Brien K, Robson K, Bracht M, Cruz M, Lui K, Alvaro R, et al. Effectiveness of Family Integrated Care in neonatal intensive care units on infant and parent outcomes: a multicentre, multinational, cluster-randomised controlled trial. Lancet Child Adolesc Health. 2018;2:245–54.
Church PT, Grunau RE, Mirea L, Petrie J, Soraisham AS, Synnes A, et al. Family integrated care (FICare): positive impact on behavioural outcomes at 18 months. Early Hum Dev. 2020;151. https://pubmed.ncbi.nlm.nih.gov/32987227/.
Voos KC, Ross G, Ward MJ, Yohay AL, Osorio SN, Perlman JM. Effects of implementing family-centered rounds (FCRs) in a neonatal intensive care unit (NICU). J Matern Fetal Neonatal Med. 2011;24:1403–6. https://pubmed.ncbi.nlm.nih.gov/21801140/.
Landry MA, Lafrenaye S, Roy MC, Cyr C. A randomized, controlled trial of bedside versus conference-room case presentation in a pediatric intensive care unit. Pediatrics. 2007;120:275–80. https://doi.org/10.1542/peds.2007-0107.
Barfield WD, Papile LA, Baley JE, Benitz W, Cummings J, Carlo WA, et al. Levels of neonatal care. Pediatrics. 2012;130:587–97. https://doi.org/10.1542/peds.2012-1999.
Hoeben H, Alferink MT, van Kempen AAMW, van Goudoever JB, van Veenendaal NR, van der Schoor SRD, et al. Collaborating to Improve Neonatal Care: ParentAl participation on the NEonatal ward-study protocol of the neoPARTNER Study. Children. 2023;10. http://www.ncbi.nlm.nih.gov/pubmed/37761442.
Hemming K, Taljaard M, McKenzie JE, Hooper R, Copas A, Thompson JA, et al. Reporting of stepped wedge cluster randomised trials: extension of the CONSORT 2010 statement with explanation and elaboration. BMJ. 2018;363. https://www.bmj.com/content/363/bmj.k1614.
Aftyka A, Rybojad B, Rosa W, Wróbel A, Karakuła-Juchnowicz H. Risk factors for the development of post-traumatic stress disorder and coping strategies in mothers and fathers following infant hospitalisation in the neonatal intensive care unit. J Clin Nurs. 2017;26:443645 https://pubmed.ncbi.nlm.nih.gov/28231614/.
van Veenendaal NR, van Kempen AAMW, Broekman BFP, et al. Association of a Zero-Separation Neonatal Care Model With Stress in Mothers of Preterm Infants. JAMA Netw Open. 2022;5:e224514. https://doi.org/10.1001/jamanetworkopen.2022.4514.
Prouhet PM, Gregory MR, Russell CL, Yaeger LH. Fathers’ stress in the neonatal intensive care unit: a systematic review. Adv Neonatal Care. 2018;18:105–20. https://journals.lww.com/advancesinneonatalcare/fulltext/2018/04000/fathers__stress_in_the_neonatal_intensive_care.7.aspx.
Schappin R, Wijnroks L, Uniken Venema MMAT, Jongmans MJ. Rethinking stress in parents of preterm infants: a meta-analysis. PLoS ONE. 2013;8:e54992 https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0054992.
R Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. 2021. https://www.scirp.org/reference/referencespapers?referenceid=3131254.
van Buuren S, Groothuis-Oudshoorn K. mice: multivariate imputation by chained equations in R. J Stat Softw. 2011;45:1–67. https://www.jstatsoft.org/index.php/jss/article/view/v045i03.
Bates D, Mächler M, Bolker BM, Walker SC. Fitting linear mixed-effects models using lme4. J Stat Softw. 2015;67:1–48. https://doi.org/10.18637/jss.v067.i01.
Benzies KM, Aziz K, Shah V, Faris P, Isaranuwatchai W, Scotland J. et al. Effectiveness of Alberta Family Integrated Care on infant length of stay in level II neonatal intensive care units: a cluster randomized controlled trial. BMC Pediatr. 2020;20:1–11. https://bmcpediatr.biomedcentral.com/articles/10.1186/s12887-020-02438-6.
Zhang Y, Jiang M, Wang S, Xiang X, He W, Du J, et al. Effect of family integrated care on stress in mothers of preterm infants: A multicenter cluster randomized controlled trial. J Affect Disord. 2024;350:304–12.
Van Veenendaal NR, Van Der Schoor SRD, Broekman BFP, De Groof F, Van Laerhoven H, Van Den Heuvel MEN, et al. Association of a family integrated care model with paternal mental health outcomes during neonatal hospitalization. JAMA Netw Open. 2022;5:E2144720.
van Wyk L, Majiza AP, Ely CSE, Singer LT. Psychological distress in the neonatal intensive care unit: a meta-review. Pediatr Res. 2024;96:1510 https://pmc.ncbi.nlm.nih.gov/articles/PMC11624136/.
Alferink MT, Moreno-Sanz B, Cabrera-Lafuente M, Ergenekon E, de Haan TR, van Kempen AAMW, et al. RISEinFAMILY project: the integration of families at neonatal intensive care units (NICUs) to empower them as primary caregivers: study protocol for a stepped wedge cluster controlled trial. Trials. 2024;25. https://pubmed.ncbi.nlm.nih.gov/38594733/.
Labrie NHM, van Veenendaal NR, Ludolph RA, Ket JCF, van der Schoor SRD, van Kempen AAMW. Effects of parent-provider communication during infant hospitalization in the NICU on parents: a systematic review with meta-synthesis and narrative synthesis. Patient Educ Couns. 2021;104:1526–52. https://pubmed.ncbi.nlm.nih.gov/33994019/.
Acknowledgements
We would like to thank Jos W.R. Twisk (Prof, Department of Biostatistics and Epidemiology, VU, Amsterdam, the Netherlands) for his guidance on epidemiologic questions, as well as James P. Hughes (Prof, Department of Biostatistics, University of Washington, United States) for specific expertise in the design of this trial. We also extend our gratitude to Nanon H.M. Labrie (mother of a preterm infant born at 26 weeks of gestation, PhD) and Sylvia A. Obermann-Borst (mother of a preterm infant born at 29 weeks of gestation and Scientific Coordinator at Care4Neo, Dutch parent and patient support group, MD, PhD) for their valuable insights from a parent’s perspective. We are also deeply grateful to our lead researchers (Ron H.T. van Beek, Lotte H. Hendrikx, Claire A.M. Lutterman, Angelique K.E. Hoffman-Haringsma, Anne M. de Grauw, Ageeth G. Kaspers, Femke de Groof, Martijn J.M. van Brakel, Maarten Rijpert, Fenna Visser) and their research assistants for their dedication and commitment to the implementation of FICare and the inclusion of participants.
Funding
This study was supported by SPIN, the General Paediatrics Research Network of the Dutch Association for Paediatrics, supported by het Cultuurfonds.
Author information
Authors and Affiliations
Consortia
Contributions
Conceptualisation, methodology, validation and resources: MTA, HH, AAMWvK, JBvG, NRvV, and SRDvdS; software: M.T.A., HH, NHJ and SRDvdS; Data curation: MTA, HH; formal analysis: MTA, HH, NHJ; investigation: MTA, HH, NRvV, and SRDvdS; writing—original draft preparation: MTA, HH, NHJ and SRDvdS; writing—review and editing: HH, MTA, NHJ, AAMWvK, JBvG, SRDvdS and NRvV; visualization: MTA, HH; supervision: AAMWvK, JBvG, and SRDvdS; project administration: MTA, HH, and SRDvdS; funding acquisition: HH and SRDvdS; MTA and HH contributed equally as first authors. Members of the neoPARTNER study group contributed to patient recruitment, data collection, and provision of laboratory samples. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
Ethical approval by the Medical Ethics Review Committee (MEC-U, Nieuwegein, The Netherlands) was received on 6 December 2021. All methods were performed in accordance with the relevant guidelines and regulations. Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Alferink, M.T., Hoeben, H., Jonkman, N.H. et al. Family integrated care reduces stress in transferred parents of preterm infants, but not across all families: a stepped-wedge cluster-randomized trial. J Perinatol 45, 797–805 (2025). https://doi.org/10.1038/s41372-025-02318-w
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41372-025-02318-w