Abstract
Retinopathy of Prematurity (ROP) remains a worldwide problem. A more complete understanding of the pathogenesis might inform progress toward its elimination. ROP pathogenesis is undeniably complex, including preterm birth and oxygen exposure, but many other factors are implicated as well. In this Perspective, we focus on two pathogenic factors that are within the domain of neonatal hematology and transfusion medicine. Specifically, we address evidence that ROP pathogenesis can involve: 1) an elevated nucleated red blood cell (NRBC) count at preterm birth, as evidence of chronic hypoxia in utero, which should be recognized as a biomarker of elevated risk for developing ROP; and 2) transfusions of adult donor red blood cells (RBC) result in a dose-dependent elevation in adult hemoglobin (HbA), which can deliver and release excessive oxygen to the developing retina. Early studies indicate that eliminating adult donor RBC transfusions for vulnerable preterm infants might reduce or eliminate ROP.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
Inquiries regarding data access can be addressed to the corresponding author.
References
Hartnett ME. Pathophysiology of retinopathy of prematurity. Annu Rev Vis Sci. 2023;9:39–70.
Hartnett ME. Pathophysiology and mechanisms of severe retinopathy of prematurity. Ophthalmology. 2015;122:200–10.
García H, Villasis-Keever MA, Zavala-Vargas G, Bravo-Ortiz JC, Pérez-Méndez A, Escamilla-Núñez A. Global prevalence and severity of retinopathy of prematurity over the last four decades (1985-2021): A systematic review and meta-analysis. Arch Med Res. 2024;55:102967.
Chiang MF, Quinn GE, Fielder AR, Ostmo SR, Paul Chan RV, Berrocal A, et al. International classification of retinopathy of prematurity, Third Edition. Ophthalmology. 2021;128:e51–e68.
Dammann O, Hartnett ME, Stahl A. Retinopathy of prematurity. Dev Med Child Neurol. 2023;65:625–31.
Almutairi M, Chechalk K, Deane E, Fox R, Janes A, Maguire-Henry T, et al. Biomarkers in retinopathy of prematurity: a systematic review and meta-analysis. Front Pediatr. 2024;12:1371776.
Darlow BA, Vento M, Beltempo M, Lehtonen L, Håkansson S, Reichman B, et al. International Network for Evaluating Outcomes (iNeo) of Neonates. Variations in oxygen saturation targeting, and retinopathy of prematurity screening and treatment criteria in neonatal intensive care units: an international survey. Neonatology. 2018;114:323–31.
Chen ML, Guo L, Smith LE, Dammann CE, Dammann O. High or low oxygen saturation and severe retinopathy of prematurity: a meta-analysis. Pediatrics. 2010;125:e1483–92.
Tolsma KW, Allred EN, Chen ML, Duker J, Leviton A, Dammann O. Neonatal bacteremia and retinopathy of prematurity: the ELGAN study. Arch Ophthalmol. 2011;129:1555–63.
Dammann O, Stansfield BK. Neonatal sepsis as a cause of retinopathy of prematurity: An etiological explanation. Prog Retin Eye Res. 2024;98:101230.
Fevereiro-Martins M, Guimarães H, Marques-Neves C, Bicho M. Retinopathy of prematurity: contribution of inflammatory and genetic factors. Mol Cell Biochem. 2022;477:1739–63.
Li X, Owen LA, Taylor KD, Ostmo S, Chen YI, Coyner AS. i-ROP Consortium. Genome-wide association identifies novel ROP risk loci in a multiethnic cohort. Commun Biol. 2024;7:107.
Kim ES, Calkins KL, Chu A. Retinopathy of prematurity: the role of nutrition. Pediatr Ann. 2023;52:e303–8.
Wu PY, Fu YK, Lien RI, Chiang MC, Lee CC, Chen HC, et al. Systemic cytokines in retinopathy of prematurity. J Pers Med. 2023;13:291.
Cakir B, Liegl R, Hellgren G, Lundgren P, Sun Y, Klevebro S, et al. Thrombocytopenia is associated with severe retinopathy of prematurity. JCI Insight. 2018;3:e99448.
Seliniotaki AK, Haidich AB, Moutzouri S, Lithoxopoulou M, Ziakas N, Lundgren P, et al. Association of platelet deficiency with severe retinopathy of prematurity: a review. Acta Paediatr. 2022;111:2056–70.
Dammann O, Brinkhaus MJ, Bartels DB, Dördelmann M, Dressler F, Kerk J, et al. Immaturity, perinatal inflammation, and retinopathy of prematurity: a multi-hit hypothesis. Early Hum Dev. 2009;85:325–9.
Dammann O, Rivera JC, Chemtob S. The prenatal phase of retinopathy of prematurity. Acta Paediatr. 2021;110:2521–8.
Strawbridge JC, Chu A, Dammann O, Hanson J, Janzen C, Tsui I. Prenatal maternal characteristics associated with retinopathy of prematurity. Retina. 2023;43:230–7.
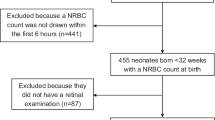
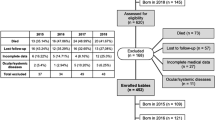
Lubetzky R, Stolovitch C, Dollberg S, Mimouni FB, Salomon M, Mandel D. Nucleated red blood cells in preterm infants with retinopathy of prematurity. Pediatrics. 2005;116:e619–22.
Christensen RD, Henry E, Andres RL, Bennett ST. Reference ranges for blood concentrations of nucleated red blood cells in neonates. Neonatology. 2011;99:289–94.
Niranjan HS, Bharath Kumar Reddy KR, Benakappa N, Murthy K, Shivananda S, Veeranna V. Role of hematological parameters in predicting retinopathy of prematurity (ROP) in preterm neonates. Indian J Pediatr. 2013;80:726–30.
Gotru S, Ahlers-Schmidt CR, Delmore P, Shaw J, Bloom BT. The absolute nucleated red blood cell (aNRBC) count at birth is not an indicator for retinopathy of prematurity (ROP). J Perinatol. 2013;33:21–4.
Lubetzky R, Mandel D, Mimouni FB. Absolute nucleated red blood cell count and retinopathy of prematurity (ROP). J Perinatol. 2013;33:579–80.
Fevereiro-Martins M, Santos AC, Marques-Neves C, Guimarães H, Bicho M. GenE-ROP Study Group. Complete blood count parameters as biomarkers of retinopathy of prematurity: a Portuguese multicenter study. Graefes Arch Clin Exp Ophthalmol. 2023;261:2997–3006.
Widness JA, Schmidt RL, Sawyer ST. Erythropoietin transplacental passage—review of animal studies. J Perinat Med. 1995;23:61–70.
Christensen RD Nucleated red blood cells in neonatal medicine. In Hematology and Transfusion Medicine. 4th edition, Ohls RK, Maheshwari A, Christensen RD, eds. Elsevier, Philadelphia 2024, 27-38.
Quigley JG, Means RT Jr, Glader B The birth, and death of red blood cells: erythropoiesis, the mature red blood cells, and cell destruction. In Wintrobe’s Clinical Hematology, 15th Edition, Means Jr RT, Rodgers GM, Glader B, Arber DA, Appelbaum RF, Dispenzieri A, Fehnigher TA, Michaelis L, and Leonard JP eds, Worters Kluwer, Philadelphia, 2024. 102–3.
Bahr TM, Henry E, O’Brien EA, Christensen RD. Nucleated red blood cell counts of neonates born emergently 1-4 h after a maternal cardiac arrest. Neonatology. 2022;119:255–9.
Bahr TM, Albertine KH, Christensen RD, Dahl MJ, Rebentisch A, Dawson E, et al. Nucleated red blood cell emergence-time in newborn lambs following a dose of darbepoetin alfa. Curr Pediatr Rev. 2023;19:425–8.
Christensen RD, Lambert DK, Richards DS. Estimating the nucleated red blood cell ‘emergence time’ in neonates. J Perinatol. 2014;34:116–9.
Cremer M, Roll S, Gräf C, Weimann A, Bührer C, Dame C. Nucleated red blood cells as a marker for an increased risk of unfavorable outcome and mortality in very low birth weight infants. Early Hum Dev. 2015;91:559–63.
Bahr TM, Ohls RK, Baserga MC, Lawrence SM, Winter SL, Christensen RD. Implications of an elevated nucleated red blood cell count in neonates with moderate to severe hypoxic-ischemic encephalopathy. J Pediatr. 2022;246:12–18.e2.
Clark C, Gibbs JAH, Maniello R, Peterbridge EW, Aranda JV. Blood transfusion: a possible risk factor in retrolental fibroplasia. Acta Pediatr Scand. 1981;70:535.
Shohat M, Reisner SH, Krikler R, Nissenkorn I, Yassur Y, Ben-Sira I. Retinopathy of prematurity: incidence and risk factors. Pediatrics. 1983;72:159–60.
Hesse L, Eberl M, Schlaud C, Poets F. Blood transfusion. Iron load and retinopathy of prematurity. Eur J Pediatr. 1997;156:465–370.
Cooke RW, Clark D, Nickey-Dwyer M, Weindling AM. The apparent role of blood transfusion in the development of retinopathy of prematurity. Eur J Pediatr. 1993;152:833–6.
Inder TE, Clemett RS, Austin NC, Graham P, Darlow BA. High iron status in very low birth weight infants is associated with an increased risk of retinopathy of prematurity. J Pediatr. 1997;131:541–4.
Collard KJ. Transfusion related morbidity in premature babies: Possible mechanisms and implications for practice. World J Clin Pediatr. 2014;3:19–29.
Lust C, Vesoulis A, Jackups R Jr, Liao S, Rao R, Mathur AM. Early red cell transfusion is associated with the development of severe retinopathy of prematurity. J Perinatol. 2019;39:393–400.
Dani C, Reali MF, Bertini G, Martelli E, Pezzati M, Rubaltelli FF. The role of blood transfusions and iron intake on retinopathy of prematurity. Early Hum Dev. 2001;62:57–63.
Del Vecchio A, Henry E, D’Amato G, Cannuscio A, Corriero L, Motta M, et al. Instituting a program to reduce the erythrocyte transfusion rate was accompanied by reductions in the incidence of bronchopulmonary dysplasia, retinopathy of prematurity and necrotizing enterocolitis. J Matern Fetal Neonatal Med. 2013;26:77–9.
Stutchfield CJ, Jain A, Odd D, Williams C, Markham R. Foetal haemoglobin, blood transfusion, and retinopathy of prematurity in very preterm infants: a pilot prospective cohort study. Eye (Lond). 2017;31:1451–5.
Zhu Z, Hua X, Yu Y, Zhu P, Hong K, Ke Y. Effect of red blood cell transfusion on the development of retinopathy of prematurity: A systematic review and meta-analysis. PLoS One. 2020;15:e0234266.
Hengartner T, Adams M, Pfister RE, Snyers D, McDougall J, Waldvogel S, et al. Swiss Neonatal Network. Associations between red blood cell and platelet transfusions and retinopathy of prematurity. Neonatology. 2020;117:1–7.
Dani C, Coviello C, Panin F, Frosini S, Costa S, Purcaro V, et al. Incidence and risk factors of retinopathy of prematurity in an Italian cohort of preterm infants. Ital J Pediatr. 2021;47:64.
Teofili L, Papacci P, Bartolo M, Molisso A, Orlando N, Pane L, et al. Transfusion-free survival predicts severe retinopathy in preterm neonates. Front Pediatr. 2022;10:814194.
Raffa LH, Aljohani W. Evaluation of the effect of blood transfusion on retinopathy of prematurity at a tertiary care center in western Saudi Arabia. Cureus. 2022;14:e24495.
Teofili L, Papacci P, Orlando N, Bianchi M, Pasciuto T, Mozzetta I, et al. BORN study: a multicenter randomized trial investigating cord blood red blood cell transfusions to reduce the severity of retinopathy of prematurity in extremely low gestational age neonates. Trials. 2022;23:1010.
Prasad N, Dubey A, Kumar K, Shrivastava J. Role of fetal hemoglobin in the development and progression of retinopathy of prematurity in preterm infants. Indian J Ophthalmol. 2023;71:3478–83.
Glaser K, Härtel C, Dammann O, Herting E, Andres O, Speer CP, et al. German Neonatal Network. Erythrocyte transfusions are associated with retinopathy of prematurity in extremely low gestational age newborns. Acta Paediatr. 2023;112:2507–15.
Torrejon-Rodriguez L, Pinilla-Gonzalez A, Lara Cantón I, Albiach-Delgado A, Cascant-Vilaplana MM, Cernada M, et al. Effect of autologous umbilical cord blood transfusion in the development of retinopathy of prematurity: randomized clinical trial - study protocol. Front Pediatr. 2023;11:1269797.
Pellegrino C, Papacci P, Beccia F, Serrao F, Cantone GV, Cannetti G, et al. Differences in cerebral tissue oxygenation in preterm neonates receiving adult or cord blood red cell transfusions. JAMA Netw Open. 2023;6:e2341643.
Teofili L, Papacci P, Dani C, Cresi F, Remaschi G, Pellegrino C, et al. Cord blood transfusions in extremely low gestational age neonates to reduce severe retinopathy of prematurity: results of a prespecified interim analysis of the randomized BORN trial. Ital J Pediatr. 2024;50:142.
El Emrani S, van der Meeren LE, Lopriore E, Schalij‐Delfos NE. Erythrocyte transfusions and retinopathy of prematurity: plea for application of the two‐phase theory. Acta Paediatrica. 2024;113:615–6.
Wang X, Rao R, Li H, Lei X, Dong W. Red blood cell transfusion for incidence of retinopathy of prematurity: prospective multicenter cohort study. JMIR Pediatr Parent. 2024;7:e60330.
Fevereiro-Martins M, Santos AC, Marques-Neves C, Bicho M, Guimarães H. On Behalf Of The GenE-Rop Study Group. Retinopathy of prematurity in eight Portuguese neonatal intensive care units: incidence, risk factors, and progression-a prospective multicenter study. Child (Basel). 2024;11:1154.
Fevereiro-Martins M, Aguiar L, Inácio Â, Cardoso C, Santos AC, Marques-Neves C, et al. GenE-ROP Study Group. Fetal hemoglobin as a predictive biomarker for retinopathy of prematurity: a prospective multicenter cohort study in Portugal. Biomedicines. 2025;13:110.
El Emrani S, Derks LA, Tjiam AM, van Bohemen M, Termote JUM, van der Meeren LE, et al. The association between red blood cell transfusion timing and the development of retinopathy of prematurity: Application of the two-phase theory. Acta Ophthalmol. 2025. https://doi.org/10.1111/aos.17471.
Querol S, Rocha V, Ruggeri A Procurement and Management of Cord Blood Unit for Allogeneic Transplantation. 2024 Apr 11. In: Sureda A, Corbacioglu S, Greco R, Kröger N, Carreras E, editors. The EBMT Handbook: Hematopoietic Cell Transplantation and Cellular Therapies [Internet]. 8th ed. Cham (CH): Springer; 2024. Chapter 18.
Christensen RD, Bahr TM, Christensen TR, Ohls RK, Krong J, Carlton LC, et al. Banked term umbilical cord blood to meet the packed red blood cell transfusion needs of extremely low-gestational-age neonates: a feasibility analysis. J Perinatol. 2024;44:873–9.
Bahr TM, Christensen TR, Ilstrup SJ, Ohls RK, Christensen RD. Term umbilical cord blood, fully tested and processed, as the source of red blood cell transfusions for extremely-low-gestational age neonates. Semin Fetal Neonatal Med. 2025;30:101546.
Christensen RD, Lambert DK, Baer VL, Montgomery DP, Barney CK, Coulter DM, et al. Postponing or eliminating red blood cell transfusions of very low birth weight neonates by obtaining all baseline laboratory blood tests from otherwise discarded fetal blood in the placenta. Transfusion. 2011;51:253–8.
Carroll PD, Nankervis CA, Iams J, Kelleher K. Umbilical cord blood as a replacement source for admission complete blood count in premature infants. J Perinatol. 2012;32:97–102.
Baer VL, Lambert DK, Carroll PD, Gerday E, Christensen RD. Using umbilical cord blood for the initial blood tests of VLBW neonates results in higher hemoglobin and fewer RBC transfusions. J Perinatol. 2013;33:363–5.
Carroll PD, Livingston E, Baer VL, Karkula K, Christensen RD. Evaluating otherwise-discarded umbilical cord blood as a source for a neonate’s complete blood cell count at various time points. Neonatology. 2018;114:82–6.
Bahr TM, Carroll PD. Cord blood sampling for neonatal admission laboratory testing-an evidence-based blood conservation strategy. Semin Perinatol. 2023;47:151786.
Tweddell SM, Morelli TM, Bahr TM, Krueger A, Christensen RD, Ohls RK Identifying barriers to complying with new restrictive NICU transfusion guidelines. J Perinatol. 2025. https://doi.org/10.1038/s41372-025-02225-0. Epub ahead of print.
Ohls RK, Bahr TM, Peterson TG, Christensen RD. A practical guide to reducing/eliminating red blood cell transfusions in the neonatal intensive care unit. Semin Fetal Neonatal Med. 2025;30:101546.
Bahr TM, Christensen RD, Weaver-Lewis KA, Scott DM, Gerday E, Tuttle JJ, et al. A prospective randomized pilot trial comparing weekly vs. biweekly Darbepoetin administration to preterm infants. J Perinatol. 2025 Mar. https://doi.org/10.1038/s41372-025-02247-8. Epub ahead of print.
Christensen RD, Bahr TM, Ohls RK. Administering supplemental iron and erythropoiesis-stimulating agents to infants born preterm: what do we need to build consensus? J Pediatr. 2025;279:114460.
Bahr TM, Ohls RK, Christensen RD. Treating preterm infants with erythropoietin does not increase the risk of retinopathy of prematurity. J Perinatol. 2025;45:292–3.
Ohls RK, Das A, Tan S, Lowe JR, Schibler K, Beauman SS, et al. Darbepoetin, red cell mass, and neuroprotection in preterm infants: a randomized clinical trial. JAMA Pediatr. 2025;12(May):e250807.
Becker S, Wang H, Yu B, Brown R, Han X, Lane RH, et al. Protective effect of maternal uteroplacental insufficiency on oxygen-induced retinopathy in offspring: removing bias of premature birth. Sci Rep. 2017;7:42301.
Fung C, Cung T, Nelson C, Wang H, Bretz C, Ramshekar A, et al. Retinopathy of prematurity protection conferred by uteroplacental insufficiency through erythropoietin signaling in an experimental murine model. Pediatr Res. 2023;94:950–5.
Pellegrino C, Stone EF, Valentini CG, Teofili L. Fetal red blood cells: A comprehensive review of biological properties and implications for neonatal transfusion. Cells. 2024;13:1843.
Author information
Authors and Affiliations
Contributions
Conceptualization, RDC, TB, SJI, MEH, and RKO. Methodology, RDC, TM, SJI, MEH, and RKO. Original Draft Preparation, RDC. Review and Editing, RDC, TM, SJI, MEH, and RKO.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Christensen, R.D., Bahr, T.M., Ilstrup, S.J. et al. Involving neonatal hematology and transfusion medicine in global efforts to eliminate severe retinopathy of prematurity. J Perinatol 45, 1839–1847 (2025). https://doi.org/10.1038/s41372-025-02368-0
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41372-025-02368-0