Abstract
Objective
Evaluate earlier intervention on short- and longer-term outcomes in preterm infants with post-hemorrhagic ventricular dilatation (PHVD) born at ≤32 weeks’ gestation.
Study design
Retrospective, multi-center, observational study.
Results:
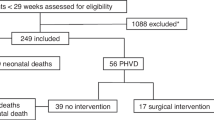
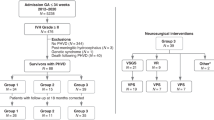
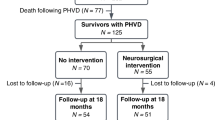
One hundred patients met eligibility criteria. Of 70 survivors, PHVD resolved spontaneously in 32 (46%). The 38 infants needing intervention were managed with: lumbar puncture (LP) alone (n = 23, 60%); LP and ventricular access device (VAD) only (n = 6, 16%); LP, VAD, ventricular-peritoneal shunt (n = 9, 24%). There were no differences in incidence of cerebral palsy or Bayley Scales of Infant and Toddler Development (BSID-III) composite score between the intervention and non-intervention group (p > 0.5). Neurosurgical intervention was initiated at smaller ventricle size and BSID-III scores improved significantly compared to a historical cohort with late intervention, (p < 0.05).
Conclusion
Initiation of early intervention for PHVD was feasible and was associated with improved neurodevelopmental outcomes compared to late intervention.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The datasets and materials used or analysed during this study are available from the corresponding author on request.
References
Afifi J, Leijser LM, de Vries LS, Shah PS, Mitra S, Brouwer MJ, et al. Variability in the diagnostic and management practices of post-hemorrhagic ventricular dilatation in very preterm infants across Canadian centers and comparison with European practices. J Neonatal Perinat Med. 2022;15:721–9. https://www.ncbi.nlm.nih.gov/pubmed/36463462.
El-Dib M, Limbrick D, Inder TWA, Kulkarni A, Warf B, Volpe J, et al. Management of post-hemorrhagic ventricular dilatation in the infant born preterm. J Pediatr. 2020;226:16–27.
Pinto C, Malik P, Desai R, Shelar V, Bekina-Sreenivasan D, Satnarine TA, et al. Post-hemorrhagic hydrocephalus and outcomes amongst neonates with intraventricular hemorrhage: a systematic review and pooled analysis. Cureus. 2021;13:e18877. https://www.ncbi.nlm.nih.gov/pubmed/34804726.
Leijser L, Miller S, Wezel-Meijler van, G Brouwer A, Traubici, J’ van Haastert I, et al. Posthemorrhagic ventricular dilatation in preterm infants: When best to intervene? Neurology. 2018;91:e1–9.
Cizmeci M, Groenendaal F, Liem K, van Haastert I, Benavente-Fernandez I, van Straaten H, et al. Randomized controlled early versus late ventricular intervention study in post hemorrhagic ventricular dilatation: outcome at 2 years. J Pediatr. 2020;226:28–35.
de Vries LS, Liem KD, Van Dijk K, Smit BJ, Sie L, Rademaker KJ, et al. Early versus late treatment of posthaemorrhagic venticular dilatation: results of a retrospective study from five neonatal intensive care units in The Netherlands. Acta Paediatr. 2007;91:212–7.
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inf. 2009;42:377–81. https://linkinghub.elsevier.com/retrieve/pii/S1532046408001226.
Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inf. 2019;95:103208. https://linkinghub.elsevier.com/retrieve/pii/S1532046419301261.
Leijser LM, Scott JN, Roychoudhury S, Zein H, Murthy P, Thomas SP, et al. Post- hemorrhagic ventricular dilatation: inter-observer reliability of ventricular size measurements in extremely preterm infants. Pediatr Res. 2021;90:403–10. https://www.ncbi.nlm.nih.gov/pubmed/33184496.
Davies MW, Swaminathan M, Chuang SL, Betheras FR. Reference ranges for the linear dimentions of the intracranial ventricles in preterm neonates. ADC Fetal Neonatal Ed. 2000;82:F218–23.
Mohammad K, Scott J, Leijser L, Zein H, Afifi J, Piedboeuf B, et al. Consensus approach for standardizing the screening and classification of preterm brain injury diagnosed with cranial ultrasound: a Canadian perspective. Front Pediatr. 2021;9:618236
Bayley N. Bayley’s scales of infant and toddler development. 3rd ed. San Antonio, TX: Harcourt Assessment; 2006.
Hendson L, Church PT, Banihani R. Follow-up care of the extremely preterm infant after discharge from the neonatal intensive care unit. Paediatr Child Health. 2022;27:359–64.
Maitre N, Burton V, Duncan A, Iyer S, Ostrander B, Winter S. Network implementation of guideline for early detection decreases age at cerebral palsy diagnosis. Pediatrics. 2020;145. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC7193973/.
Palisano R, Rosenbaum P, Walter S, Russell D, Wood E, Galuppi B. Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev Med Child Neurol. 1997;39:214–23.
Shankaran S, Bajaj M, Natarajan G, Saha S, Pappas A, Davis AS, et al. Outcomes following post-hemorrhagic ventricular dilatation among infants of extremely low gestational age. J Pediatr. 2020;226:36–44 e3. https://www.ncbi.nlm.nih.gov/pubmed/32739261.
Sewell E, Cohen S. Surgical interventions and short term outcomes for preterm infants with post haemorrhagic hydrocephalus: a multicenter cohort study. Arch Disease Child Fetal Neonatal Ed. 2024;110:10–16
Badhiwala JH, Hong CJ, Nassiri F, Hong BY, Riva-Cambrin J, Kulkarni AV.Treatment of posthemorrhagic ventricular dilation in preterm infants: a systematic review and meta-analysis of outcomes and complications. J Neurosurg Pediatr. 2015;16:545–55. https://thejns.org/view/journals/j-neurosurg-pediatr/16/5/article-p545.xml.
de Vries L, Groenendaal F, Liem K, Heep A, Brouwer A, ’tVerlaat van, et al. Treatment thresholds for intervention in posthaemorrhagic ventricular dilation: a randomized controlled trial. Arch Disease Child Fetal Neonatal Ed. 2019;104:F70–5.
Beltempo M, Shah P, Yoon E, Goswami N. Canadian Neonatal Network, Annual Report 2022. Toronto: Canadian Neonatal Network; 2022.
Cizmeci MN, de Vries L, Ly LG, van Haastert MA, Groenendaal F, Kelly EN, et al. Periventricular hemorrhagic infarction in very preterm infants: characteristic sonographic findings and association with neurodevelopmental outcome at age 2 years. J Pediatr. 2020;217:79–85.
Limbrick DD Jr, de Vries LS. New insights into the management of post- hemorrhagic hydrocephalus. Semin Perinatol. 2022;46:151597. https://www.ncbi.nlm.nih.gov/pubmed/35461702.
Holwerda JC, Van Braeckel K, Roze E, Hoving EW, Maathuis CGB, Brouwer OF, et al. Functional outcome at school age of neonatal post-hemorrhagic ventricular dilatation. Early Hum Dev. 2016;96:15–20. https://www.ncbi.nlm.nih.gov/pubmed/26986627.
Acknowledgements
We thank the Neonatal Nurse Practitioners in the NICU at the Hospital for Sick Children for their meticulous ongoing care of many fragile patients with VAD who require daily reservoir taps, often for many months. We are grateful to the Neonatal Neurodevelopmental Follow Up teams at SickKids, Mount Sinai and Sunnybrook Hospital for completing BSID-III testing during the global pandemic.
Author information
Authors and Affiliations
Contributions
D.W. designed the protocol, the data collection instrument, collated the data from participating centers, carried out the initial data analysis and drafted the manuscript, reviewed and revised the manuscript. S.B., A.K., L. Leijser, and L.Ly designed the protocol and data collection instrument, critically analyzed the data and aided in the interpretation of the results and reviewed and revised the manuscript. L.D., E.K., K.R., S.W., and E.A. collected data at their participating centers and critically reviewed the manuscript. Y.D., E.N., P.C., and S.M. conceptualized the study, aided in the interpretation of the results and critically reviewed the manuscript. P.G., D.K., and J.T. reviewed the protocol and provided feedback specific to interpretation of cUS findings and critically reviewed the manuscript. M.C. aided in the interpretation of the results and critically reviewed the manuscript. RP assisted with the development of the REDCap data collection tool and assisted with co-ordination of REB approvals.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
Research Ethics Board approval was obtained from Clinical Trials Ontario (Study ID 3226). Parental consent was not obtained as this was considered an evidence-based change in practice. This study was performed in accordance with the Declaration of Helsinki.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wilson, D., Breitbart, S., DiFonzo, L. et al. Implementation of an early intervention strategy for post hemorrhagic ventricular dilatation in preterm infants. J Perinatol (2025). https://doi.org/10.1038/s41372-025-02371-5
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41372-025-02371-5