Abstract
Objective
To investigate the impact of hyperglycemia on the neurodevelopmental outcomes in extremely preterm infants.
Study design
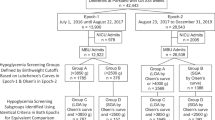
This single-center retrospective cohort study enrolled extremely preterm infants born at <28 weeks of gestation. Hyperglycemia was defined as a blood glucose level of >15 mmol/L. The Kyoto Scale of Psychological Development at 18 months of corrected age was used for neurodevelopmental assessment, and a developmental quotient (DQ) of ≥85 was defined as normal.
Results
Among the 102 surviving extremely preterm infants, 54 (53%) had hyperglycemia. The hyperglycemia group had lower DQ (81.0 ± 19.3 vs. 91.1 ± 15.3, P < 0.01) and decreased normal DQ rate (37% vs. 75%, P < 0.001). In the multiple logistic regression models, hyperglycemia was significantly associated with lower normal DQ rates (P = 0.03).
Conclusion
Hyperglycemia, defined as a blood glucose level of >15 mmol/L, was independently negatively associated with normal DQ after adjusting for confounders.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
All datasets generated or analyzed during the current study are available from the corresponding author upon reasonable request.
References
Meetze W, Bowsher R, Compton J, Moorehead H. Hyperglycemia in extremely- low-birth-weight infants. Biol Neonate. 1998;74:214–21.
Salis ER, Reith DM, Wheeler BJ, Broadbent RS, Medlicott NJ. Insulin resistance, glucagon-like peptide-1 and factors influencing glucose homeostasis in neonates. Arch Dis Child Fetal Neonatal Ed. 2017;102:F162–f6.
Blanco CL, Baillargeon JG, Morrison RL, Gong AK. Hyperglycemia in extremely low birth weight infants in a predominantly Hispanic population and related morbidities. J Perinatol. 2006;26:737–41.
Zamir I, Tornevi A, Abrahamsson T, Ahlsson F, Engström E, Hallberg B, et al. Hyperglycemia in extremely preterm infants-insulin treatment, mortality and nutrient intakes. J Pediatr. 2018;200:104–10.e1.
Inage Y, Hirano D, Nakagawa A, Yamada S, Kotake Y, Ikoma N, et al. Risk factors for hyperglycemia in extremely low birth weight infants during the first 14 days. Pediatrics Neonatol. 2022;63:13–8.
Stensvold HJ, Strommen K, Lang AM, Abrahamsen TG, Steen EK, Pripp AH, et al. Early enhanced parenteral nutrition, hyperglycemia, and death among extremely low-birth-weight infants. JAMA Pediatrics. 2015;169:1003.
Auerbach A, Eventov-Friedman S, Arad I, Peleg O, Bdolah-Abram T, Bar-Oz B, et al. Long duration of hyperglycemia in the first 96 h of life is associated with severe intraventricular hemorrhage in preterm infants. J Pediatr. 2013;163:388–93.
Gonzalez Villamizar JD, Haapala JL, Scheurer JM, Rao R, Ramel SE. Relationships between Early Nutrition, Illness, and Later Outcomes among Infants Born Preterm with Hyperglycemia. J Pediatr. 2020;223:29–33.e2.
Kermorvant-Duchemin E, Pinel AC, Lavalette S, Lenne D, Raoul W, Calippe B, et al. Neonatal hyperglycemia inhibits angiogenesis and induces inflammation and neuronal degeneration in the retina. PLoS ONE. 2013;8:e79545.
Callaway DA, McGill-Vargas LL, Quinn A, Jordan JL, Winter LA, Anzueto D, et al. Prematurity disrupts glomeruli development, whereas prematurity and hyperglycemia lead to altered nephron maturation and increased oxidative stress in newborn baboons. Pediatr Res. 2018;83:702–11.
Gisslen T, Ennis K, Bhandari V, Rao R. Recurrent hypoinsulinemic hyperglycemia in neonatal rats increases PARP-1 and NF-κB expression and leads to microglial activation in the cerebral cortex. Pediatr Res. 2015;78:513–9.
Ramel S, Rao R. Hyperglycemia in extremely preterm infants. Neoreviews. 2020;21:e89–e97.
Lagacé M, Tam EWY. Neonatal dysglycemia: a review of dysglycemia in relation to brain health and neurodevelopmental outcomes. Pediatr Res. 2024;96:1429–37.
Beardsall K, Vanhaesebrouck S, Ogilvy-Stuart AL, Vanhole C, Palmer CR, van Weissenbruch M, et al. Early insulin therapy in very-low-birth-weight infants. N Engl J Med. 2008;359:1873–84.
Bottino M, Cowett RM, Sinclair JC. Interventions for treatment of neonatal hyperglycemia in very low birth weight infants. Cochrane Database Syst Rev. 2011;10:CD007453.
Tottman AC, Alsweiler JM, Bloomfield FH, Gamble G, Jiang Y, Leung M, et al. Long-term outcomes of hyperglycemic preterm infants randomized to tight glycemic control. J Pediatr. 2018;193:68–75.e1.
Hays SP, Smith EO, Sunehag AL. Hyperglycemia is a risk factor for early death and morbidity in extremely low birth-weight infants. Pediatrics. 2006;118:1811–8.
Beardsall K, Thomson L, Guy C, Iglesias-Platas I, van Weissenbruch MM, Bond S, et al. Real-time continuous glucose monitoring in preterm infants (REACT): an international, open-label, randomised controlled trial. Lancet Child Adolesc Health. 2021;5:265–73.
Lee JH, Hornik CP, Testoni D, Laughon MM, Cotten CM, Maldonado RS, et al. Insulin, hyperglycemia, and severe retinopathy of prematurity in extremely low-birth-weight infants. Am J Perinatol. 2016;33:393–400.
Stensvold HJ, Strommen K, Lang AM, Abrahamsen TG, Steen EK, Pripp AH, et al. Early enhanced parenteral nutrition, hyperglycemia, and death among extremely low-birth-weight infants. JAMA Pediatr. 2015;169:1003–10.
Yoo HS, Ahn SY, Lee MS, Han YM, Sung SI, Chang YS, et al. Permissive hyperglycemia in extremely low birth weight infants. J Korean Med Sci. 2013;28:450–60.
Yamauchi T, Imamura M, Takasawa K, Nakajima K, Nakagawa R, Gau M, et al. Prematurity at less than 24 weeks of gestation is a risk for prolonged hyperglycemia in extremely low-birth weight infants. Endocrine. 2020;70:71–7.
Beardsall K, Vanhaesebrouck S, Ogilvy-Stuart AL, Vanhole C, Palmer CR, Ong K, et al. Prevalence and determinants of hyperglycemia in very low birth weight infants: cohort analyses of the NIRTURE study. J Pediatr. 2010;157:715–9 e1-3.
Koyama T, Osada H, Tsujii H, Kurita H. Utility of the Kyoto Scale of Psychological Development in cognitive assessment of children with pervasive developmental disorders. Psychiatry Clin Neurosci. 2009;63:241–3.
Kono Y, Yonemoto N, Kusuda S, Hirano S, Iwata O, Tanaka K, et al. Developmental assessment of VLBW infants at 18 months of age: A comparison study between KSPD and Bayley III. Brain Dev. 2016;38:377–85.
Kono Y, Mishina J, Yonemoto N, Kusuda S, Fujimura M. Outcomes of very-low-birthweight infants at 3 years of age born in 2003-2004 in Japan. Pediatr Int. 2011;53:1051–8.
Administration USFaD. CLIA - Clinical Laboratory Improvement Amendments [Available from: https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfClia/Results.cfm?start_search=1&Document_Number=CW180011&SortColumn=ded.
Chen H, Yao Q, Dong Y, Tang Z, Li R, Cai B, et al. The accuracy evaluation of four blood glucose monitoring systems according to ISO 15197:2003 and ISO 15197:2013 criteria. Prim Care Diabetes. 2019;13:252–8.
Itabashi K, Miura F, Uehara R, Nakamura Y. New Japanese neonatal anthropometric charts for gestational age at birth. Pediatr Int. 2014;56:702–8.
Jobe AH, Bancalari E. Bronchopulmonary dysplasia. Am J Respir Crit Care Med. 2001;163:1723–9.
Papile LA, Burstein J, Burstein R, Koffler H. Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1500 gm. J Pediatr. 1978;92:529–34.
Bell MJ, Ternberg JL, Feigin RD, Keating JP, Marshall R, Barton L, et al. Neonatal necrotizing enterocolitis. Therapeutic decisions based upon clinical staging. Ann Surg. 1978;187:1–7.
Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transpl. 2013;48:452–8.
Zamir I, Stoltz Sjostrom E, Ahlsson F, Hansen-Pupp I, Serenius F, Domellof M. Neonatal hyperglycaemia is associated with worse neurodevelopmental outcomes in extremely preterm infants. Arch Dis Child Fetal Neonatal Ed. 2021;106:460–6.
Van Der Lugt NM, Smits-Wintjens VE, Van Zwieten PH, Walther FJ. Short and long term outcome of neonatal hyperglycemia in very preterm infants: a retrospective follow-up study. BMC Pediatrics. 2010;10:52.
Heald A, Abdel-Latif ME, Kent AL. Insulin infusion for hyperglycaemia in very preterm infants appears safe with no effect on morbidity, mortality and long-term neurodevelopmental outcome. J Matern Fetal Neonatal Med. 2012;25:2415–8.
Mitanchez-Mokhtari D, Lahlou N, Kieffer F, Magny JF, Roger M, Voyer M. Both relative insulin resistance and defective islet beta-cell processing of proinsulin are responsible for transient hyperglycemia in extremely preterm infants. Pediatrics. 2004;113:537–41.
McKinlay CJD, Alsweiler JM, Anstice NS, Burakevych N, Chakraborty A, Chase JG, et al. Association of Neonatal Glycemia With Neurodevelopmental Outcomes at 4.5 Years. JAMA Pediatr. 2017;171:972–83.
Morgan C. The potential risks and benefits of insulin treatment in hyperglycaemic preterm neonates. Early Hum Dev. 2015;91:655–9.
Beardsall K, Vanhaesebrouck S, Frystyk J, Ogilvy-Stuart AL, Vanhole C, van Weissenbruch M, et al. Relationship between insulin-like growth factor I levels, early insulin treatment, and clinical outcomes of very low birth weight infants. J Pediatr. 2014;164:1038–44.e1.
Kothadia JM, O’Shea TM, Roberts D, Auringer ST, Weaver RG 3rd, et al. Randomized placebo-controlled trial of a 42-Day tapering course of dexamethasone to reduce the duration of ventilator dependency in very low birth weight infants. Pediatrics. 1999;104:22–7.
Doyle LW, Cheong JL, Hay S, Manley BJ, Halliday HL. Late (≥ 7 days) systemic postnatal corticosteroids for prevention of bronchopulmonary dysplasia in preterm infants. Cochrane Database Syst Rev. 2021;11:Cd001145.
Hey E. Hyperglycaemia and the very preterm baby. Semin Fetal Neonatal Med. 2005;10:377–87.
Bermick J, Dechert RE, Sarkar S. Does hyperglycemia in hypernatremic preterm infants increase the risk of intraventricular hemorrhage? J Perinatol. 2016;36:729–32.
Author information
Authors and Affiliations
Contributions
Y.M. performed the study design, data collection, statistical analyses, drafted the initial manuscript, and revised the manuscript. K.N. made substantial contributions to the study design and interpretation of data and revised the manuscript. F.N. provided supervision throughout the entire process and made substantial contributions to the study design, interpretation of data and revision of the manuscript. All authors have read the draft and approved the final manuscript as submitted.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
This study was approved by the Ethics Committee of Saitama Medical Center, Saitama Medical University (approval number: 2024-048). This retrospective observational study was conducted using the opt-out method on our hospital website with a waiver of additional written informed consent. All methods used in this study were conducted in accordance with the relevant guidelines and regulations.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Minamitani, Y., Nakajima, K. & Namba, F. Association of hyperglycemia in extremely preterm infants with neurodevelopmental outcomes at 18 months of corrected age. J Perinatol 45, 1370–1376 (2025). https://doi.org/10.1038/s41372-025-02388-w
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41372-025-02388-w