Abstract
Objective
Characteristics associated with extubation success (ES) in established grade 3 bronchopulmonary dysplasia (G3-BPD) are unknown. The respiratory severity score (RSS) is associated with extubation failure in younger preterm infants and adverse outcomes in established BPD. We evaluated the association between the RSS and ES in G3-BPD.
Study design
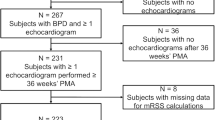
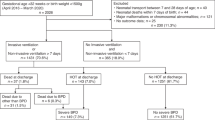
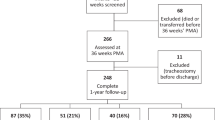
Retrospective observational study of infants diagnosed with G3-BPD undergoing their first extubation attempt after 36 weeks postmenstrual age (PMA). Bivariable and multivariable logistic regression models were used to determine the associations between RSS and ES while adjusting for confounding characteristics.
Results
Among 239 infants with G3-BPD undergoing an extubation attempt with a median RSS of 3.0, 142 (59%) were successful. A higher RSS was associated with lower odds of ES in adjusted analysis.
Conclusion
RSS is independently associated with ES in infants with established G3-BPD undergoing their first extubation attempt after 36 weeks PMA, with lower odds of success as RSS increases.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The datasets generated during/or analyzed during the current study and the code used to analyze and manage the data are available from the corresponding author on reasonable request.
References
Horbar JD, Carpenter JH, Badger GJ, Kenny MJ, Soll RF, Morrow KA, et al. Mortality and neonatal morbidity among infants 501 to 1500 grams from 2000 to 2009. Pediatrics. 2012;129:1019–26.
Stoll BJ, Hansen NI, Bell EF, Shankaran S, Laptook AR, Walsh MC, et al. Neonatal outcomes of extremely preterm infants from the NICHD Neonatal Research Network. Pediatrics. 2010;126:443–56.
Fanaroff AA, Stoll BJ, Wright LL, Carlo WA, Ehrenkranz RA, Stark AR, et al. Trends in neonatal morbidity and mortality for very low birthweight infants. Am J Obstet Gynecol. 2007;196:147–e1.
Al-Mandari H, Shalish W, Dempsey E, Keszler M, Davis PG, Sant’Anna G. International survey on periextubation practices in extremely preterm infants. Arch Dis Child-Fetal Neonatal Ed. 2015;100:F428–31.
Shalish W, Kanbar L, Kovacs L, Chawla S, Keszler M, Rao S, et al. Assessment of extubation readiness using spontaneous breathing trials in extremely preterm neonates. JAMA Pediatrics. 2020;174:178–85.
Shalish W, Latremouille S, Papenburg J, Sant’Anna GM. Predictors of extubation readiness in preterm infants: a systematic review and meta-analysis. Arch Dis Child-Fetal Neonatal Ed. 2019;104:F89–97.
Cheng Z, Dong Z, Zhao Q, Zhang J, Han S, Gong J, et al. A prediction model of extubation failure risk in preterm infants. Front Pediatrics. 2021;9:693320.
Chawla S, Natarajan G, Shankaran S, Carper B, Brion LP, Keszler M, et al. Markers of successful extubation in extremely preterm infants, and morbidity after failed extubation. J Pediatrics. 2017;189:113–9.
Gupta D, Greenberg RG, Sharma A, Natarajan G, Cotten M, Thomas R, et al. A predictive model for extubation readiness in extremely preterm infants. J Perinatol. 2019;39:1663–9.
Mhanna MJ, Iyer NP, Piraino S, Jain M. Respiratory severity score and extubation readiness in very low birth weight infants. Pediatrics Neonatol. 2017;58:523–8.
Jung YH, Jang J, Kim HS, Shin SH, Choi CW, Kim EK, et al. Respiratory severity score as a predictive factor for severe bronchopulmonary dysplasia or death in extremely preterm infants. BMC Pediatrics. 2019;19:1–8.
Kielt MJ, Logan JW, Backes CH, Conroy S, Reber KM, Shepherd EG, et al. Noninvasive respiratory severity indices predict adverse outcomes in bronchopulmonary dysplasia. J Pediatrics. 2022;242:129–36.
Beer L, Rivera BK, Jama W, Slaughter JL, Backes CH, Conroy S, et al. Association of the respiratory severity score with bronchopulmonary dysplasia-associated pulmonary hypertension in infants born extremely preterm. J Perinatol. 2024;44:294–300.
Jensen EA, Dysart K, Gantz MG, McDonald S, Bamat NA, Keszler M, et al. The diagnosis of bronchopulmonary dysplasia in very preterm infants. An evidence-based approach. Am J Respiratory Crit care Med. 2019;200:751–9.
Doyle LW, Davis PG, Morley CJ, McPhee A, Carlin JB, DART Study Investigators. Low-dose dexamethasone facilitates extubation among chronically ventilator-dependent infants: a multicenter, international, randomized, controlled trial. Pediatrics. 2006;117:75–83.
Natarajan A, Lam G, Liu J, Beam AL, Beam KS, Levin JC. Prediction of extubation failure among low birthweight neonates using machine learning. J Perinatol. 2023;43:209–14.
Khodak I, Kahovec M, Romano V, Nielsen A, Day CL, Dylag AM. Reducing Failed Extubations in preterm infants via standardization and real-time decision support. Pediatrics. 2024;154:e2023062930.
Acknowledgements
We would like to thank Matthew Devine and Bolu Oluwalade in the Division of Neonatology for their data abstraction work.
Author information
Authors and Affiliations
Contributions
AZ, and NB conceptualized and designed the study, supervised, and collected data, designed the methodology with help from MH, interpreted the data, and analyzed results. MH carried out the analysis under supervision from NB. AZ wrote the initial manuscript draft, and reviewed and revised the manuscript throughout the submission process. KG, SL, TN helped conceptualize and revise the study. KG, SL, MH, TN reviewed and revised the manuscript throughout the submission process. NB reviewed and revised the initial draft and was involved with revisions throughout the submission process.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
Data used for this study was approved for collection by the CHOP Institutional Review Board, #19-016420. Informed consent was not required. All methods were performed in accordance with relevant guidelines and regulations.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zierk, A.W., Gibbs, K.A., Nelin, T.D. et al. Association between the respiratory severity score and extubation success in severe bronchopulmonary dysplasia. J Perinatol (2025). https://doi.org/10.1038/s41372-025-02396-w
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41372-025-02396-w