Abstract
Objective
To examine maternal risk factors for congenital syphilis (CS).
Study design
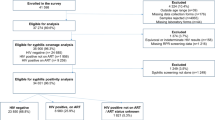
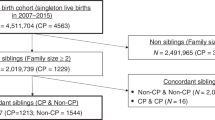
We used a retrospective, population-based cohort of births in California (2011–2021) with linked birth certificates and hospital records. Modified Poisson regression models with robust standard errors were used to assess characteristics associated with CS. Among dyads with CS, maternal syphilis documentation was also examined.
Results
Of 4,481,096 births, 4659 (0.1%) had maternal syphilis without CS, and 2608 (0.06%) had both maternal syphilis and CS. CS was associated with having public insurance, tobacco use, drug use disorders, and residence in fringe-metro or medium/small-metro counties. Among CS dyads, 62.0% had no maternal syphilis documentation. There was a lower risk of no maternal syphilis documentation among those with <12th grade education; non-Hispanic Black identity; tobacco, cannabis, or drug use disorders; mental health conditions; and inadequate prenatal care.
Conclusions
Universal prenatal syphilis screening, treatment, and documentation are essential to preventing CS.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
Due to restrictions from the Committee for the Protection of Human Subjects (CPHS), data cannot be released by the authors. Individuals may apply for California vital statistics and California Department of Health Care Access and Information (HCAI) data directly from the Health and Human Services Agency (HHSA). Stata code used in this analysis is available upon request from the corresponding author.
References
Gregory ECW, Ely DM. Trends and characteristics in maternal syphilis rates during pregnancy: United States, 2016–2022. National Center for Health Statistics, Centers for Disease Control and Prevention; 2024.
David M, Hcini N, Mandelbrot L, Sibiude J, Picone O. Fetal and neonatal abnormalities due to congenital syphilis: a literature review. Prenat Diagn. 2022;42:643–55.
McClure EM, Silver RM, Kim J, Ahmed I, Kallapur M, Ghanchi N, et al. Maternal infection and stillbirth: a review. J Matern Fetal Neonatal Med. 2022;35:4442–50.
Rocha AFB, Araújo MAL, Barros VLD, Américo CF, Silva Júnior GBD. Complications, clinical manifestations of congenital syphilis, and aspects related to its prevention: an integrative review. Rev Bras Enferm. 2021;74:e20190318.
Stafford IA, Workowski KA, Bachmann LH. Syphilis complicating pregnancy and congenital syphilis. N Engl J Med. 2024;390:242–53.
Chen H-Y, Klausner JD, Stafford IA. Congenital syphilis in live births: adverse outcomes, hospital length of stay, and costs. Obstet Gynecol. 2024;144:207–14.
McDonald R, O’Callaghan K, Torrone E, Barbee L, Grey J, Jackson D, et al. Vital signs: missed opportunities for preventing congenital syphilis—United States, 2022. Morb Mortal Wkly Rep. 2023;72:1269–74.
Kimball A, Torrone E, Miele K, Bachmann L, Thorpe P, Weinstock H, et al. Missed opportunities for prevention of congenital syphilis—United States, 2018. Morb Mortal Wkly Rep. 2020;69:661–5.
Workowski K, Bachmann L, Chan P, Johnston CM, Muzny CA, Park I, et al. Sexually transmitted infections treatment guidelines, 2021. MMWR Recomm Rep. 2021;70:1–187.
California Department of Public Health. California sexually transmitted infections (STIs) treatment guidelines for adults and adolescents. Sacramento, CA: Sexually Transmitted Diseases Control Branch; 2025.
Alexander JM, Sheffield JS, Sanchez PJ, Mayfield J, Wendel GD Jr. Efficacy of treatment for syphilis in pregnancy. Obstet Gynecol. 1999;93:5–8.
Tannis A, Miele K, Carlson JM, O’Callaghan KP, Woodworth KR, Anderson B, et al. Syphilis treatment among people who are pregnant in six U.S. States, 2018–2021. Obstet Gynecol. 2024;143:718–29.
Machefsky AM, Loosier PS, Cramer R, Bowen VB, Kersh EN, Tao G, et al. A new call to action to combat an old nemesis: addressing rising congenital syphilis rates in the United States. J Women’s Health. 2021;30:920–6.
O’Connor NP, Gonzalez BE, Esper FP, Tamburro J, Kadkhoda K, Foster CB. Congenital syphilis: missed opportunities and the case for rescreening during pregnancy and at delivery. IDCases. 2020;22:e00964.
Cooper JM, Sánchez PJ. Congenital syphilis. Semin Perinatol. 2018;42:176–84.
Fukuda A, Katz AR, Park IU, Komeya AY, Chang A, Ching N, et al. Congenital syphilis: a case report demonstrating missed opportunities for screening and inadequate treatment despite multiple health care encounters during pregnancy. Sex Transm Dis. 2021;48:e124–e5.
Smullin C, Wagman J, Mehta S, Klausner JD. A narrative review of the epidemiology of congenital syphilis in the United States from 1980 to 2019. Sex Transm Dis. 2021;48:71–8.
Biswas HH, Chew Ng RA, Murray EL, Chow JM, Stoltey JE, Watt JP, et al. Characteristics associated with delivery of an infant with congenital syphilis and missed opportunities for prevention-California, 2012 to 2014. Sex Transm Dis. 2018;45:435–41.
Carlson JM, Tannis A, Woodworth KR, Reynolds MR, Shinde N, Anderson B, et al. Substance use among persons with syphilis during pregnancy—Arizona and Georgia, 2018–2021. MMWR Morb Mortal Wkly Rep. 2023;72:63–7.
Kachikis A, Schiff MA, Moore K, Chapple-McGruder T, Arluck J, Hitti J. Risk factors associated with congenital syphilis, Georgia, 2008–2015. Infect Dis Obstet Gynecol. 2023;2023:3958406.
Staneva M, Hobbs CV, Dobbs T. Spike in congenital syphilis, Mississippi, USA, 2016–2022. Emerg Infect Dis. 2023;29:1965–72.
DiOrio D, Kroeger K, Ross A. Social vulnerability in congenital syphilis case mothers: qualitative assessment of cases in Indiana, 2014 to 2016. Sex Transm Dis. 2018;45:447–51.
Villarreal DD, Lewis KA, Cielo M, Klausner JD. Patterns of congenital syphilis in a large public hospital: birthing parent risk factors and infant outcomes. Sex Transm Dis. 2025;52:395-401.
Daniels E, Atkinson A, Cardoza N, Ramakrishnan A, Willers D, Reno H. Social factors associated with congenital syphilis in Missouri. Clin Infect Dis. 2024;79:744–50.
Round JM, Plitt SS, Eisenbeis L, Smyczek P, Gratrix J, Charlton C, et al. Examination of Care milestones for preventing congenital syphilis transmission among syphilis-infected pregnant women in Alberta, Canada: 2017–2019. Sex Transm Dis. 2022;49:477–83.
Baer RJ, Bandoli G, Jelliffe-Pawlowski L, Chambers CD. The University of California study of outcomes in mothers and infants (a Population-Based Research Resource): retrospective cohort study. JMIR Public Health Surveill. 2024;10:e59844.
Centers for Disease Control and Prevention. National overview of STIs, 2022. Atlanta, GA: Centers for Disease Control and Prevention; 2022.
Kimball A, Bowen VB, Miele K, Weinstock H, Thorpe P, Bachmann L, et al. Congenital syphilis diagnosed beyond the neonatal period in the United States: 2014–2018. Pediatrics. 2021;148:e2020049080.
Centers for Disease Control and Prevention. 2013 NCHS Urban-Rural Classification Scheme for Counties. Hyattsville, MD: National Center for Health Statistics, US Department of Health and Human Services; 2014. Contract No: 166.
Kotelchuck M. The adequacy of prenatal care utilization index: its us distribution and association with low birthweight. Am J Public Health. 1994;84:1486–9.
Chen W, Qian L, Shi J, Franklin M. Comparing performance between log-binomial and robust Poisson regression models for estimating risk ratios under model misspecification. BMC Med Res Methodol. 2018;18:63.
Zou, G. A modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159;702–6
Goyal M, Singh P, Singh K, Shekhar S, Agrawal N, Misra S. The effect of the COVID-19 pandemic on maternal health due to delay in seeking health care: experience from a tertiary center. Int J Gynaecol Obstet. 2021;152:231–5.
Lee J. Correlates of and disparities in cancellations or delays of prenatal visits during the COVID-19 pandemic: emphasis on racial/ethnic minorities and persons with low socioeconomic status. J Racial Ethn Health Disparities. 2024;11:1564–77.
Stanford KA, Mason JA, Friedman EE. Trends in STI testing and diagnosis rates during the COVID-19 pandemic at a large urban tertiary care center, and the role of the emergency department in STI care. Front Reprod Health. 2023;5:1082429.
Hackett C, Frank L, Heldt-Werle L, Loosier PS. Provider-reported barriers in sexual health care services for women with upstream barriers: the case of syphilis and congenital syphilis in Southern Colorado, 2022. Sex Transm Dis. 2024;51:337–41.
Klaman SL, Lorvick J, Jones HE. Provision of and barriers to integrating reproductive and sexual health services for reproductive-age women in opioid treatment programs. J Addict Med. 2019;13:422–9.
Klaman SL, Turner K, Lorvick J, Jones HE. Integrating reproductive and sexual health education and services into opioid use disorder treatment programs: a qualitative study. J Addict Med. 2020;14:e175–e82.
MacAfee LK, Harfmann RF, Cannon LM, Minadeo L, Kolenic G, Kusunoki Y, et al. Substance use treatment patient and provider perspectives on accessing sexual and reproductive health services: barriers, facilitators, and the need for integration of care. Subst Use Misuse. 2020;55:95–107.
Strathdee SA, Bristow CC, Gaines T, Shoptaw S. Collateral Damage: a narrative review on epidemics of substance use disorders and their relationships to sexually transmitted infections in the United States. Sex Transm Dis. 2021;48:466–73.
American College of Obstetricians and Gynecologists. Practice advisory: screening for syphilis in pregnancy. Washington, DC: American College of Obstetricians and Gynecologists; 2024.
California Department of Public Health (CDPH) updates syphilis screening recommendations [press release]. Sacramento, CA: California Department of Public Health (CDPH); 2024.
Dude AM, Drexler K, Yee LM, Badreldin N. Adherence to sexually transmitted infection screening in pregnancy. J Women’s Health. 2023;32:652–6.
Asher GN, Viswanathan M, Takyi A, Middleton JC, Baker C, Kahwati LC. Screening for syphilis infection during pregnancy: updated evidence report and systematic review for the US preventive services task force. JAMA. 2025;333:2015–7.
Fang J, Silva RM, Tancredi DJ, Pinkerton KE, Sankaran D. Examining associations in congenital syphilis infection and socioeconomic factors between California’s small-to-medium and large metro counties. J Perinatol. 2022;42:1434–9.
Williams CL, Harrison LL, Llata E, Smith RA, Meites E. Sexually transmitted diseases among pregnant women: 5 States, United States, 2009–2011. Matern Child Health J. 2018;22:538–45.
Leichliter JS, Grey JA, Cuffe KM, de Voux A, Cramer R, Hexem S, et al. Geographic correlates of primary and secondary syphilis among men who have sex with men in the United States. Ann Epidemiol. 2019;32:14–9.e1.
Ahmad FA, Dickey V, Tetteh EK, Foraker R, McKay VR. The use of the consolidated framework for implementation research to understand facilitators and barriers to sexually transmitted infection screening in primary care. Sex Transm Dis. 2022;49:610–5.
Baynes A, McArthur A. Adherence to recommended Australian sexually transmitted infections screening guidelines among asymptomatic men who have sex with men: a best practice implementation project. JBI Evid Synth. 2014;12:210–26.
Cullinen K, Hill M, Anderson T, Jones V, Nelson J, Halawani M, et al. Improving sexually transmitted infection screening, testing, and treatment among people with HIV: a mixed-method needs assessment to inform a multi-site, multi-level intervention and evaluation plan. PLoS ONE. 2022;16:e0261824.
Shangani S, Bhaskar N, Richmond N, Operario D, van den Berg JJ. A systematic review of early adoption of implementation science for HIV prevention or treatment in the United States. AIDS. 2021;35:177–91.
Johnson EK, Nelson CP. Values and pitfalls of the use of administrative databases for outcomes assessment. J Urol. 2013;190:17–8.
Katz A, Freier A. Recognition of inherent biases in administrative data. Can Fam Physician. 2022;68:933–4.
Funding
This study was supported by the Study of Outcomes of Mothers and Infants (SOMI) at the University of California San Diego. Additional support was provided by the National Institutes of Health (NIH), National Institute on Drug Abuse (NIDA) grant T32DA052142 to JF. NIH had no role in the study design, analysis, interpretation, writing, or decision to submit this study for publication.
Author information
Authors and Affiliations
Contributions
JF conceptualized the study, conducted the formal analysis, and wrote the original draft of the manuscript. RJB was responsible for data management and provided a curated dataset for the analysis. NM, RJ, and CC contributed to the conceptualization of the study, writing and interpretation of the results, and editing of the manuscript. All authors approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
All study protocols were approved by the Committee for the Protection of Human Subjects (CPHS) within the Health and Human Services Agency (HHSA) of the State of California and the Institutional Review Board at the University of California San Diego. The study was conducted in accordance with the Declaration of Helsinki, and we received a waiver for informed consent due to the nature of the administrative dataset and minimal risk of the study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Frankeberger, J., Matoba, N., Baer, R.J. et al. Identifying missed prevention opportunities: maternal and congenital syphilis in hospital records and birth certificates in California from 2011 to 2021. J Perinatol (2025). https://doi.org/10.1038/s41372-025-02450-7
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41372-025-02450-7