Abstract
Objective
To quantify opioid and benzodiazepine exposure in extremely preterm neonates and assess variation by gestational age, facility, and clinical factors.
Study design
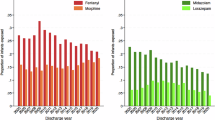
Cross-sectional study of 1501 neonates born at 23–28 weeks gestation at Kaiser Permanente Northern California (2011–2021). Medication data were extracted from electronic records. Cumulative opioid and benzodiazepine exposures were standardized to morphine and lorazepam equivalents per kg. Logistic regression evaluated associations with clinical comorbidities.
Results
Thirty percent of neonates were exposed to both drug classes, 24% to opioids alone, and 1.5% to benzodiazepines alone. Exposure was inversely related to gestational age and varied widely across facilities. High opioid exposure (≥10 MME/kg) was associated with mechanical ventilation (aOR 3.7), vasopressors (aOR 4.6), oxygen at 36 weeks (aOR 1.7), and severe IVH (aOR 2.5).
Conclusions
Opioid and benzodiazepine use is common and variable in extremely preterm neonates. Standardized pain management and long-term outcome studies are urgently needed.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Carbajal R, Rousset A, Danan C, Coquery S, Nolent P, Ducrocq S, et al. Epidemiology and treatment of painful procedures in neonates in intensive care units. JAMA. 2008;300:60–70.
Committee on Fetus and Newborn and Section on Anesthesiology and Pain Medicine. Prevention and management of procedural pain in the neonate: an update. Pediatrics 2016;137:e20154271.
Smith GC, Gutovich J, Smyser C, Pineda R, Newnham C, Tjoeng TH, et al. Neonatal intensive care unit stress is associated with brain development in preterm infants. Ann Neurol. 2011;70:541–9.
Brummelte S, Grunau RE, Chau V, Poskitt KJ, Brant R, Vinall J, et al. Procedural pain and brain development in premature newborns. Ann Neurol. 2012;71:385–96.
Bouza H. The impact of pain in the immature brain. J Matern Fetal Neonatal Med. 2009;22:722–32.
Doesburg SM, Chau CM, Cheung TPL, Moiseev A, Ribary U, Herdman AT, et al. Neonatal pain-related stress, functional cortical activity and visual-perceptual abilities in school-age children born at extremely low gestational age. Pain. 2013;154:1946–52.
McPherson C, Miller SP, El-Dib M, Massaro AN, Inder TE. The influence of pain, agitation, and their management on the immature brain. Pediatr Res. 2020;88:168–75.
Selvanathan T, Ufkes S, Guo T, Chau V, Branson HM, Ibrahim GM, et al. Pain exposure and brain connectivity in preterm infants. JAMA Netw Open. 2024;7:e242551.
Lim Y, Godambe S. Prevention and management of procedural pain in the neonate: an update, American Academy of Pediatrics, 2016. Arch Dis Child Educ Pr Ed. 2017;102:254–6.
Zwicker JG, Miller SP, Grunau RE, Chau V, Brant R, Studholme C, et al. Smaller cerebellar growth and poorer neurodevelopmental outcomes in very preterm infants exposed to neonatal morphine. J Pediatr. 2016;172:81–7.e2.
McPherson C, Haslam M, Pineda R, Rogers C, Neil JJ, Inder TE. Brain injury and development in preterm infants exposed to fentanyl. Ann Pharmacother. 2015;49:1291–7.
Selvanathan T, Zaki P, McLean MA, Au-Young SH, Chau C, Chau V, et al. Early-life exposure to analgesia and 18-month neurodevelopmental outcomes in very preterm infants. Pediatr Res. 2023;94:738–46.
Puia-Dumitrescu M, Comstock BA, Li S, Heagerty PJ, Perez KM, Law JB, et al. Assessment of 2-year neurodevelopmental outcomes in extremely preterm infants receiving opioids and benzodiazepines. JAMA Netw Open. 2021;4:e2115998.
Kocek M, Wilcox R, Crank C, Patra K. Evaluation of the relationship between opioid exposure in extremely low birth weight infants in the neonatal intensive care unit and neurodevelopmental outcome at 2 years. Early Hum Dev. 2016;92:29–32.
Steinbauer P, Deindl P, Fuiko R, Unterasinger L, Cardona F, Wagner M, et al. Long-term impact of systematic pain and sedation management on cognitive, motor, and behavioral outcomes of extremely preterm infants at preschool age. Pediatr Res. 2021;89:540–8.
Mills KP, Lean RE, Smyser CD, Inder T, Rogers C, McPherson CC. Fentanyl exposure in preterm infants: Five-year neurodevelopmental and socioemotional assessment. Front Pain Res. 2022;3:836705.
Giordano V, Deindl P, Fuiko R, Unterasinger L, Waldhoer T, Cardona F, et al. Effect of increased opiate exposure on three years neurodevelopmental outcome in extremely preterm infants. Early Hum Dev. 2018;123:1–5.
Young C, Jevtovic-Todorovic V, Qin YQ, Tenkova T, Wang H, Labruyere J, et al. Potential of ketamine and midazolam, individually or in combination, to induce apoptotic neurodegeneration in the infant mouse brain. Br J Pharm. 2005;146:189–97.
Stefovska VG, Uckermann O, Czuczwar M, Smitka M, Czuczwar P, Kis J, et al. Sedative and anticonvulsant drugs suppress postnatal neurogenesis. Ann Neurol. 2008;64:434–45.
Anand KJ, Hall RW, Desai N, Shephard B, Bergqvist LL, Young TE, et al. Effects of morphine analgesia in ventilated preterm neonates: primary outcomes from the NEOPAIN randomised trial. Lancet. 2004;363:1673–82.
Ng E, Klinger G, Shah V, Taddio A. Safety of benzodiazepines in newborns. Ann Pharmacother. 2002;36:1150–5.
Curtis S, Kilpatrick R, Billimoria ZC, Zimmerman K, Tolia V, Clark R, et al. Use of dexmedetomidine and opioids in hospitalized pretermiInfants. JAMA Netw Open. 2023;6:e2341033.
Durrmeyer X, Vutskits L, Anand KJ, Rimensberger PC. Use of analgesic and sedative drugs in the NICU: integrating clinical trials and laboratory data. Pediatr Res. 2010;67:117–27.
Gordon N. Similarity of the adult Kaiser Permanente membership in Northern California to the insured and general population in Northern California: Statistics from the 2011-12 California Health Interview Survey. 2015. https://divisionofresearch.kaiserpermanente.org/projects/memberhealthsurvey/SiteCollectionDocuments/chis_non_kp_2011.pdf.
Mehler K, Oberthuer A, Haertel C, Herting E, Roth B, Goepel W, et al. Use of analgesic and sedative drugs in VLBW infants in German NICUs from 2003-2010. Eur J Pediatr. 2013;172:1633–9.
Carbajal R, Eriksson M, Courtois E, Boyle E, Avila-Alvarez A, Andersen RD, et al. Sedation and analgesia practices in neonatal intensive care units (EUROPAIN): results from a prospective cohort study. Lancet Respir Med. 2015;3:796–812.
Borenstein-Levin L, Synnes A, Grunau RE, Miller SP, Yoon EW, Shah PS, et al. Narcotics and sedative use in preterm neonates. J Pediatr. 2017;180:92–8.e1.
Schiller RM, Allegaert K, Hunfeld M, van den Bosch GE, van den Anker J, Tibboel D. Analgesics and sedatives in critically ill newborns and infants: The impact on long-term neurodevelopment. J Clin Pharm. 2018;58:S140–50.
Davidson A, Flick RP. Neurodevelopmental implications of the use of sedation and analgesia in neonates. Clin Perinatol. 2013;40:559–73.
Walter-Nicolet E, Marchand-Martin L, Morgan AS, Kaminski M, Benhammou V, Ancel PY, et al. Neurodevelopmental outcomes at five years in children born very preterm (24-31 weeks) exposed to opioids with or without midazolam: results from the French nationwide EPIPAGE-2 cohort study. Lancet Reg Health Eur. 2025;52:101242.
Duerden EG, Guo T, Dodbiba L, Chakravarty MM, Chau V, Poskitt KJ, et al. Midazolam dose correlates with abnormal hippocampal growth and neurodevelopmental outcome in preterm infants. Ann Neurol. 2016;79:548–59.
McPherson C, Grunau RE. Neonatal pain control and neurologic effects of anesthetics and sedatives in preterm infants. Clin Perinatol. 2014;41:209–27.
Acknowledgements
Funded in part by a grant from the US Food and Drug Administration U01FD007702.
Author information
Authors and Affiliations
Contributions
All authors contributed to the: 1. Conception and design of the work. 2. The acquisition, analysis, and interpretation of data. 3. Drafting the work and reviewing it critically for important intellectual content. 4. Final approval of the version to be published.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kuzniewicz, M.W., Sun, L.S., Lahiri, A. et al. Cumulative exposure to opioids and benzodiazepines in extremely preterm neonates. J Perinatol (2025). https://doi.org/10.1038/s41372-025-02513-9
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41372-025-02513-9