Abstract
Background
Parental presence at bedside is a critical component of family-centered care for infants admitted to Neonatal Intensive Care Units (NICUs) and their caregivers, allowing for engagement with baby as well as education from the care team.
Local problem
Many families face barriers to physical presence, including transportation, childcare responsibilities, work, and illness, among others.
Interventions
Telehealth can be an avenue for parents to be engaged while not directly at bedside. This project details efforts to launch virtual visits in a Level III NICU, including challenges and lessons learned, across 4 PDSA cycles.
Methods
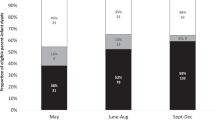
We measured the percentage of families on the NICU who attended 4 or more cares sessions per week. We obtained survey responses and open-ended feedback about the implementation from staff and patients.
Results
Family engagement rates were higher during active PDSA cycles at trending significance level. Most providers and parents rated the intervention as highly feasible and satisfying. Attendance in cares sessions improved across the QI project, especially for families with public insurance.
Conclusions
We found that telehealth visits were able to lessen the disparities in cares participation rates between families with private insurance and families with public insurance.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
Data may be shared upon reasonable request to the corresponding author.
References
Novak JL, Vittner D. Parent engagement in the NICU. J Neonatal Nurs. 2021;27:257–62.
Lewis TP, Andrews KG, Shenberger E, Betancourt TS, Fink G, Pereira S, et al. Caregiving can be costly: a qualitative study of barriers and facilitators to conducting kangaroo mother care in a US tertiary hospital neonatal intensive care unit. BMC Pregnancy Childbirth. 2019;19:1–12.
Bourque SL, Williams VN, Scott J, Hwang SS. The role of distance from home to hospital on parental experience in the NICU: a qualitative study. Children. 2023;10:1576.
Seaton SE, Barker L, Draper ES, Abrams KR, Modi N, Manktelow BN, et al. Estimating neonatal length of stay for babies born very preterm. Arch Dis Child Fetal Neonatal Ed. 2019;104:F182–6.
Kelleher J, Dempsey J, Takamatsu S, Paul JJ, Kent E, Dempsey AG. Adaptation of infant mental health services to preterm infants and their families receiving neonatal intensive care unit services during the COVID-19 pandemic. Infant Ment Health J. 2022;43:100–10.
Pineda R, Bender J, Hall B, Shabosky L, Annecca A, Smith J. Parent participation in the neonatal intensive care unit: predictors and relationships to neurobehavior and developmental outcomes. Early Hum Dev. 2018;117:32–8.
Bourque SL, Weikel BW, Palau MA, Greenfield JC, Hall A, Klawetter S, et al. The association of social factors and time spent in the NICU for mothers of very preterm infants. Hosp Pediatr. 2021;11:988–96.
Whitehill L, Smith J, Colditz G, Le T, Kellner P, Pineda R. Socio-demographic factors related to parent engagement in the NICU and the impact of the SENSE program. Early Hum Dev. 2021;163:105486.
Ferreira A, Ferretti E, Curtis K, Joly C, Sivanthan M, Major N, et al. Parents’ views to strengthen partnerships in newborn intensive care. Front Pediatr. 2021;9:721835.
Acknowledgements
We would like to thank the UCH NICU nurses and staff for participation in this quality improvement initiative. We would also like to thank UCH IT teams for creating solutions to integrate virtual care visits into patient portals.
Funding
This quality improvement initiative was funded by the University of Colorado Hospital Clinical Effectiveness & Patient Safety (CEPS) Grant Program and the University Hills Rotary Club. Jacob Holzman, PhD was supported by the National Institute of Mental Health (NIMH) 1K23MH134189. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Contributions
All author contributions are described using the CRediT (Contributor Roles Taxonomy) system. JK: conceptualization, methodology, investigation, writing—original draft, writing—review and editing. DC: conceptualization, investigation, data curation, and writing—review and editing. JH: formal analysis, data curation, visualization, writing—original draft, and writing—review and editing. AS: visualization, data curation, project administration, and validation. KH: data curation, validation, and investigation. SS: writing—original draft. LB: conceptualization and supervision. JB: funding acquisition and conceptualization. JD: data curation, visualization, and formal analysis. AD: conceptualization, funding acquisition, supervision, and writing—review and editing.
Corresponding author
Ethics declarations
Competing interests
JB has been involved with content creation as Topic Co-Lead for the AI and Technology Forum on Healio Inc. and serves as the Site Co-Investigator for Aerofact Phase IIb clinical trial for Aerofact Inc. No other authors have conflicts of interest related to information presented in this manuscript to disclose.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kelleher, J., Cooke, D., Holzman, J.B.W. et al. A quality improvement initiative to increase family engagement and reduce disparities in visitation via telehealth in a level III neonatal intensive care unit. J Perinatol (2026). https://doi.org/10.1038/s41372-025-02527-3
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41372-025-02527-3