Abstract
Background
BPD, ROP, brain injury (severe IVH or PVL), NEC, and sepsis are independently associated with neurodevelopmental impairment (NDI).
Objectives
Evaluate the contribution of BPD, ROP, brain injury, NEC, and sepsis, individually or in combination with BPD, on NDI at 18-24 months corrected age (CA).
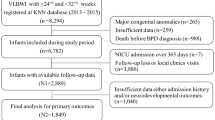
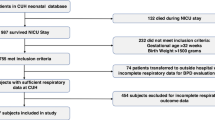
Methods
Demographic, NICU, and follow-up data from infants born ≤32 weeks gestational age with a birth weight <1500 grams were collected. NDI at 18–24 months CA was defined as blindness, deafness, or a composite score of <85 on the BSID-III. Univariate testing and logistic regression models were used.
Results
Univariate analysis revealed a significant association between moderate and severe BPD, brain injury, NEC, and ROP with NDI. Logistic regression showed infants with brain injury or NEC had significantly greater odds of developing NDI.
Conclusions
BPD with brain injury or NEC increases the risk of NDI. Infants with ≥3 comorbidities had significantly higher odds of NDI.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The data analyzed in this study is not publicly available. Datasets are available from the corresponding author upon reasonable request.
References
Harrison MS, Goldenberg RL. Global burden of prematurity. Semin Fetal Neonatal Med. 2016;21:74–9.
Donlon J, Bhat V, Hunter K, Kushnir A, Bhandari V. Impact of severity and age with variable definitions of bronchopulmonary dysplasia on neurodevelopmental outcomes. Pediatr Res. 2024;96:1243–50.
Dogra MR, Katoch D, Dogra M. An Update on Retinopathy of Prematurity (ROP). Indian J Pediatr. 2017;84:930–6.
Uberos J, Nieto-Ruiz A, Contreras Chova F, Carrasco-Solis M, Ruiz-Lopez A, Fernandez-Marin E, et al. Late Neonatal Sepsis in Very-low-birth-weight Premature Newborns Is Associated With Alterations in Neurodevelopment at Twenty-five Months of Age. Pediatr Infect Dis J. 2024;43:550–5.
Ballabh P. Intraventricular hemorrhage in premature infants: mechanism of disease. Pediatr Res. 2010;67:1–8.
Jones IH, Hall NJ. Contemporary Outcomes for Infants with Necrotizing Enterocolitis-A Systematic Review. J Pediatr. 2020;220:86–92 e3.
Fang L, Wang C, Yang Y, Feng J, Chen F. A meta-analysis of adverse effects of retinopathy of prematurity on neurodevelopment in preterm infants. Medicine. 2023;102:e36557.
Gilfillan M, Bhandari A, Bhandari V. Diagnosis and management of bronchopulmonary dysplasia. BMJ. 2021;375:n1974.
Scheese DJ, Sodhi CP, Hackam DJ. New insights into the pathogenesis of necrotizing enterocolitis and the dawn of potential therapeutics. Semin Pediatr Surg. 2023;32:151309.
Balany J, Bhandari V. Understanding the Impact of Infection, Inflammation, and Their Persistence in the Pathogenesis of Bronchopulmonary Dysplasia. Front Med. 2015;2:90.
Malavolti AM, Bassler D, Arlettaz-Mieth R, Faldella G, Latal B, Natalucci G. Bronchopulmonary dysplasia-impact of severity and timing of diagnosis on neurodevelopment of preterm infants: a retrospective cohort study. BMJ Paediatr Open. 2018;2:e000165.
Han YS, Kim SH, Sung TJ. Impact of the definition of bronchopulmonary dysplasia on neurodevelopmental outcomes. Sci Rep. 2021;11:22589.
Rees P, Callan C, Chadda KR, Vaal M, Diviney J, Sabti S, et al. Preterm Brain Injury and Neurodevelopmental Outcomes: A Meta-analysis. Pediatrics 2022;150:e2022057442.
Shah DK, Doyle LW, Anderson PJ, Bear M, Daley AJ, Hunt RW, et al. Adverse neurodevelopment in preterm infants with postnatal sepsis or necrotizing enterocolitis is mediated by white matter abnormalities on magnetic resonance imaging at term. J Pediatr. 2008;153:170–5, 5 e1.
Nguyen KL, Fitzgerald DA, Webb A, Bajuk B, Popat H. Neurodevelopmental outcomes of extremely preterm infants with bronchopulmonary dysplasia (BPD) - A retrospective cohort study. Paediatr Respir Rev. 2024;50:23–30.
Jensen EA, Dysart K, Gantz MG, McDonald S, Bamat NA, Keszler M, et al. The Diagnosis of Bronchopulmonary Dysplasia in Very Preterm Infants. An Evidence-based Approach. Am J Respir Crit Care Med. 2019;200:751–9.
Jobe AH, Bancalari E. Bronchopulmonary dysplasia. Am J Respir Crit Care Med. 2001;163:1723–9.
Katz TA, van Kaam AH, Schuit E, Mugie SM, Aarnoudse-Moens CSH, Weber EH, et al. Comparison of New Bronchopulmonary Dysplasia Definitions on Long-Term Outcomes in Preterm Infants. J Pediatr. 2023;253:86–93 e4.
Katz TA, van Kaam AH, Zuithoff NPA, Mugie SM, Beuger S, Blok GJ, et al. Association between bronchopulmonary dysplasia severity and its risk factors and long-term outcomes in three definitions: a historical cohort study. Arch Dis Child Fetal Neonatal Ed. 2024;110:51–6.
Lingasubramanian G, Hum CE, Hunter K, Mehta R, Bhandari V. Timing and risk factors associated with acute kidney injury in infants with necrotizing enterocolitis. J Perinatol. 2024;44:1774–9.
Sheth S, Goto L, Bhandari V, Abraham B, Mowes A. Factors associated with development of early and late pulmonary hypertension in preterm infants with bronchopulmonary dysplasia. J Perinatol. 2020;40:138–48.
Bizzarro MJ, Li FY, Katz K, Shabanova V, Ehrenkranz RA, Bhandari V. Temporal quantification of oxygen saturation ranges: an effort to reduce hyperoxia in the neonatal intensive care unit. J Perinatol. 2014;34:33–8.
Bayley N. Bayley Scales of Infant and Toddler Development 3rd Edition: Screening Test Manual. San Antonio, TX: Harcourt Assessment, Inc. 2006. https://doi.org/10.1037/t14978-000.
Celik P, Ayranci Sucakli I, Yakut HI. Which Bayley-III cut-off values should be used in different developmental levels?. Turk J Med Sci. 2020;50:764–70.
Johnson S, Moore T, Marlow N. Using the Bayley-III to assess neurodevelopmental delay: which cut-off should be used?. Pediatr Res. 2014;75:670–4.
Bauer SE, Schneider L, Lynch SK, Malleske DT, Shepherd EG, Nelin LD. Factors Associated with Neurodevelopmental Impairment in Bronchopulmonary Dysplasia. J Pediatr. 2020;218:22–7 e2.
Katz TA, van Kaam AH, Mugie SM, Aarnoudse-Moens CSH, de Groof F, van Kempen A, et al. Risk Factors for Neurodevelopmental Impairment at 2- and 5-Years Corrected Age in Preterm Infants with Established Bronchopulmonary Dysplasia. Neonatology. 2024;121:125–32.
Decollogne L, Epiard C, Chevallier M, Ego A, Alin L, Debillon T. Neurodevelopmental impairment at 2 years of age in children born before 29 weeks’ gestation with bronchopulmonary dysplasia. Arch Pediatr. 2021;28:23–8.
Bae SP, Shin SH, Yoon YM, Kim EK, Kim HS. Association of Severe Retinopathy of Prematurity and Bronchopulmonary Dysplasia with Adverse Neurodevelopmental Outcomes in Preterm Infants without Severe Brain Injury. Brain Sci 2021;11:699.
Yazici A, Buyuktiryaki M, Simsek GK, Kanmaz Kutman HG, Canpolat FE. Factors associated with neurodevelopmental impairment in preterm infants with bronchopulmonary dysplasia. Eur Rev Med Pharmacol Sci. 2022;26:1579–85.
van Roode T, Sharples K, Dickson N, Paul C. Life-Course Relationship between Socioeconomic Circumstances and Timing of First Birth in a Birth Cohort. PLoS One. 2017;12:e0170170.
Duncan GJ, Lee KTH, Rosales-Rueda M, Kalil A. Maternal Age and Child Development. Demography. 2018;55:2229–55.
Locke A, Kanekar S. Imaging of Premature Infants. Clin Perinatol. 2022;49:641–55.
Acknowledgements
The authors would like to thank Dr. Elizabeth R. Saslow, PhD, the developmental psychologist who conducted BSID-III assessments.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Author information
Authors and Affiliations
Contributions
Concept and design: Bhat and Bhandari; Acquisition, analysis, and interpretation of data: Donlon, Hawkins, Bhat, Hunter, Kushnir, Bhandari; Statistical analysis: Hunter; Initial draft of the manuscript: Donlon; Revision of manuscript: Donlon, Hawkins, Bhat, Hunter, Kushnir, Bhandari.
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no conflicts of interest.
Ethics statement
All methods were performed in accordance with the relevant guidelines and regulations.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Donlon, J., Hawkins, K., Bhat, V. et al. Impact of bronchopulmonary dysplasia, brain injury, necrotizing enterocolitis, retinopathy of prematurity and sepsis on neurodevelopmental outcomes in premature infants. J Perinatol (2025). https://doi.org/10.1038/s41372-025-02549-x
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41372-025-02549-x