Abstract
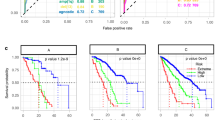
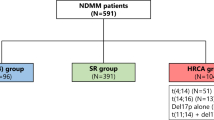
The cytogenetic abnormalities translocations t(4;14) and t(14;16) and the deletion of chromosome 17p in newly-diagnosed multiple myeloma are associated with poor disease prognosis and are traditionally deemed as “high-risk”. However, in the setting of relapsed/refractory multiple myeloma (RRMM) their effect is less characterized. A systematic search was conducted in the PubMed database (end-of-search: 20 August 2024) for randomized controlled trials on anti-myeloma therapies for RRMM that reported outcomes for standard-risk and high-risk patient subgroups. A total of 28 studies were included; 23 reported progression-free survival (PFS) and 8 overall survival (OS) outcomes. Per overall analysis, high-risk cytogenetics were not associated with impaired treatment efficacy compared to standard-risk in terms of both PFS and OS. Among 9 treatment subgroups, high-risk patients on anti-BCMA therapies seemed to exhibit a 18% lower risk of a PFS event compared to the overall treatment effect for this population, but results were not significant. In the subgroup analyses, deletion 17p seemed to have the biggest impact on treatment efficacy, but results were not statistically significant. Overall, the presence of high-risk cytogenetics at study entry in RRMM did not alter treatment efficacy. Novel tools are needed to improve risk stratification at myeloma relapse.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
Data available upon request from the corresponding author.
References
Palumbo A, Anderson K. Multiple myeloma. N Engl J Med. 2011;364:1046–60. https://doi.org/10.1056/NEJMra1011442.
Rajkumar SV, Dimopoulos MA, Palumbo A, Blade J, Merlini G, Mateos MV, et al. International Myeloma Working Group updated criteria for the diagnosis of multiple myeloma. Lancet Oncol. 2014;15:e538–48. https://doi.org/10.1016/S1470-2045(14)70442-5.
Avet-Loiseau H, Magrangeas F, Moreau P, Attal M, Facon T, Anderson K, et al. Molecular heterogeneity of multiple myeloma: pathogenesis, prognosis, and therapeutic implications. J Clin Oncol. 2011;29:1893–7. https://doi.org/10.1200/JCO.2010.32.8435.
Morgan GJ, Walker BA, Davies FE. The genetic architecture of multiple myeloma. Nat Rev Cancer. 2012;12:335–48. https://doi.org/10.1038/nrc3257.
Fonseca R, Barlogie B, Bataille R, Bastard C, Bergsagel PL, Chesi M, et al. Genetics and cytogenetics of multiple myeloma: a workshop report. Cancer Res. 2004;64:1546–58. https://doi.org/10.1158/0008-5472.can-03-2876.
Fonseca R, Bergsagel PL, Drach J, Shaughnessy J, Gutierrez N, Stewart AK, et al. International Myeloma Working Group. International Myeloma Working Group molecular classification of multiple myeloma: spotlight review. Leukemia. 2009;23:2210–21. https://doi.org/10.1038/leu.2009.174.
Fonseca R, Blood E, Rue M, Harrington D, Oken MM, Kyle RA, et al. Clinical and biologic implications of recurrent genomic aberrations in myeloma. Blood. 2003;101:4569–75. https://doi.org/10.1182/blood-2002-10-3017.
Smallbone P, Clugston S, De Kraa R, Purtill D, Wright M, Leahy MF, et al. Presence of Multiple High Risk Cytogenetic Abnormalities Is Associated with Rapid Progression and Shorter Survival in Newly Diagnosed Multiple Myeloma. Blood. 2020;136:23. https://doi.org/10.1182/blood-2020-141783.
Skerget S, Penaherrera D, Chari A, Jagannath S, Siegel DS, Vij R, et al. Comprehensive molecular profiling of multiple myeloma identifies refined copy number and expression subtypes. Nat Genet. 2024. https://doi.org/10.1038/s41588-024-01853-0.
Verma R, Kumar L, Gupta R, Halder A, Sharma A, Saxena R. Impact of cytogenetics on clinical outcome in multiple myeloma: A risk stratification model. JCO. 2011;29:e18576–e18576. https://doi.org/10.1200/jco.2011.29.15_suppl.e18576.
Munshi NC, Anderson KC, Bergsagel PL, Shaughnessy J, Palumbo A, Durie B, et al. International Myeloma Workshop Consensus Panel 2. Consensus recommendations for risk stratification in multiple myeloma: report of the International Myeloma Workshop Consensus Panel 2. Blood. 2011;117:4696–700. https://doi.org/10.1182/blood-2010-10-300970.
Sonneveld P, Avet-Loiseau H, Lonial S, Usmani S, Siegel D, Anderson KC, et al. Treatment of multiple myeloma with high-risk cytogenetics: a consensus of the International Myeloma Working Group. Blood. 2016;127:2955–62. https://doi.org/10.1182/blood-2016-01-631200.
Kapoor P, Kumar S, Fonseca R, Lacy MQ, Witzig TE, Hayman SR, et al. Impact of risk stratification on outcome among patients with multiple myeloma receiving initial therapy with lenalidomide and dexamethasone. Blood. 2009;114:518–21. https://doi.org/10.1182/blood-2009-01-202010.
Ntanasis-Stathopoulos I, Gavriatopoulou M, Kastritis E, Terpos E, Dimopoulos MA. Multiple myeloma: Role of autologous transplantation. Cancer Treat Rev. 2020;82:101929. https://doi.org/10.1016/j.ctrv.2019.101929.
Dimopoulos MA, Moreau P, Terpos E, Mateos MV, Zweegman S, Cook G, et al. Multiple Myeloma: EHA-ESMO Clinical Practice Guidelines for Diagnosis, Treatment and Follow-up. Hemasphere. 2021;5:e528. https://doi.org/10.1097/HS9.0000000000000528.
Terpos E, Ntanasis-Stathopoulos I, Gavriatopoulou M, Katodritou E, Hatjiharissi E, Malandrakis P, et al. Efficacy and safety of daratumumab with ixazomib and dexamethasone in lenalidomide-exposed patients after one prior line of therapy: Final results of the phase 2 study DARIA. Am J Hematol. 2024;99:396–407. https://doi.org/10.1002/ajh.27206.
Raab MS, Zamagni E, Manier S, Rodriguez-Otero P, Schjesvold F, Broijl A. Difficult-to-treat patients with relapsed/refractory multiple myeloma: A review of clinical trial results. EJHaem. 2023;4:1117–31. https://doi.org/10.1002/jha2.743.
Caro J, Al Hadidi S, Usmani S, Yee AJ, Raje N, Davies FE. How to Treat High-Risk Myeloma at Diagnosis and Relapse. Am Soc Clin Oncol Educ Book. 2021;41:291–309. https://doi.org/10.1200/EDBK_320105.
Higgins JP. Cochrane handbook for systematic reviews of interventions version 5.0. 1. The Cochrane Collaboration. http://www.cochrane-handbook.org. 2008.
Sterne JA, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 28;366. (2019)
Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. bmj. 1997;315:629–34.
Sterne JA, Egger M. Funnel plots for detecting bias in meta-analysis: guidelines on choice of axis. J Clin Epidemiol. 2001;54:1046–55.
Duval S, Tweedie R. Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000;56:455–63. https://doi.org/10.1111/j.0006-341x.2000.00455.x.
Richardson PG, Kumar SK, Masszi T, Grzasko N, Bahlis NJ, Hansson M, et al. Final Overall Survival Analysis of the TOURMALINE-MM1 Phase III Trial of Ixazomib, Lenalidomide, and Dexamethasone in Patients With Relapsed or Refractory Multiple Myeloma. J Clin Oncol. 2021;39:2430–42. https://doi.org/10.1200/JCO.21.00972.
Avet-Loiseau H, Bahlis NJ, Chng WJ, Masszi T, Viterbo L, Pour L, et al. Ixazomib significantly prolongs progression-free survival in high-risk relapsed/refractory myeloma patients. Blood. 2017;130:2610–8. https://doi.org/10.1182/blood-2017-06-791228.
Fu W, Li W, Hu J, An G, Wang Y, Fu C, et al. Daratumumab, Bortezomib, and Dexamethasone versus Bortezomib and Dexamethasone in Chinese Patients With Relapsed or Refractory Multiple Myeloma: Updated Analysis of LEPUS. Clin Lymphoma Myeloma Leuk. 2023;23:e51–e58. https://doi.org/10.1016/j.clml.2022.10.007.
Avet-Loiseau H, Fonseca R, Siegel D, Dimopoulos MA, Špička I, Masszi T, et al. Carfilzomib significantly improves the progression-free survival of high-risk patients in multiple myeloma. Blood. 2016;128:1174–80. https://doi.org/10.1182/blood-2016-03-707596.
Kaufman JL, Dimopoulos MA, White D, Benboubker L, Cook G, Leiba M, et al. Daratumumab, lenalidomide, and dexamethasone in relapsed/refractory myeloma: a cytogenetic subgroup analysis of POLLUX. Blood Cancer J. 2020;10:111 https://doi.org/10.1038/s41408-020-00375-2.
Richard S, Chari A, Delimpasi S, Simonova M, Spicka I, Pour L, et al. Selinexor, bortezomib, and dexamethasone versus bortezomib and dexamethasone in previously treated multiple myeloma: Outcomes by cytogenetic risk. Am J Hematol. 2021;96:1120–30. https://doi.org/10.1002/ajh.26261.
Richardson PG, Perrot A, San-Miguel J, Beksac M, Spicka I, Leleu X, et al. Isatuximab plus pomalidomide and low-dose dexamethasone versus pomalidomide and low-dose dexamethasone in patients with relapsed and refractory multiple myeloma (ICARIA-MM): follow-up analysis of a randomised, phase 3 study. Lancet Oncol 2022;23:416–27. https://doi.org/10.1016/S1470-2045(22)00019-5.
Richardson PG, Harrison SJ, Bringhen S, Schjesvold F, Yong K, Campana F, et al. Isatuximab for relapsed/refractory multiple myeloma: review of key subgroup analyses from the Phase III ICARIA-MM study. Future Oncol. 2021;17:4797–812. https://doi.org/10.2217/fon-2021-0568.
Weisel K, Spencer A, Lentzsch S, Avet-Loiseau H, Mark TM, Spicka I, et al. Daratumumab, bortezomib, and dexamethasone in relapsed or refractory multiple myeloma: subgroup analysis of CASTOR based on cytogenetic risk. J Hematol Oncol. 2020;13:115 https://doi.org/10.1186/s13045-020-00948-5.
Chng WJ, Goldschmidt H, Dimopoulos MA, Moreau P, Joshua D, Palumbo A, et al. Carfilzomib-dexamethasone vs bortezomib-dexamethasone in relapsed or refractory multiple myeloma by cytogenetic risk in the phase 3 study ENDEAVOR. Leukemia. 2017;31:1368–74. https://doi.org/10.1038/leu.2016.390.
Miguel JS, Weisel K, Moreau P, Lacy M, Song K, Delforge M, et al. Pomalidomide plus low-dose dexamethasone versus high-dose dexamethasone alone for patients with relapsed and refractory multiple myeloma (MM-003): a randomised, open-label, phase 3 trial. Lancet Oncol. 2013;14:1055–66. https://doi.org/10.1016/S1470-2045(13)70380-2.
Hungria V, Robak P, Hus M, Zherebtsova V, Ward C, Ho PJ, et al. DREAMM-7 Investigators. Belantamab Mafodotin, Bortezomib, and Dexamethasone for Multiple Myeloma. N Engl J Med. 2024;391:393–407. https://doi.org/10.1056/NEJMoa2405090.
Dimopoulos MA, Beksac M, Pour L, Delimpasi S, Vorobyev V, Quach H, et al. DREAMM-8 Investigators. Belantamab Mafodotin, Pomalidomide, and Dexamethasone in Multiple Myeloma. N Engl J Med. 2024;391:408–21. https://doi.org/10.1056/NEJMoa2403407.
Rodriguez-Otero P, Ailawadhi S, Arnulf B, Patel K, Cavo M, Nooka AK, et al. Ide-cel or Standard Regimens in Relapsed and Refractory Multiple Myeloma. N Engl J Med. 2023;388:1002–14. https://doi.org/10.1056/NEJMoa2213614.
San-Miguel J, Dhakal B, Yong K, Spencer A, Anguille S, Mateos MV, et al. Cilta-cel or Standard Care in Lenalidomide-Refractory Multiple Myeloma. N Engl J Med. 2023;389:335–47. https://doi.org/10.1056/NEJMoa2303379.
Usmani SZ, Quach H, Mateos MV, Landgren O, Leleu X, Siegel D, et al. Carfilzomib, dexamethasone, and daratumumab versus carfilzomib and dexamethasone for patients with relapsed or refractory multiple myeloma (CANDOR): updated outcomes from a randomised, multicentre, open-label, phase 3 study. Lancet Oncol. 2022;23:65–76. https://doi.org/10.1016/S1470-2045(21)00579-9.
Richardson PG, Oriol A, Beksac M, Liberati AM, Galli M, Schjesvold F, et al. OPTIMISMM trial investigators. Pomalidomide, bortezomib, and dexamethasone for patients with relapsed or refractory multiple myeloma previously treated with lenalidomide (OPTIMISMM): a randomised, open-label, phase 3 trial. Lancet Oncol. 2019;20:781–94. https://doi.org/10.1016/S1470-2045(19)30152-4.
Moreau P, Dimopoulos MA, Mikhael J, Yong K, Capra M, Facon T, et al. IKEMA study group. Isatuximab, carfilzomib, and dexamethasone in relapsed multiple myeloma (IKEMA): a multicentre, open-label, randomised phase 3 trial. Lancet. 2021;397:2361–71. https://doi.org/10.1016/S0140-6736(21)00592-4.
Dimopoulos MA, Dytfeld D, Grosicki S, Moreau P, Takezako N, Hori M, et al. Elotuzumab Plus Pomalidomide and Dexamethasone for Relapsed/Refractory Multiple Myeloma: Final Overall Survival Analysis From the Randomized Phase II ELOQUENT-3 Trial. J Clin Oncol. 2023;41:568–78. https://doi.org/10.1200/JCO.21.02815.
Kumar SK, Harrison SJ, Cavo M, de la Rubia J, Popat R, Gasparetto C, et al. Venetoclax or placebo in combination with bortezomib and dexamethasone in patients with relapsed or refractory multiple myeloma (BELLINI): a randomised, double-blind, multicentre, phase 3 trial. Lancet Oncol. 2020;21:1630–42. https://doi.org/10.1016/S1470-2045(20)30525-8.
Xia Z, Leng Y, Fang B, Liang Y, Li W, Fu C, et al. Aponermin or placebo in combination with thalidomide and dexamethasone in the treatment of relapsed or refractory multiple myeloma (CPT-MM301): a randomised, double-blinded, placebo-controlled, phase 3 trial. BMC Cancer. 2023;23:980 https://doi.org/10.1186/s12885-023-11489-8.
Schjesvold FH, Dimopoulos MA, Delimpasi S, Robak P, Coriu D, Legiec W, et al. OCEAN (OP-103) Investigators. Melflufen or pomalidomide plus dexamethasone for patients with multiple myeloma refractory to lenalidomide (OCEAN): a randomised, head-to-head, open-label, phase 3 study. Lancet Haematol. 2022;9:e98–e110. https://doi.org/10.1016/S2352-3026(21)00381-1.
San-Miguel JF, Hungria VT, Yoon SS, Beksac M, Dimopoulos MA, Elghandour A, et al. Panobinostat plus bortezomib and dexamethasone versus placebo plus bortezomib and dexamethasone in patients with relapsed or relapsed and refractory multiple myeloma: a multicentre, randomised, double-blind phase 3 trial. Lancet Oncol. 2014;15:1195–206. https://doi.org/10.1016/S1470-2045(14)70440-1.
Siegel DS, Dimopoulos MA, Ludwig H, Facon T, Goldschmidt H, Jakubowiak A, et al. Improvement in Overall Survival With Carfilzomib, Lenalidomide, and Dexamethasone in Patients With Relapsed or Refractory Multiple Myeloma. J Clin Oncol. 2018;36:728–34. https://doi.org/10.1200/JCO.2017.76.5032.
San-Miguel JF, Hungria VT, Yoon SS, Beksac M, Dimopoulos MA, Elghandour A, et al. Overall survival of patients with relapsed multiple myeloma treated with panobinostat or placebo plus bortezomib and dexamethasone (the PANORAMA 1 trial): a randomised, placebo-controlled, phase 3 trial. Lancet Haematol. 2016;3:e506–e515. https://doi.org/10.1016/S2352-3026(16)30147-8.
Dimopoulos MA, Hungria VTM, Radinoff A, Delimpasi S, Mikala G, Masszi T, et al. Efficacy and safety of single-agent belantamab mafodotin versus pomalidomide plus low-dose dexamethasone in patients with relapsed or refractory multiple myeloma (DREAMM-3): a phase 3, open-label, randomised study. Lancet Haematol. 2023;10:e801–e812. https://doi.org/10.1016/S2352-3026(23)00243-0.
Dimopoulos MA, Dytfeld D, Grosicki S, Moreau P, Takezako N, Hori M, et al. Elotuzumab plus Pomalidomide and Dexamethasone for Multiple Myeloma. N Engl J Med. 2018;379:1811–22. https://doi.org/10.1056/NEJMoa1805762.
Dimopoulos MA, Terpos E, Boccadoro M, Delimpasi S, Beksac M, Katodritou E, et al. APOLLO Trial Investigators. Daratumumab plus pomalidomide and dexamethasone versus pomalidomide and dexamethasone alone in previously treated multiple myeloma (APOLLO): an open-label, randomised, phase 3 trial. Lancet Oncol. 2021;22:801–12. https://doi.org/10.1016/S1470-2045(21)00128-5.
Sammartano V, Franceschini M, Fredducci S, Caroni F, Ciofini S, Pacelli P, et al. Anti-BCMA novel therapies for multiple myeloma. Cancer Drug Resist. 2023;6:169–81. https://doi.org/10.20517/cdr.2022.138.
Raje N, Berdeja J, Lin Y, Siegel D, Jagannath S, Madduri D, et al. Anti-BCMA CAR T-Cell Therapy bb2121 in Relapsed or Refractory Multiple Myeloma. N Engl J Med. 2019;380:1726–37. https://doi.org/10.1056/NEJMoa1817226.
Berdeja JG, Madduri D, Usmani SZ, Jakubowiak A, Agha M, Cohen AD, et al. Ciltacabtagene autoleucel, a B-cell maturation antigen-directed chimeric antigen receptor T-cell therapy in patients with relapsed or refractory multiple myeloma (CARTITUDE-1): a phase 1b/2 open-label study. Lancet. 2021;398:314–24. https://doi.org/10.1016/S0140-6736(21)00933-8.
Lonial S, Lee HC, Badros A, Trudel S, Nooka AK, Chari A, et al. Belantamab mafodotin for relapsed or refractory multiple myeloma (DREAMM-2): a two-arm, randomised, open-label, phase 2 study. Lancet Oncol. 2020;21:207–21. https://doi.org/10.1016/S1470-2045(19)30788-0.
Mei H, Li C, Jiang H, Zhao X, Huang Z, Jin D, et al. A bispecific CAR-T cell therapy targeting BCMA and CD38 in relapsed or refractory multiple myeloma. J Hematol Oncol. 2021;14:161 https://doi.org/10.1186/s13045-021-01170-7.
de la Rubia J, Alonso R, Clavero ME, Askari E, García A, Antón C, et al. Belantamab Mafodotin in Patients with Relapsed/Refractory Multiple Myeloma: Results of the Compassionate Use or the Expanded Access Program in Spain. Cancers (Basel). 2023;15:2964 https://doi.org/10.3390/cancers15112964.
Hultcrantz M, Derkach A, Hassoun H, Korde N, Maclachla KH, Mailankody S, et al. Belantamab Mafodotin in Patients with Relapsed/Refractory Multiple Myeloma, a Real-World Single Center Experience. Blood. 2022;140:7246–8. https://doi.org/10.1182/blood-2022-171077.
Hultcrantz M, Kleinman D, Vij R, Escalante F, Delforge M, Kotowsky N, et al. PB2114: Belantamab mafodotin for relapsed/refractory multiple myeloma: a real-world observational study update. Hemasphere. 2023;7:e20009f4 https://doi.org/10.1097/01.HS9.0000975232.20009.f4.
Wang Q, Wei R, Guo S, Min C, Zhong X, Huang H, et al. An alternative fully human anti-BCMA CAR-T shows response for relapsed or refractory multiple myeloma with anti-BCMA CAR-T exposures previously. Cancer Gene Ther. 2024;31:420–6. https://doi.org/10.1038/s41417-023-00712-0.
Mateos MV, Moreau P, Dimopoulos MA, Hong WJ, Cooper S, Yu Y, et al. A phase III, randomized, multicenter, open-label study of venetoclax or pomalidomide in combination with dexamethasone in patients with t(11;14)-positive relapsed/refractory multiple myeloma. JCO. 2020;38:TPS8554–TPS8554. https://doi.org/10.1200/JCO.2020.38.15_suppl.TPS8554.
Bahlis NJ, Baz R, Harrison SJ, Quach H, Ho SJ, Vangsted AJ, et al. Phase I Study of Venetoclax Plus Daratumumab and Dexamethasone, With or Without Bortezomib, in Patients With Relapsed or Refractory Multiple Myeloma With and Without t(11;14). J Clin Oncol. 2021;39:3602–12. https://doi.org/10.1200/JCO.21.00443.
Kumar S, Kaufman JL, Gasparetto C, Mikhael J, Vij R, Pegourie B, et al. Efficacy of venetoclax as targeted therapy for relapsed/refractory t(11;14) multiple myeloma. Blood. 2017;130:2401–9. https://doi.org/10.1182/blood-2017-06-788786.
Kaufman JL, Gasparetto C, Schjesvold FH, Moreau P, Touzeau C, Facon T, et al. Targeting BCL-2 with venetoclax and dexamethasone in patients with relapsed/refractory t(11;14) multiple myeloma. Am J Hematol. 2021;96:418–27. https://doi.org/10.1002/ajh.26083.
Giesen N, Paramasivam N, Toprak UH, Huebschmann D, Xu J, Uhrig S, et al. Comprehensive genomic analysis of refractory multiple myeloma reveals a complex mutational landscape associated with drug resistance and novel therapeutic vulnerabilities. Haematologica. 2022;107:1891–901. https://doi.org/10.3324/haematol.2021.279360.
Vo JN, Wu YM, Mishler J, Hall S, Mannan R, Wang L, et al. Multiple Myeloma Research Consortium; Bergsagel PL, Auclair D, Cho HJ, Robinson DR, Chinnaiyan AM. The genetic heterogeneity and drug resistance mechanisms of relapsed refractory multiple myeloma. Nat Commun. 2022;13:3750 https://doi.org/10.1038/s41467-022-31430-0.
Durer C, Durer S, Lee S, Chakraborty R, Malik MN, Rafae A, et al. Treatment of relapsed multiple myeloma: Evidence-based recommendations. Blood Rev. 2020;39:100616 https://doi.org/10.1016/j.blre.2019.100616.
Hernández-Rivas JÁ, Ríos-Tamayo R, Encinas C, Alonso R, Lahuerta JJ. The changing landscape of relapsed and/or refractory multiple myeloma (MM): fundamentals and controversies. Biomark Res. 2022;10:1 https://doi.org/10.1186/s40364-021-00344-2.
Cornell RF, Kassim AA. Evolving paradigms in the treatment of relapsed/refractory multiple myeloma: increased options and increased complexity. Bone Marrow Transpl. 2016;51:479–91. https://doi.org/10.1038/bmt.2015.307.
Jeryczynski G, Bolomsky A, Agis H, Krauth MT. Stratification for RRMM and Risk-Adapted Therapy: Sequencing of Therapies in RRMM. Cancers (Basel). 2021;13:5886 https://doi.org/10.3390/cancers13235886.
Zhou X, Hofmann A, Vogt C, Nerreter S, Teufel E, Stanojkovska E, et al. Advanced Risk Stratification in Multiple Myeloma Beyond Traditional FISH: The First Prospective Real-World Evidence for SKY92 Gene Expression Profiling. Blood. 2022;140:4273–4. https://doi.org/10.1182/blood-2022-163848.
Zhou X, Hofmann A, Vogt C, Nerreter S, Teufel E, Stanojkovska E, et al. P52 Risk stratification combining SKY92 Gene expression profiling and traditional fish in multiple myeloma: the first prospective evidence in the R2-ISS era. Hemasphere. 2023;7:39.
Richter J, Wang PF, Molinari A, Gorsh B, Boytsov N, Landi S, et al. Treatment Patterns and Patient Outcomes in Relapsed/Refractory Multiple Myeloma (RRMM) Stratified By Exposure to Lenalidomide or Anti-CD38 Therapy and Double-Class Refractory Status: A Retrospective Electronic Health Record Database Study. Blood. 2022;140:4338–40. https://doi.org/10.1182/blood-2022-164918.
Kastritis E, Migkou M, Dalampira D, Gavriatopoulou M, Fotiou D, Roussou M, et al. Chromosome 1q21 aberrations identify ultra high-risk myeloma with prognostic and clinical implications. Am J Hematol. 2022;97:1142–9. https://doi.org/10.1002/ajh.26639.
Weinhold N, Salwender HJ, Cairns DA, Raab MS, Waldron G, Blau IW, et al. Chromosome 1q21 abnormalities refine outcome prediction in patients with multiple myeloma - a meta-analysis of 2,596 trial patients. Haematologica. 2021;106:2754–8. https://doi.org/10.3324/haematol.2021.278888.
D’Agostino M, Cairns DA, Lahuerta JJ, Wester R, Bertsch U, Waage A, et al. Second Revision of the International Staging System (R2-ISS) for Overall Survival in Multiple Myeloma: A European Myeloma Network (EMN) Report Within the HARMONY Project. J Clin Oncol. 2022;40:3406–18. https://doi.org/10.1200/JCO.21.02614.
Kaiser MF, Phillip R, Hall A, Holroyd A, Bevington L, de Tute RM, et al. Ultra High-Risk Multiple Myeloma Patients with Multi-Hit Tumours and SKY92 High Risk Signature Are at Increased Risk of Early Relapse Even When Treated with Extended Intensified Induction and Consolidation - Results from the Optimum/Muknine Trial. Blood. 2023;142:881 https://doi.org/10.1182/blood-2023-177896.
Corre J et al. oral presentation, IMS 2024
Rasche L, Chavan SS, Stephens OW, Patel PH, Tytarenko R, Ashby C, et al. Spatial genomic heterogeneity in multiple myeloma revealed by multi-region sequencing. Nat Commun. 2017;8:268. https://doi.org/10.1038/s41467-017-00296-y.
Sonneveld P. Management of multiple myeloma in the relapsed/refractory patient. Hematol Am Soc Hematol Educ Program. 2017;2017:508–17. https://doi.org/10.1182/asheducation-2017.1.508.
Rajkumar SV. Multiple myeloma: 2024 update on diagnosis, risk-stratification, and management. Am J Hematol. 2024;99:1802–24. https://doi.org/10.1002/ajh.27422.
Miething CC. Clonal evolution in myeloma: a narrow road to remission. Haematologica. 2019;104:1292–3. https://doi.org/10.3324/haematol.2019.220152.
Toenges R, Alberge JB, Corrado F, Bidikian N, Dos Santos DMC, Dutta AK, et al. Single-Cell Whole-Genome Sequencing of Circulating Tumor Cells in Relapsed/Refractory Multiple Myeloma Patients Receiving BCMA- or GPRC5D-Targeted Immunotherapies. Blood. 2024;144:492 https://doi.org/10.1182/blood-2024-204132. (Supplement 1).
Ntanasis-Stathopoulos I, Filippatos C, Ntanasis-Stathopoulos A, Malandrakis P, Kastritis E, Tsitsilonis OE, et al. Evaluating Minimal Residual Disease Negativity as a Surrogate Endpoint for Treatment Efficacy in Multiple Myeloma: A Meta-Analysis of Randomized Controlled Trials. Am J Hematol. 2025;100:427–38. https://doi.org/10.1002/ajh.27582.
Zhong H, Huang D, Wu J, Chen X, Chen Y, Huang C. 18F‑FDG PET/CT based radiomics features improve prediction of prognosis: multiple machine learning algorithms and multimodality applications for multiple myeloma. BMC Med Imaging. 2023;23:87 https://doi.org/10.1186/s12880-023-01033-2.
Haddaway NR, Page MJ, Pritchard CC, McGuinness LA. PRISMA2020: An R package and Shiny app for producing PRISMA 2020-compliant flow diagrams, with interactivity for optimised digital transparency and Open Synthesis Campbell Systematic Reviews. 2022;18, e1230. https://doi.org/10.1002/cl2.1230
Author information
Authors and Affiliations
Contributions
Conceptualization: INS, CF, MG; Data curation: INS, CF, PM; Formal analysis: CF; Investigation: INS, PM, VK, MT, EK, ET, MAD, MG; Methodology: INS, CF; Supervision: ET, MG; Roles/Writing - original draft: INS, CF; Writing - review & editing: PM, VK, MT, EK, MAD, ET, MG.
Corresponding author
Ethics declarations
Competing interests
INS declares honoraria from Janssen. PM declares honoraria from Janssen. EK declares honoraria from Amgen, Janssen, GSK, and Pfizer. MAD declares honoraria from Abbvie, Amgen, Bristol Myers Squibb, GSK, Janssen, Karyopharm, Pharmacyclics Inc, Pfizer, Sanofi, and Takeda. ET declares honoraria from Amgen, Astra/Zeneca, Bristol Myers Squibb, Eusa Pharma, GSK, Integris Pharma, Janssen, Pfizer, Sanofi, and Takeda. MG declares honoraria from GSK, Janssen, Sanofi, Abbvie, Amgen, and Takeda. The other authors declare no conflict of interest.
Ethics approval and consent to participate statement
This systematic review and meta-analysis was conducted in accordance with the PRISMA guidelines. As this study is based solely on previously published peer-reviewed data and does not involve human participants, interventions, or identifiable personal data, it did not require approval by an ethics committee or informed consent.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ntanasis-Stathopoulos, I., Filippatos, C., Malandrakis, P. et al. The impact of high-risk cytogenetics on treatment efficacy and outcomes of patients with relapsed/refractory multiple myeloma: a systematic review and meta-analysis of randomized controlled trials. Leukemia 39, 2226–2236 (2025). https://doi.org/10.1038/s41375-025-02677-5
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41375-025-02677-5