Abstract
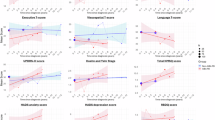
Cortical hypometabolism on FDG-PET is a well-established neuroimaging biomarker of cognitive impairment in Parkinson’s disease (PD), but its pathophysiologic origins are incompletely understood. Cholinergic basal forebrain (cBF) degeneration is a prominent pathological feature of PD-related cognitive impairment and may contribute to cortical hypometabolism through cholinergic denervation of cortical projection areas. Here, we investigated in-vivo associations between subregional cBF volumes on 3T-MRI, cortical hypometabolism on [18F]FDG-PET, and cognitive deficits in a cohort of 95 PD participants with varying degrees of cognitive impairment. We further assessed the spatial correspondence of the cortical pattern of cBF-associated hypometabolism with the pattern of cholinergic denervation in PD as assessed by [18F]FEOBV-PET imaging of presynaptic cholinergic terminal density in a second cohort. Lower volume of the cortically-projecting posterior cBF, but not of the anterior cBF, was significantly associated with extensive neocortical hypometabolism [p(FDR) < 0.05], which mediated the association between cBF atrophy and cognitive impairment (mediated proportion: 43%, p < 0.001). In combined models, posterior cBF atrophy explained more variance in cortical hypometabolism (R2 = 0.26, p < 0.001) than local atrophy in the cortical areas themselves (R2 = 0.16, p = 0.01). Topographic correspondence analysis with the [18F]FEOBV-PET pattern revealed that cortical areas showing most pronounced cBF-associated hypometabolism correspond to those showing most severe cholinergic denervation in PD (Spearman’s ρ = 0.57, p < 0.001). In conclusion, posterior cBF atrophy in PD is selectively associated with hypometabolism in denervated cortical target areas, which mediates the effect of cBF atrophy on cognitive impairment. These data provide first-time in-vivo evidence that cholinergic degeneration represents a principle pathological correlate of cortical hypometabolism underlying cognitive impairment in PD.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The data generated and analysed in the current study are available from the corresponding authors upon reasonable and formal request approved by the relevant local ethics committees.
References
Aarsland D, Batzu L, Halliday GM, Geurtsen GJ, Ballard C, Chaudhuri KR, et al. Parkinson disease-associated cognitive impairment. Nat Rev Dis Prim. 2021;7:47.
Garcia-Garcia D, Clavero P, Gasca Salas C, Lamet I, Arbizu J, Gonzalez-Redondo R, et al. Posterior parietooccipital hypometabolism may differentiate mild cognitive impairment from dementia in Parkinson’s disease. Eur J Nucl Med Mol Imaging. 2012;39:1767–77.
González-Redondo R, García-García D, Clavero P, Gasca-Salas C, García-Eulate R, Zubieta JL, et al. Grey matter hypometabolism and atrophy in Parkinson’s disease with cognitive impairment: a two-step process. Brain. 2014;137:2356–67.
Rodriguez-Oroz MC, Gago B, Clavero P, Delgado-Alvarado M, Garcia-Garcia D, Jimenez-Urbieta H. The relationship between atrophy and hypometabolism: is it regionally dependent in dementias? Curr Neurol Neurosci Rep. 2015;15:44.
Nestor PJ. The Lewy body, the hallucination, the atrophy and the physiology. Oxford University Press; 2007.
Borghammer P. Perfusion and metabolism imaging studies in Parkinson’s disease. Dan Med J. 2012;59:B4466.
Bohnen NI, Yarnall AJ, Weil RS, Moro E, Moehle MS, Borghammer P, et al. Cholinergic system changes in Parkinson’s disease: emerging therapeutic approaches. Lancet Neurol. 2022;21:381–92.
Ballinger EC, Ananth M, Talmage DA, Role LW. Basal forebrain cholinergic circuits and signaling in cognition and cognitive decline. Neuron. 2016;91:1199–218.
Ovsepian SV, O’Leary VB, Zaborszky L. Cholinergic mechanisms in the cerebral cortex: beyond synaptic transmission. Neuroscientist. 2015;22:238–51.
Browne SE, Lin L, Mattsson A, Georgievska B, Isacson O. Selective antibody-induced cholinergic cell and synapse loss produce sustained hippocampal and cortical hypometabolism with correlated cognitive deficits. Exp Neurol. 2001;170:36–47.
Gelfo F, Petrosini L, Alessandro PG, Bartolo D, Burello L, Vitale E, et al. Cortical metabolic deficits in a rat model of cholinergic basal forebrain degeneration. Neurochem Res. 2013;38:2114–23.
Grothe MJ, Labrador-Espinosa MA, Jesús S, Macías-García D, Adarmes-Gómez A, Carrillo F, et al. In vivo cholinergic basal forebrain degeneration and cognition in Parkinson’s disease: Imaging results from the COPPADIS study. Parkinsonism Relat Disord. 2021;88:68–75.
Barrett MJ, Sperling SA, Blair JC, Freeman CS, Flanigan JL, Smolkin ME, et al. Lower volume, more impairment: reduced cholinergic basal forebrain grey matter density is associated with impaired cognition in Parkinson disease. J Neurol Neurosurg Psychiatry. 2019;90:1251–6.
Ray NJ, Bradburn S, Murgatroyd C, Toseeb U, Mir P, Kountouriotis GK, et al. In vivo cholinergic basal forebrain atrophy predicts cognitive decline in de novo Parkinson’s disease. Brain. 2018;141:165–76.
Schulz J, Pagano G, Bonfante JAF, Wilson H, Politis M. Nucleus basalis of Meynert degeneration precedes and predicts cognitive impairment in Parkinson’s disease. Brain. 2018;141:1501–16.
Pereira JB, Hall S, Jalakas M, Grothe MJ, Strandberg O, Stomrud E, et al. Longitudinal degeneration of the basal forebrain predicts subsequent dementia in Parkinson’s disease. Neurobiol Dis. 2020;139:104831.
Labrador-Espinosa MA, Silva-Rodríguez J, Reina-Castillo MI, Mir P, Grothe MJ. Basal forebrain atrophy, cortical thinning, and amyloid-β status in Parkinson’s disease-related cognitive decline. Mov Disord. 2023;38:1871–80.
Postuma RB, Berg D, Stern M, Poewe W, Olanow CW, Oertel W, et al. MDS clinical diagnostic criteria for Parkinson’s disease. Mov Disord. 2015;30:1591–601.
Okkels N, Horsager J, Labrador-Espinosa M, Kjeldsen PL, Damholdt MF, Mortensen J, et al. Severe cholinergic terminal loss in newly diagnosed dementia with Lewy bodies. Brain. 2023;146:3690–704.
Skorvanek M, Goldman JG, Jahanshahi M, Marras C, Rektorova I, Schmand B, et al. Global scales for cognitive screening in Parkinson’s disease: critique and recommendations. Mov Disord. 2018;33:208–18.
Pagonabarraga J, Kulisevsky J, Llebaria G, García-Sánchez C, Pascual-Sedano B, Gironell A. Parkinson’s disease-cognitive rating scale: a new cognitive scale specific for Parkinson’s disease. Mov Disord. 2008;23:998–1005.
Hall S, Janelidze S, Londos E, Leuzy A, Stomrud E, Dage JL, et al. Plasma phospho-tau identifies Alzheimer’s co-pathology in patients with lewy body disease. Mov Disord. 2021;36:767–71.
Ashton NJ, Brum WS, Di Molfetta G, Benedet AL, Arslan B, Jonaitis E, et al. Diagnostic accuracy of a plasma phosphorylated tau 217 immunoassay for Alzheimer disease pathology. JAMA Neurol. 2024;81:255–63.
Periñán MT, Macías-García D, Labrador-Espinosa M, Jesús S, Buiza-Rueda D, Adarmes-Gómez AD, et al. Association of PICALM with cognitive impairment in Parkinson’s disease. Mov Disord. 2021;36:118–23.
Mizutani R, Saiga R, Takekoshi S, Inomoto C, Nakamura N, Itokawa M, et al. A method for estimating spatial resolution of real image in the Fourier domain. J Microsc. 2015;261:57–66.
Felix C, Alex Z, Barry B. A data-driven approach for estimating the spatial resolution of brain PET images (4301). Neurology. 2020;94:4301.
Ashburner J. A fast diffeomorphic image registration algorithm. NeuroImage. 2007;38:95–113.
Fritz H-CJ, Ray N, Dyrba M, Sorg C, Teipel S, Grothe MJ. The corticotopic organization of the human basal forebrain as revealed by regionally selective functional connectivity profiles. Hum Brain Mapp. 2019;40:868–78.
Grothe MJ, Heinsen H, Amaro E, Grinberg LT, Teipel SJ. Cognitive correlates of basal forebrain atrophy and associated cortical hypometabolism in mild cognitive impairment. Cerebral Cortex. 2016;26:2411–26.
Silva-Rodríguez J, Labrador-Espinosa MA, Moscoso A, Schöll M, Mir P, Grothe MJ. Characteristics of amnestic patients with hypometabolism patterns suggestive of Lewy body pathology. Brain. 2023;146:4520–31.
Gonzalez-Escamilla G, Lange C, Teipel S, Buchert R, Grothe MJ. PETPVE12: an SPM toolbox for partial volume effects correction in brain PET – application to amyloid imaging with AV45-PET. NeuroImage. 2017;147:669–77.
Okkels N, Horsager J, Labrador-Espinosa MA, Hansen FO, Andersen KB, Just K, et al. Distribution of cholinergic nerve terminals in the aged human brain measured with [18 F]FEOBV PET and its correlation with histological data. NeuroImage. 2023;269:119908.
Groemping U. Relative importance for linear regression in R: the package relaimpo. J Stat Softw. 2006;17:1–27.
Imai K, Keele L, Yamamoto T. Identification, inference and sensitivity analysis for causal mediation effects. Stat Sci. 2010;25:51–71.
Schaefer A, Kong R, Gordon EM, Laumann TO, Zuo X-N, Holmes AJ, et al. Local-global parcellation of the human cerebral cortex from intrinsic functional connectivity MRI. Cerebral Cortex. 2018;28:3095–114.
Bohnen NI, Koeppe RA, Minoshima S, Giordani B, Albin RL, Frey KA, et al. Cerebral glucose metabolic features of Parkinson disease and incident dementia: longitudinal study. J Nucl Med. 2011;52:848–55.
Mesulam MM. The cholinergic innervation of the human cerebral cortex. Prog Brain Res. 2004;145:67–78.
Jellinger K. Quantitative changes in some subcortical nuclei in aging, Alzheimer’s disease and Parkinson’s disease. Neurobiol Aging. 1987;8:556–61.
Liu AKL, Chang RC-C, Pearce RKB, Gentleman SM. Nucleus basalis of Meynert revisited: anatomy, history and differential involvement in Alzheimer’s and Parkinson’s disease. Acta Neuropathol. 2015;129:527–40.
Schumacher J, Kanel P, Dyrba M, Storch A, Teipel S, Grothe MJ. Structural and molecular cholinergic imaging markers of cognitive decline in Parkinson's disease. Brain. 2023;146:4964–73.
Ray NJ, Kanel P, Bohnen NI. Atrophy of the cholinergic basal forebrain can detect presynaptic cholinergic loss in Parkinson’s disease. Ann Neurol. 2023;93:991–8.
Crowley SJ, Kanel P, Roytman S, Bohnen NI, Hampstead BM. Basal forebrain integrity, cholinergic innervation and cognition in idiopathic Parkinson’s disease. Brain. 2024;147:1799–1808.
Khundakar AA, Hanson PS, Erskine D, Lax NZ, Roscamp J, Karyka E, et al. Analysis of primary visual cortex in dementia with Lewy bodies indicates GABAergic involvement associated with recurrent complex visual hallucinations. Acta Neuropathol Commun. 2016;4:66.
Patterson L, Firbank MJ, Colloby SJ, Attems J, Thomas AJ, Morris CM. Neuropathological changes in dementia with lewy bodies and the Cingulate Island sign. J Neuropathol Exp Neurol. 2019;78:717–24.
Higuchi M, Tashiro M, Arai H, Okamura N, Hara S, Higuchi S, et al. Glucose hypometabolism and neuropathological correlates in brains of dementia with Lewy bodies. Exp Neurol. 2000;162:247–56.
Andersen KB, Hansen AK, Schacht AC, Horsager J, Gottrup H, Klit H, et al. Synaptic density and glucose consumption in patients with Lewy Body Diseases: an [(11) C]UCB-J and [(18) F]FDG PET study. Mov Disord. 2023;38:796–805.
Albrecht F, Ballarini T, Neumann J, Schroeter ML. FDG-PET hypometabolism is more sensitive than MRI atrophy in Parkinson’s disease: a whole-brain multimodal imaging meta-analysis. NeuroImage Clin. 2019;21:101594.
Lanskey JH, McColgan P, Schrag AE, Acosta-Cabronero J, Rees G, Morris HR, et al. Can neuroimaging predict dementia in Parkinson’s disease? Brain. 2018;141:2545–60.
Svenningsson P, Westman E, Ballard C, Aarsland D. Cognitive impairment in patients with Parkinson’s disease: diagnosis, biomarkers, and treatment. Lancet Neurol. 2012;11:697–707.
Bohnen NI, Muller MLTM, Kotagal V, Koeppe RA, Kilbourn MA, Albin RL, et al. Olfactory dysfunction, central cholinergic integrity and cognitive impairment in Parkinson’s disease. Brain. 2010;133:1747–54.
Van Der Zee S, Müller MLTM, Kanel P, Van Laar T, Bohnen NI. Cholinergic denervation patterns across cognitive domains in Parkinson’s disease. Mov Disord. 2021;36:642–50.
Mori T, Ikeda M, Fukuhara R, Nestor PJ, Tanabe H. Correlation of visual hallucinations with occipital rCBF changes by donepezil in DLB. Neurology. 2006;66:935–7.
Suantio AM, Huang HL, Kwok CSN, Teo DCH, Nguyen MH. FDG-PET in suspected dementia with Lewy bodies: a case report. BMC Geriatr. 2019;19:150.
Satoh M, Ishikawa H, Meguro K, Kasuya M, Ishii H, Yamaguchi S. Improved visual hallucination by donepezil and occipital glucose metabolism in dementia with lewy bodies: the Osaki-Tajiri project. Eur Neurol. 2010;64:337–44.
Baik K, Kim SM, Jung JH, Lee YH, Chung SJ, Yoo HS, et al. Donepezil for mild cognitive impairment in Parkinson’s disease. Sci Rep. 2021;11:4734.
Bohnen NI, Müller MLTM, Kotagal V, Koeppe RA, Kilbourn MR, Gilman S, et al. Heterogeneity of cholinergic denervation in Parkinson’s disease without dementia. J Cereb Blood Flow Metab. 2012;32:1609–17.
Hirano S, Shinotoh H, Shimada H, Ota T, Sato K, Tanaka N, et al. Voxel-based acetylcholinesterase PET study in early and late onset Alzheimer’s disease. J Alzheimers Dis. 2018;62:1539–48.
Richter N, Nellessen N, Dronse J, Dillen K, Jacobs HIL, Langen KJ, et al. Spatial distributions of cholinergic impairment and neuronal hypometabolism differ in MCI due to AD. NeuroImage Clin. 2019;24:101978.
Grothe MJ, Teipel SJ. Spatial patterns of atrophy, hypometabolism, and amyloid deposition in Alzheimer’s disease correspond to dissociable functional brain networks. Hum Brain Mapp. 2016;37:35–53.
Mielke MM, Dage JL, Frank RD, Algeciras-Schimnich A, Knopman DS, Lowe VJ, et al. Performance of plasma phosphorylated tau 181 and 217 in the community. Nat Med. 2022;28:1398–405.
Gharbi-Meliani A, Dugravot A, Sabia S, Regy M, Fayosse A, Schnitzler A, et al. The association of APOE ε4 with cognitive function over the adult life course and incidence of dementia: 20years follow-up of the Whitehall II study. Alzheimers Res Ther. 2021;13:5.
Jansen WJ, Janssen O, Tijms BM, Vos SJB, Ossenkoppele R, Visser PJ, et al. Prevalence estimates of amyloid abnormality across the Alzheimer disease clinical spectrum. JAMA Neurol. 2022;79:228–43.
Coughlin DG, Hurtig HI, Irwin DJ. Pathological Influences on clinical heterogeneity in Lewy body diseases. Mov Disord. 2020;35:5–19.
Peter J, Mayer I, Kammer T, Minkova L, Lahr J, Klöppel S, et al. The relationship between cholinergic system brain structure and function in healthy adults and patients with mild cognitive impairment. Sci Rep. 2021;11:1–7.
Frey KA, Bohnen NILJ. Molecular imaging of neurodegenerative Parkinsonism. PET Clin. 2021;16:261–72.
Apostolova I, Lange C, Frings L, Klutmann S, Meyer PT, Buchert R. Nigrostriatal degeneration in the cognitive part of the striatum in Parkinson disease is associated with frontomedial hypometabolism. Clin Nuclear Med. 2020;45:95–99.
Orso B, Arnaldi D, Girtler N, Brugnolo A, Doglione E, Mattioli P, et al. Dopaminergic and serotonergic degeneration and cortical [18F]fluorodeoxyglucose positron emission tomography in De Novo Parkinson’s disease. Mov Disord. 2021;36:2293–302.
Acknowledgements
The authors would like to thank the participants in this study for their contribution to science and the Instituto de Biomedicina de Sevilla and the Hospital Universitario Virgen del Rocío for the research resources provided.
Funding
This work was supported by the Spanish Ministry of Science and Innovation (RTC2019-007150-1, PID2021-127034OA-I00), the Instituto de Salud Carlos III-Fondo Europeo de Desarrollo Regional (ISCIII-FEDER) (PI16/01575, PI18/01898, PI19/01576, PI20/00613, PI21/01875, PI22/01704), the Consejería de Economía, Innovación, Ciencia y Empleo de la Junta de Andalucía (CVI-02526, CTS-7685), the Consejería de Salud y Bienestar Social de la Junta de Andalucía (PI-0471-2013, PE-0210-2018, PI-0459-2018, PE-0186-2019), the Consejería de Transformación Económica, Industria, Conocimiento y Universidades de la Junta de Andalucía (PY20_00896, P20_00903), and the Fundación Alicia Koplowitz. Several authors of this publication are members of the European Reference Network for Rare Neurological Diseases (project ID 739510). M.A.L.E. is supported by a PhD scholarship (VI-PPIT-US) from the University of Seville (USE-19094-G). J.S.R. is supported by the “Sara Borrell” program (CD21/00067) of the ISCIII-FEDER. M.J.G. is supported by the “Miguel Servet” program (CP19/00031) of the ISCIII-FEDER. N.O. is supported by the Danish Parkinson’s Disease Association and the Health Research Foundation of Central Denmark Region. L.M.D. is supported by the “Río Hortega” program (CM21/00051) of the ISCIII-FEDER. D.M.G. is supported by the “Juan Rodés” program (JR22/00073) of the ISCIII-FEDER.
Author information
Authors and Affiliations
Contributions
MJG and PM contributed to the study conceptualization and design. NO, LMD, JH, AMCG, EIC, MSE, DMG, SJ, AAG, EOL, FC, FRL, DGS, and PB contributed to the data collection and material preparation. MALE, JSR, NO, SCL, PFR, and JFMR were involved in pre-processing and preparing the data for the analysis. The analyses were performed by MALE and JSR. The first draft of the manuscript was written by MALE and JSR. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of the University Hospital ‘Virgen del Rocío’ (approval number: 2158-N-20).
Consent for publication
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Labrador-Espinosa, M.A., Silva-Rodriguez, J., Okkels, N. et al. Cortical hypometabolism in Parkinson’s disease is linked to cholinergic basal forebrain atrophy. Mol Psychiatry 30, 2372–2380 (2025). https://doi.org/10.1038/s41380-024-02842-9
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41380-024-02842-9