Abstract
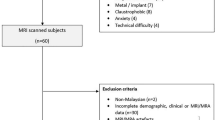
Little is known about how thalamic vascular patterns interact with small vessel diseases (SVDs) to influence affective symptoms. Here we collected 7-Telsa magnetic resonance imaging (MRI) data from 84 individuals with SVD and analyzed the influences of thalamic vascular pattern on affective symptoms, aiming to elucidate the underlying mechanisms driven by brain structure and function in the context of SVD. Subjects with a combined arterial supply by tuberothalamic and paramedian arteries to the right thalamus exhibited a lower Hamilton Anxiety scale (HAMA) score. When grouped by SVD burden, the same correlation remained in subjects with low SVD burden, whereas no difference was observed in the high SVD burden group. Interestingly, interaction effects of SVD and thalamic vascular pattern were also found affecting thalamic volume and resting-state brain activity in ventromedial prefrontal cortex (vmPFC). With moderated mediation analysis, right thalamic vascular pattern was indicated to affect anxiety through both direct (vascular pattern → HAMA score) and indirect (vascular pattern → thalamic volume → HAMA score) pathways. But high SVD burden interrupted the effects of right thalamic vascular pattern on HAMA score and thalamic volume. The finding that subjects with a combined arterial supply to the right thalamus exhibited a lower level of anxiety may suggest a novel vascular resilience for regulating anxiety. However, this vascular compensation mechanism was found to be impaired by elevated SVD burden and the disrupted inhibitory vmPFC activity caused by impaired thalamus. The findings of the present study provide a new underlying mechanism for affective disorders with SVD involved.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the cor- responding authors upon reasonable request.
References
Pessoa L. A network model of the emotional brain. Trends Cogn Sci. 2017;21:357–71.
Malezieux M, Klein AS, Gogolla N. Neural circuits for emotion. Annu Rev Neurosci. 2023;46:211–31.
Scharf AC, Gronewold J, Eilers A, Todica O, Moenninghoff C, Doeppner TR, et al. Depression and anxiety in acute ischemic stroke involving the anterior but not paramedian or inferolateral thalamus. Front Psychol. 2023;14:1218526.
Liebermann D, Ostendorf F, Kopp UA, Kraft A, Bohner G, Nabavi DG, et al. Subjective cognitive-affective status following thalamic stroke. J Neurol. 2013;260:386–96.
Li S, Kumar Y, Gupta N, Abdelbaki A, Sahwney H, Kumar A, et al. Clinical and neuroimaging findings in thalamic territory infarctions: a review. J Neuroimaging. 2018;28:343–9.
Schmahmann JD. Vascular syndromes of the thalamus. Stroke. 2003;34:2264–78.
Cooper CM, Chin Fatt CR, Liu P, Grannemann BD, Carmody T, Almeida JRC, et al. Discovery and replication of cerebral blood flow differences in major depressive disorder. Mol Psychiatry. 2020;25:1500–10.
Tang WK, Chen YK, Lu JY, Mok VC, Xiang YT, Ungvari GS, et al. Microbleeds and post-stroke emotional lability. J Neurol Neurosurg Psychiatry. 2009;80:1082–6.
Bordes S, Werner C, Mathkour M, McCormack E, Iwanaga J, Loukas M, et al. Arterial supply of the thalamus: a comprehensive review. World Neurosurg. 2020;137:310–8.
Lin E, Kamel H, Gupta A, RoyChoudhury A, Girgis P, Glodzik L. Incomplete circle of Willis variants and stroke outcome. Eur J Radiol. 2022;153:110383.
Clancy U, Gilmartin D, Jochems ACC, Knox L, Doubal FN, Wardlaw JM. Neuropsychiatric symptoms associated with cerebral small vessel disease: a systematic review and meta-analysis. Lancet Psychiatry. 2021;8:225–36.
Li X, Qin RR, Chen J, Jiang HF, Tang P, Wang YJ, et al. Neuropsychiatric symptoms and altered sleep quality in cerebral small vessel disease. Front Psychiatry. 2022;13:882922.
Clancy U, Ramirez J, Chappell FM, Doubal FN, Wardlaw JM, Black SE. Neuropsychiatric symptoms as a sign of small vessel disease progression in cognitive impairment. Cereb Circ Cogn Behav. 2022;3:100041.
Direk N, Perez HS, Akoudad S, Verhaaren BF, Niessen WJ, Hofman A, et al. Markers of cerebral small vessel disease and severity of depression in the general population. Psychiatry Res Neuroimaging. 2016;253:1–6.
Spalletta G, Iorio M, Vecchio D, Piras F, Ciullo V, Banaj N, et al. Subclinical cognitive and neuropsychiatric correlates and hippocampal volume features of brain white matter hyperintensity in healthy people. J Pers Med. 2020;10:172.
Hannawi Y, Vaidya D, Yanek LR, Johansen MC, Kral BG, Becker LC, et al. Association of vascular properties with the brain white matter hyperintensity in middle-aged population. J Am Heart Assoc. 2022;11:e024606.
Doubal FN, MacLullich AM, Ferguson KJ, Dennis MS, Wardlaw JM. Enlarged perivascular spaces on MRI are a feature of cerebral small vessel disease. Stroke. 2010;41:450–4.
Greenberg SM, Vernooij MW, Cordonnier C, Viswanathan A, Al-Shahi Salman R, Warach S, et al. Cerebral microbleeds: a guide to detection and interpretation. Lancet Neurol. 2009;8:165–74.
Vermeer SE, Longstreth WT Jr., Koudstaal PJ. Silent brain infarcts: a systematic review. Lancet Neurol. 2007;6:611–9.
Staals J, Makin SD, Doubal FN, Dennis MS, Wardlaw JM. Stroke subtype, vascular risk factors, and total MRI brain small-vessel disease burden. Neurology. 2014;83:1228–34.
Cao QL, Sun Y, Hu H, Wang ZT, Tan L, Yu JT, et al. Association of cerebral small vessel disease burden with neuropsychiatric symptoms in non-demented elderly: a longitudinal study. J Alzheimers Dis. 2022;89:583–92.
Wang Y, Yang Y, Wang T, Nie S, Yin H, Liu J. et al. Correlation between white matter hyperintensities related gray matter volume and cognition in cerebral small vessel disease. J Stroke Cerebrovasc Dis. 2020;29:105275.
Guo C, Wang B, Huo Y, Shan L, Qiao T, Yang Z, et al. The effects of P2 segment of posterior cerebral artery to thalamus blood supply pattern on gait in cerebral small vessel disease: A 7 T MRI based study. Neurobiol Dis. 2024;190:106372.
Kato H, Yoshikawa T, Oku N, Imaizumi M, Takasawa M, Kimura Y, et al. Statistical parametric analysis of cerebral blood flow in vascular dementia with small-vessel disease using Tc-HMPAO SPECT. Cerebrovasc Dis. 2008;26:556–62.
Ter Telgte A, van Leijsen EMC, Wiegertjes K, Klijn CJM, Tuladhar AM, de Leeuw FE. Cerebral small vessel disease: from a focal to a global perspective. Nat Rev Neurol. 2018;14:387–98.
Zhang X, Suo X, Yang X, Lai H, Pan N, He M, et al. Structural and functional deficits and couplings in the cortico-striato-thalamo-cerebellar circuitry in social anxiety disorder. Transl Psychiatry. 2022;12:26.
Zhang Y, Zhang Y, Ai H, Van Dam NT, Qian L, Hou G, et al. Microstructural deficits of the thalamus in major depressive disorder. Brain Commun. 2022;4:fcac236.
Xu J, Chen H, Hu Z, Ke Z, Qin R, Chen Y, et al. Characteristic patterns of functional connectivity-mediated cerebral small vessel disease-related cognitive impairment and depression. Cereb Cortex. 2024;34:bhad468.
Datta R, Bacchus MK, Kumar D, Elliott MA, Rao A, Dolui S, et al. Fast automatic segmentation of thalamic nuclei from MP2RAGE acquisition at 7 Tesla. Magn Reson Med. 2021;85:2781–90.
Jerman T, Pernus F, Likar B, Spiclin Z. Enhancement of vascular structures in 3D and 2D angiographic images. IEEE Trans Med Imaging. 2016;35:2107–18.
Chao-Gan Y, Yu-Feng Z. DPARSF: A MATLAB toolbox for “Pipeline” data analysis of resting-state fMRI. Front Syst Neurosci. 2010;4:13.
Hayes AF PROCESS: a versatile computational tool for mediation, moderation, and conditional process analysis. 2012.
Zhang X, Cheng B, Yang X, Suo X, Pan N, Chen T, et al. Emotional intelligence mediates the protective role of the orbitofrontal cortex spontaneous activity measured by fALFF against depressive and anxious symptoms in late adolescence. Eur Child Adolesc Psychiatry. 2023;32:1957–67.
Xue S, Kong F, Song Y, Liu J. Neural correlates of social interaction anxiety and their relation to emotional intelligence: a resting-state fMRI study. Neurosci Lett. 2024;818:137475.
Adrian-Ventura J, Fabregat-Nabas J, Costumero V, Avila C. Underlying differences in resting-state activity metrics related to sensitivity to punishment. Behav Brain Res. 2023;437:114152.
Etkin A, Wager TD. Functional neuroimaging of anxiety: a meta-analysis of emotional processing in PTSD, social anxiety disorder, and specific phobia. Am J Psychiatry. 2007;164:1476–88.
van Sloten TT, Sigurdsson S, van Buchem MA, Phillips CL, Jonsson PV, Ding J, et al. Cerebral small vessel disease and association with higher incidence of depressive symptoms in a general elderly population: The AGES-Reykjavik Study. Am J Psychiatry. 2015;172:570–8.
Fang Y, Qin T, Liu W, Ran L, Yang Y, Huang H, et al. Cerebral small-vessel disease and risk of incidence of depression: a meta-analysis of longitudinal cohort studies. J Am Heart Assoc. 2020;9:e016512.
Ozel F, Hilal S, de Feijter M, van der Velpen I, Direk N, Ikram MA, et al. Associations of neuroimaging markers with depressive symptoms over time in middle-aged and elderly persons. Psychol Med. 2023;53:4355–63.
Zhang Y, Zhu C, Chen H, Duan X, Lu F, Li M, et al. Frequency-dependent alterations in the amplitude of low-frequency fluctuations in social anxiety disorder. J Affect Disord. 2015;174:329–35.
Wang W, Hou J, Qian S, Liu K, Li B, Li M, et al. Aberrant regional neural fluctuations and functional connectivity in generalized anxiety disorder revealed by resting-state functional magnetic resonance imaging. Neurosci Lett. 2016;624:78–84.
Dymond S, Dunsmoor JE, Vervliet B, Roche B, Hermans D. Fear generalization in humans: systematic review and implications for anxiety disorder research. Behav Ther. 2015;46:561–82.
van Meurs B, Wiggert N, Wicker I, Lissek S. Maladaptive behavioral consequences of conditioned fear-generalization: a pronounced, yet sparsely studied, feature of anxiety pathology. Behav Res Ther. 2014;57:29–37.
Lissek S, Kaczkurkin AN, Rabin S, Geraci M, Pine DS, Grillon C. Generalized anxiety disorder is associated with overgeneralization of classically conditioned fear. Biol Psychiatry. 2014;75:909–15.
El-Bar N, Laufer O, Yoran-Hegesh R, Paz R. Over-generalization in youth with anxiety disorders. Soc Neurosci. 2017;12:76–85.
Dunsmoor JE, Paz R. Fear generalization and anxiety: behavioral and neural mechanisms. Biol Psychiatry. 2015;78:336–43.
Kenwood MM, Kalin NH, Barbas H. The prefrontal cortex, pathological anxiety, and anxiety disorders. Neuropsychopharmacology. 2022;47:260–75.
Li Y, Lopez-Huerta VG, Adiconis X, Levandowski K, Choi S, Simmons SK, et al. Distinct subnetworks of the thalamic reticular nucleus. Nature. 2020;583:819–24.
Li H, Jacob MA, Cai M, Duering M, Chamberland M, Norris DG, et al. Regional cortical thinning, demyelination and iron loss in cerebral small vessel disease. Brain. 2023;146:4659–73.
Liu R, Yue Y, Hou Z, Yuan Y, Wang Q. Risk factors associated with cognitions for late-onset depression based on anterior and posterior default mode sub-networks. J Affect Disord. 2018;235:544–50.
Wardlaw JM, Smith C, Dichgans M. Small vessel disease: mechanisms and clinical implications. Lancet Neurol. 2019;18:684–96.
Liu H, Hao Z, Qiu S, Wang Q, Zhan L, Huang L, et al. Grey matter structural alterations in anxiety disorders: a voxel-based meta-analysis. Brain Imaging Behav. 2024;18:456–74.
Moon CM, Kim GW, Jeong GW. Whole-brain gray matter volume abnormalities in patients with generalized anxiety disorder: voxel-based morphometry. Neuroreport. 2014;25:184–9.
Gainotti G. Emotions and the right hemisphere: can new data clarify old models? Neuroscientist. 2019;25:258–70.
Gunturkun O, Strockens F, Ocklenburg S. Brain lateralization: a comparative perspective. Physiol Rev. 2020;100:1019–63.
Sato W, Aoki S. Right hemispheric dominance in processing of unconscious negative emotion. Brain Cogn. 2006;62:261–6.
Acknowledgements
This work was supported by the National Natural Science Foundation of China (No. 82271956, No. 62331021), Shanghai Municipal Science and Technology Major Project (No. 2018SHZDZX01), Shanghai Municipal Science and Technology Explorer Project (No. 23TS1400500).
Author information
Authors and Affiliations
Contributions
BW and CG contributed to the study concept and design, analysis and interpretation of data, statistical analysis, and drafting/revising the manuscript for content. YC, YH, and BZ took part in the acquisition and interpretation of data. GL revised the manuscript. HW and YH participated in study concept and design, data acquisition and interpretation. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent
This study was approved by the Ethics Committee of Yueyang Hospital (Approval no. 2020-060), and all methods were performed in accordance with the relevant guidelines and regulations. Written informed consent was obtained from all participants.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, B., Guo, C., Chu, YH. et al. Differential impact of cerebral small vessel disease on thalamic regulation of anxiety: insights from 7T MRI. Mol Psychiatry 30, 4142–4150 (2025). https://doi.org/10.1038/s41380-025-02994-2
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41380-025-02994-2