Abstract
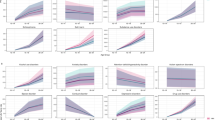
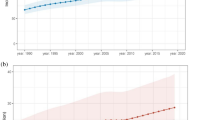
A comprehensive analysis of the global burden and trends of mental disorders (MDs) and substance use disorders (SUDs) among reproductive-age women is lacking. This study estimated the burden of disease attributable to MDs and SUDs in reproductive-age women from 1990 to 2021. Using data from the Global Burden of Disease Study 2021, we assessed the prevalence, incidence, and years lived with disability (YLDs) of 12 types of MDs and SUDs among reproductive-age women between 1990 and 2021. Estimates were stratified by age and sex at global, regional, and national levels. Trends were evaluated using the average annual percentage change (AAPC) and total percentage change. In 2021, the global age-standardized prevalence rates per 100,000 population among reproductive-age women were 17,573 (95% uncertainty interval 15,443–19,954) for MDs and 1806 (95% uncertainty interval 484–2191) for SUDs. Among MDs, depressive and anxiety disorders were the leading contributors to YLDs, with age-standardized YLD rates of 1,073.5 (686.73–1,562.48) and 844.05 (532.79–1,232.57) per 100,000 population, respectively. From 1990 to 2021, age-standardized rates of the prevalence, incidence, and YLDs of MDs increased (AAPC: 35%, 55%, and 38%, respectively), while those of SUDs decreased (AAPC: −55%, −62%, and −19%, respectively). The burden of both MDs and SUDs was highest in regions with higher sociodemographic indices. The greatest increases in burden were observed among younger women aged 15–24 years with MDs and 15–34 years with SUDs. MDs and SUDs are substantial contributors to the global disease burden in reproductive-age women. The magnitude and distribution of this burden vary by disorder type, country, age group, and sociodemographic development.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The datasets generated during and/or analysed during the current study are available in the Global Burden of Disease repository, https://vizhub.healthdata.org/gbd-results/.
References
Whiteford HA, Degenhardt L, Rehm J, Baxter AJ, Ferrari AJ, Erskine HE, et al. Global burden of disease attributable to mental and substance use disorders: findings from the Global Burden of Disease Study 2010. Lancet. 2013;382:1575–86.
GBD 2019 Mental Disorders Collaborators. Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Psychiatry. 2022;9:137–50.
GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1204–22.
GBD 2016 Alcohol and Drug Use Collaborators. The global burden of disease attributable to alcohol and drug use in 195 countries and territories, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Psychiatry. 2018;5:987–1012.
Kuehner C. Why is depression more common among women than among men? Lancet Psychiatry. 2017;4:146–58.
Annajigowda HH, Nirisha LP, Ganjekar S, Rao GN, Gururaj G, Varghese M, et al. Common mental disorders among women in reproductive age group: An analysis of national mental health survey, India 2016. Indian J Psychiatry. 2023;65:1238–43.
Kessler RC. Epidemiology of women and depression. J Affect Disord. 2003;74:5–13.
Martin CE, Scialli A, Terplan M. Addiction and depression: unmet treatment needs among reproductive age women. Matern Child Health J. 2020;24:660–7.
McHugh RK, Wigderson S, Greenfield SF. Epidemiology of substance use in reproductive-age women. Obstet Gynecol Clin North Am. 2014;41:177–89.
Kieling C, Buchweitz C, Caye A, Silvani J, Ameis SH, Brunoni AR, et al. Worldwide prevalence and disability from mental disorders across childhood and adolescence: evidence from the global burden of disease study. JAMA Psychiatry. 2024;81:347–56.
Castelpietra G, Knudsen AKS, Agardh EE, Armocida B, Beghi M, Iburg KM, et al. The burden of mental disorders, substance use disorders and self-harm among young people in Europe, 1990-2019: Findings from the Global Burden of Disease Study 2019. Lancet Reg Health Eur. 2022;16:100341.
Albright BB, Rayburn WF. Substance abuse among reproductive age women. Obstet Gynecol Clin North Am. 2009;36:891–906.
GBD 2021 Risk Factors Collaborators. Global burden and strength of evidence for 88 risk factors in 204 countries and 811 subnational locations, 1990-2021: a systematic analysis for the Global Burden of Disease Study 2021. Lancet. 2024;403:2162–203.
GBD 2021 Diseases and Injuries Collaborators. Global incidence, prevalence, years lived with disability (YLDs), disability-adjusted life-years (DALYs), and healthy life expectancy (HALE) for 371 diseases and injuries in 204 countries and territories and 811 subnational locations, 1990-2021: a systematic analysis for the Global Burden of Disease Study 2021. Lancet. 2024;403:2133–61.
Bennett AC, Gibson C, Rohan AM, Howland JF, Rankin KM. Mental health and substance use-related hospitalizations among women of reproductive age in illinois and wisconsin. Public Health Rep. 2019;134:17–26.
Friedman SH, Loue S. Incidence and prevalence of intimate partner violence by and against women with severe mental illness. J Womens Health (Larchmt). 2007;16:471–80.
Miller E, Lasser KE, Becker AE. Breast and cervical cancer screening for women with mental illness: patient and provider perspectives on improving linkages between primary care and mental health. Arch Womens Ment Health. 2007;10:189–97.
Prince M, Patel V, Saxena S, Maj M, Maselko J, Phillips MR, et al. No health without mental health. Lancet. 2007;370:859–77.
Thornicroft G. Physical health disparities and mental illness: the scandal of premature mortality. Br J Psychiatry. 2011;199:441–2.
Cabaj JL, McDonald SW, Tough SC. Early childhood risk and resilience factors for behavioural and emotional problems in middle childhood. BMC Pediatr. 2014;14:166.
Guttmann A, Dick P, To T. Infant hospitalization and maternal depression, poverty and single parenthood - a population-based study. Child Care Health Dev. 2004;30:67–75.
Klinnert MD, Nelson HS, Price MR, Adinoff AD, Leung DY, Mrazek DA. Onset and persistence of childhood asthma: predictors from infancy. Pediatrics. 2001;108:E69.
To T, Guttmann A, Dick PT, Rosenfield JD, Parkin PC, Tassoudji M, et al. Risk markers for poor developmental attainment in young children: results from a longitudinal national survey. Arch Pediatr Adolesc Med. 2004;158:643–9.
Witt WP, Wisk LE, Cheng ER, Hampton JM, Hagen EW. Preconception mental health predicts pregnancy complications and adverse birth outcomes: a national population-based study. Matern Child Health J. 2012;16:1525–41.
Kessler RC, Birnbaum H, Bromet E, Hwang I, Sampson N, Shahly V. Age differences in major depression: results from the National Comorbidity Survey Replication (NCS-R). Psychol Med. 2010;40:225–37.
Monroe SM, Slavich GM, Gotlib IH. Life stress and family history for depression: the moderating role of past depressive episodes. J Psychiatr Res. 2014;49:90–5.
Slavich GM, Sacher J. Stress, sex hormones, inflammation, and major depressive disorder: Extending Social Signal Transduction Theory of Depression to account for sex differences in mood disorders. Psychopharmacology (Berl). 2019;236:3063–79.
Yonkers KA, Vigod S, Ross LE. Diagnosis, pathophysiology, and management of mood disorders in pregnant and postpartum women. Obstet Gynecol. 2011;117:961–77.
Borri C, Mauri M, Oppo A, Banti S, Rambelli C, Ramacciotti D, et al. Axis I psychopathology and functional impairment at the third month of pregnancy: Results from the Perinatal Depression-Research and Screening Unit (PND-ReScU) study. J Clin Psychiatry. 2008;69:1617–24.
Felice E, Saliba J, Grech V, Cox J, Calleja N. Antenatal psychiatric morbidity in Maltese women. Gen Hosp Psychiatry. 2007;29:501–5.
Uguz F, Ak M. Cognitive-behavioral therapy in pregnant women with generalized anxiety disorder: a retrospective cohort study on therapeutic efficacy, gestational age and birth weight. Braz J Psychiatry. 2020;43:61–4.
Uguz F, Yakut E, Aydogan S, Bayman MG, Gezginc K. Prevalence of mood and anxiety disorders during pregnancy: a case-control study with a large sample size. Psychiatry Res. 2019;272:316–8.
Patel V, Rodrigues M, DeSouza N. Gender, poverty, and postnatal depression: a study of mothers in Goa, India. Am J Psychiatry. 2002;159:43–7.
Leahy-Warren P, McCarthy G, Corcoran P. First-time mothers: social support, maternal parental self-efficacy and postnatal depression. J Clin Nurs. 2012;21:388–97.
World Health Organization (WHO). Maternal mental health and child health and development in low and middle-income countries. Report of the meeting, Geneva, Switzerland, 30 January - 1 February, 2008.
O’Mahen HA, Woodford J, McGinley J, Warren FC, Richards DA, Lynch TR, et al. Internet-based behavioral activation–treatment for postnatal depression (Netmums): a randomized controlled trial. J Affect Disord. 2013;150:814–22.
Addati L, Cattaneo U, Esquivel V, Valarino I, International Labour Organization. Gender, E. and D. B., International Labour Organization. Conditions of Work and Equality Department., & ILO Programme on HIV/AIDS and the World of Work. Care work and care jobs for the future of decent work. ILO; 2018.
Rosenfield, S, & Smith, D (2010). Gender and mental health: Do men and women have different amounts or types of problems? In TL Scheid & TN Brown (Eds.), A handbook for the study of mental health: Social contexts, theories, and systems (2nd ed., pp. 256-67). Cambridge University Press.
Twenge JM, Haidt J, Lozano J, Cummins KM. Specification curve analysis shows that social media use is linked to poor mental health, especially among girls. Acta Psychol (Amst). 2022;224:103512.
Saunders JF, Eaton AA. Social comparisons in eating disorder recovery: Using PhotoVoice to capture the sociocultural influences on women’s recovery. Int J Eat Disord. 2018;51:1361–6.
World Health Organization. (22 June 2021-Last update:20 April 2023). Making every school a health-promoting school-Global standards and indicators. the United Nations Educational, Scientific and Cultural Organization. https://www.unesco.org/en/articles/unesco-and-who-urge-countries-make-every-school-health-promoting-school.
Fardouly J, Diedrichs PC, Vartanian LR, Halliwell E. Social comparisons on social media: the impact of Facebook on young women’s body image concerns and mood. Body Image. 2015;13:38–45.
Grabe S, Ward LM, Hyde JS. The role of the media in body image concerns among women: a meta-analysis of experimental and correlational studies. Psychol Bull. 2008;134:460–76.
van Eeden AE, van Hoeken D, Hoek HW. Incidence, prevalence and mortality of anorexia nervosa and bulimia nervosa. Curr Opin Psychiatry. 2021;34:515–24.
Fredrickson BL, Roberts TA. Objectification theory: Toward understanding women’s lived experiences and mental health risks. Psychology of Women Quarterly. 1997;21:173–206.
Keel PK, Klump KL. Are eating disorders culture-bound syndromes? Implications for conceptualizing their etiology. Psychol Bull. 2003;129:747–69.
Thapar A, Cooper M. Attention deficit hyperactivity disorder. Lancet. 2016;387:1240–50.
Polanczyk G, de Lima MS, Horta BL, Biederman J, Rohde LA. The worldwide prevalence of ADHD: a systematic review and metaregression analysis. Am J Psychiatry. 2007;164:942–8.
Hinshaw SP, Nguyen PT, O’Grady SM, Rosenthal EA. Annual Research Review: Attention-deficit/hyperactivity disorder in girls and women: underrepresentation, longitudinal processes, and key directions. J Child Psychol Psychiatry. 2022;63:484–96.
Young S, Adamo N, Asgeirsdottir BB, Branney P, Beckett M, Colley W, et al. Females with ADHD: an expert consensus statement taking a lifespan approach providing guidance for the identification and treatment of attention-deficit/ hyperactivity disorder in girls and women. BMC Psychiatry. 2020;20:404.
Faraone SV, Biederman J, Mick E. The age-dependent decline of attention deficit hyperactivity disorder: a meta-analysis of follow-up studies. Psychol Med. 2006;36:159–65.
Zhang S, Qi X, Wang Y, Fang K. Global burden of drug use disorders by region and country, 1990–2021. Front Public Health. 2024;12:1470809.
World Health Organization (2018). Adolescent alcohol-related behaviours: trends and inequalities in the WHO European Region, 2002-2014: observations from the Health Behaviour in School-aged Children (HBSC) WHO collaborative cross-national study.
OECD/European Union (2020), Health at a Glance: Europe 2020: State of Health in the EU Cycle, OECD Publishing, Paris, https://doi.org/10.1787/82129230-en.
Coleman-Cowger VH, Oga EA, Peters EN, Trocin KE, Koszowski B, Mark K. Accuracy of three screening tools for prenatal substance use. Obstet Gynecol. 2019;133:952–61.
Le TL, Kenaszchuk C, Milligan K, Urbanoski K. Levels and predictors of participation in integrated treatment programs for pregnant and parenting women with problematic substance use. BMC Public Health. 2019;19:154.
Maternal and Child Health Bureau HRaSA. (December 2024). Title V maternal and child health services block grant program. Health Resources and Services Administration. https://mchb.hrsa.gov/programs-impact/title-v-maternal-child-health-mch-services-block-grant.
Maternal and Child Health Bureau Priorities and Opportunities for Partnership. National Conference of State Legislatures: MCH Fellow Kick Off Meeting. January 7, 2023.
Nutt D, King LA, Saulsbury W, Blakemore C. Development of a rational scale to assess the harm of drugs of potential misuse. Lancet. 2007;369:1047–53.
Zhang T, Yin X, Chen H, Li Y, Chen J, Yang X. Global magnitude and temporal trends of idiopathic developmental intellectual disability attributable to lead exposure from 1990 to 2019: Results from Global Burden of Disease Study. Sci Total Environ. 2022;834:155366.
Ferrari AJ, Charlson FJ, Norman RE, Patten SB, Freedman G, Murray CJ, et al. Burden of depressive disorders by country, sex, age, and year: findings from the global burden of disease study 2010. PLoS Med. 2013;10:e1001547.
GBD 2015 Eastern Mediterranean Region Mental Health Collaborators. The burden of mental disorders in the Eastern Mediterranean region, 1990-2015: findings from the global burden of disease 2015 study. Int J Public Health. 2018;63:25–37.
India State-Level Disease Burden Initiative Mental Disorders Collaborators. The burden of mental disorders across the states of India: the Global Burden of Disease Study 1990-2017. Lancet Psychiatry. 2020;7:148–61.
Lee SC, DelPozo-Banos M, Lloyd K, Jones I, Walters JTR, Owen MJ, et al. Area deprivation, urbanicity, severe mental illness and social drift - A population-based linkage study using routinely collected primary and secondary care data. Schizophr Res. 2020;220:130–40.
World Health Organization. (2021). Mental Health Atlas. Geneva: WHO; 2020.
World Health Organization. Depression and Other Common Mental Disorders: Global Health Estimates. Geneva: WHO; 2017.
Qu X, Liu M, Ke C, Liang J, Du Y, Yao L, et al. Burden of alcohol use disorders in China and the regions with different income levels over the world. J Glob Health. 2021;11:08011.
Danpanichkul P, Ng CH, Muthiah M, Suparan K, Tan DJH, Duangsonk K, et al. From shadows to spotlight: exploring the escalating burden of alcohol-associated liver disease and alcohol use disorder in young women. Am J Gastroenterol. 2024;119:893–909.
Castaldelli-Maia JM, Bhugra D. Analysis of global prevalence of mental and substance use disorders within countries: focus on sociodemographic characteristics and income levels. Int Rev Psychiatry. 2022;34:6–15.
Javed A, Lee C, Zakaria H, Buenaventura RD, Cetkovich-Bakmas M, Duailibi K, et al. Reducing the stigma of mental health disorders with a focus on low- and middle-income countries. Asian J Psychiatr. 2021;58:102601.
Weinmann S, Koesters M. Mental health service provision in low and middle-income countries: recent developments. Curr Opin Psychiatry. 2016;29:270–5.
Peacock A, Leung J, Larney S, Colledge S, Hickman M, Rehm J, et al. Global statistics on alcohol, tobacco and illicit drug use: 2017 status report. Addiction. 2018;113:1905–26.
Suarez EA, Bateman BT, Hernandez-Diaz S, Straub L, McDougle CJ, Wisner KL, et al. Prescription stimulant use during pregnancy and risk of neurodevelopmental disorders in children. JAMA Psychiatry. 2024;81:477–88.
World Development Report 2022: finance for an equitable recovery xx, 257 p. : COVID-19 Debt management risk management financial inclusion 2022.
Chen J, Jordan LP. Intergenerational support in one- and multi-child families in china: does child gender still matter? Res Aging. 2018;40:180–204.
Meng S, Pan F, Wu F. Intergenerational financial support for homeownership and co-residence in Chinese cities. Cities. 2023;137:104310.
Chowdhury IS, Li Y, Ge J, Wang D, Mileva EA, Lugo MA, et al. China Economic Update : Navigating Uncertainty - China’s Economy in 2023 (English). Washington, D.C.: World Bank Group. http://documents.worldbank.org/curated/en/099062002232318248.
Chen H, Phillips M, Cheng H, Chen Q, Chen X, Fralick D, et al. Mental Health Law of the People’s Republic of China (English translation with annotations): Translated and annotated version of China’s new Mental Health Law. Shanghai Arch Psychiatry. 2012;24:305–21.
Yang LH, Kleinman A, Link BG, Phelan JC, Lee S, Good B. Culture and stigma: adding moral experience to stigma theory. Soc Sci Med. 2007;64:1524–35.
Li J, Zhang MM, Zhao LJ, Li WQ, Mu JL, Zhang ZH. Stigma and discrimination experienced by people with mental illness in China: A critical review and meta-synthesis of qualitative studies. Social Science & Medicine. 2018;212:7.
United Nations Office on Drugs and Crime. 2022. World drug report 2022. United Nations. https://www.unodc.org/unodc/data-and-analysis/world-drug-report-2022.html.
Centers for Disease Control and Prevention. (2021). Overdose Prevention: Understanding the Opioid Overdose Epidemic. https://www.cdc.gov/overdose-prevention/about/understanding-the-opioid-overdose-epidemic.html.
Marel C, Mills KL, Teesson M. Substance use, mental disorders and COVID-19: a volatile mix. Curr Opin Psychiatry. 2021;34:351–6.
Mendez R, Balanza-Martinez V, Luperdi SC, Estrada I, Latorre A, Gonzalez-Jimenez P, et al. Short-term neuropsychiatric outcomes and quality of life in COVID-19 survivors. J Intern Med. 2021;290:621–31.
Taquet M, Luciano S, Geddes JR, Harrison PJ. Bidirectional associations between COVID-19 and psychiatric disorder: retrospective cohort studies of 62 354 COVID-19 cases in the USA. Lancet Psychiatry. 2021;8:130–40.
Metin A, Erbicer ES, Sen S, Cetinkaya A. Gender and COVID-19 related fear and anxiety: a meta-analysis. J Affect Disord. 2022;310:384–95.
COVID-19 Mental Disorders Collaborators. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet. 2021;398:1700–12.
Acknowledgements
We thank BioMed Proofreading LLC for providing English-language editing support. We also would like to thank Professor Chingyu Cheng from the Yong Loo Lin School of Medicine, National University of Singapore, for his valuable guidance in data analysis and critical insights during this study.
Funding
The present project was supported by grants from GDPH Supporting Fund for Talent Program (KY0120220263), the National Natural Science Foundation of China (82271125, 81870663, 82171075, and 82301205), 2024 National Foreign Expert Project (S20240245), Guangdong Basic and Applied Basic Research Foundation (2023B1515120028), the launch fund of Guangdong Provincial People’s Hospital for NSFC (8217040449, 8227040339 and 8217040546), the Science and Technology Program of Guangzhou (20220610092), the Outstanding Young Talent Trainee Program of Guangdong Provincial People’s Hospital (KJ012019087), the GDPH Scientific Research Funds for Leading Medical Talents and Distinguished Young Scholars in Guangdong Province (KJ012019457), and Personalized Medical Incubator Project, The fund for Precision Medicine Research and Industry Development in SIMQ (2023-31). The funder had no role in the design, data collection, data analysis, and reporting of this study.
Author information
Authors and Affiliations
Contributions
CL and AYL are joint first authors. LL, YJH and HHY conceived the design of this paper. CL, SML and LL did analyses of the Global Burden of Disease data. AYL, CL and LL wrote the first draft and contributed to revisions of the draft. AYL, XHY, YK, YJH and HHY commented and edited all versions of the draft. All authors read and approved the final draft. All authors have full access to all the data in the study and accept responsibility to submit for publication.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Li, C., Liang, A., Kuang, Y. et al. Global burden of diseases attributed to mental and substance use disorders in reproductive-age women: an ecological analysis for the Global Burden of Disease Study 2021. Mol Psychiatry 31, 62–74 (2026). https://doi.org/10.1038/s41380-025-03216-5
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41380-025-03216-5