Abstract
Objective
To conduct a network meta-analysis to compare the efficacy and safety of various surgical strategies for refractory obsessive-compulsive disorder (OCD), including ablative surgery (ABL) and deep brain stimulation (DBS), with the aim to guide clinical treatment.
Methods
We searched major electronic databases for different surgical interventions of OCD. The primary outcomes were changes in the Yale-Brown Obsessive Compulsive Scale (Y-BOCS) at 1 year and at the longest follow-up (LFU); the secondary outcomes included responder rates of Y-BOCS (≥35% reduction) and changes in global function, depression, and anxiety; and the safety outcomes included surgery-related adverse events (SRAEs) and serious adverse events (SAEs).
Results
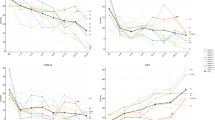
A total of 75 studies involving 1259 patients and 20 surgical strategies were enrolled. Most interventions resulted in significant improvements in Y-BOCS scores, with a reduction of around 10–15 points. Among them, radiofrequency capsulotomy (RF-Cap, mean difference [MD]: 17.251 at 1 year; MD: 17.458 at LFU) and inferior thalamic peduncle DBS (ITP-DBS, MD: 18.126 at 1 year; MD: 20.209 at LFU) were associated with the greatest improvements. Subthalamic nucleus + ventral capsule/ventral striatum DBS (STN + VC/VS-DBS) also exhibited good efficacy at the LFU (MD: 20.780), although data were lacking at 1 year. In terms of safety, ABL was associated with a higher rate of SRAEs than DBS (26 VS. 22%, p = 0.0325), with mechanical-Cap exhibiting the highest SRAE rate (47.5%). However, both DBS and ABL showed good acceptability, with no significant difference in SAEs.
Conclusion
Based on the current analysis, RF-Cap and ITP-DBS were associated with the largest improvements; however, the evidence for ITP-DBS is based on a small sample size, and should therefore be interpreted with caution. More head-to-head studies are needed to directly compare different surgical techniques and identify individual treatment options.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
Data availability
The dataset and code used for the present work will be available from the authors upon reasonable request.
References
Kumar KK, Appelboom G, Lamsam L, Caplan AL, Williams NR, Bhati MT, et al. Comparative effectiveness of neuroablation and deep brain stimulation for treatment-resistant obsessive-compulsive disorder: a meta-analytic study. J Neurol Neurosurg Psychiatry. 2019;90:469–73. https://doi.org/10.1136/jnnp-2018-319318.
Raviv N, Staudt MD, Rock AK, MacDonell J, Slyer J, Pilitsis JG. A systematic review of deep brain stimulation targets for obsessive compulsive disorder. Neurosurgery. 2020;87:1098–110. https://doi.org/10.1093/neuros/nyaa249.
Stein DJ, Costa DLC, Lochner C, Miguel EC, Reddy YCJ, Shavitt RG, et al. Obsessive-compulsive disorder. Nat Rev Dis Primers. 2019;5:52. https://doi.org/10.1038/s41572-019-0102-3.
Bergfeld IO, Dijkstra E, Graat I, de Koning P, van den Boom BJG, Arbab T, et al. Invasive and non-invasive neurostimulation for OCD. Curr Top Behav Neurosci. 2021;49:399–436. https://doi.org/10.1007/7854_2020_206.
Farrand S, Evans AH, Mangelsdorf S, Loi SM, Mocellin R, Borham A, et al. Deep brain stimulation for severe treatment-resistant obsessive-compulsive disorder: an open-label case series. Aust N Z J Psychiatry. 2018;52:699–708. https://doi.org/10.1177/0004867417731819.
Robbins TW, Vaghi MM, Banca P. Obsessive-Compulsive disorder: puzzles and prospects. Neuron. 2019;102:27–47. https://doi.org/10.1016/j.neuron.2019.01.046.
Tastevin M, Spatola G, Régis J, Lançon C, Richieri R. Deep brain stimulation in the treatment of obsessive-compulsive disorder: current perspectives. Neuropsychiatr Dis Treat. 2019;15:1259–72. https://doi.org/10.2147/NDT.S178207.
Dyster TG, Mikell CB, Sheth SA. The Co-evolution of neuroimaging and psychiatric neurosurgery. Front Neuroanat. 2016;10:68. https://doi.org/10.3389/fnana.2016.00068.
Balachander S, Arumugham SS, Srinivas D. Ablative neurosurgery and deep brain stimulation for obsessive-compulsive disorder. Indian J Psychiatry. 2019;61:S77–84. https://doi.org/10.4103/psychiatry.IndianJPsychiatry_523_18.
Peker S, Samanci MY, Yilmaz M, Sengoz M, Ulku N, Ogel K. Efficacy and safety of gamma ventral capsulotomy for treatment-resistant obsessive-compulsive disorder: a single-center experience. World Neurosurg. 2020;141:e941–52. https://doi.org/10.1016/j.wneu.2020.06.098.
Davidson B, Hamani C, Rabin JS, Goubran M, Meng Y, Huang Y, et al. Magnetic resonance-guided focused ultrasound capsulotomy for refractory obsessive compulsive disorder and major depressive disorder: clinical and imaging results from two phase I trials. Mol Psychiatry. 2020;25:1946–57. https://doi.org/10.1038/s41380-020-0737-1.
Li N, Baldermann JC, Kibleur A, Treu S, Akram H, Elias GJB, et al. A unified connectomic target for deep brain stimulation in obsessive-compulsive disorder. Nat Commun. 2020;11:3364. https://doi.org/10.1038/s41467-020-16734-3.
Hageman SB, van Rooijen G, Bergfeld IO, Schirmbeck F, de Koning P, Schuurman PR, et al. Deep brain stimulation versus ablative surgery for treatment-refractory obsessive-compulsive disorder: a meta-analysis. Acta Psychiatr Scand. 2021;143:307–18. https://doi.org/10.1111/acps.13276.
Naci H, Salcher-Konrad M, Kesselheim AS, Wieseler B, Rochaix L, Redberg RF, et al. Generating comparative evidence on new drugs and devices before approval. Lancet. 2020;395:986–97. https://doi.org/10.1016/S0140-6736(19)33178-2.
Nikolakopoulou A, Mavridis D, Furukawa TA, Cipriani A, Tricco AC, Straus SE, et al. Living network meta-analysis compared with pairwise meta-analysis in comparative effectiveness research: empirical study. BMJ. 2018;360:k585. https://doi.org/10.1136/bmj.k585.
Higgins JPT, Welton NJ. Network meta-analysis: a norm for comparative effectiveness? Lancet. 2015;386:628–30. https://doi.org/10.1016/S0140-6736(15)61478-7.
Cruz S, Gutiérrez-Rojas L, González-Domenech P, Díaz-Atienza F, Martínez-Ortega JM, Jiménez-Fernández S. Deep brain stimulation in obsessive-compulsive disorder: Results from meta-analysis. Psychiatry Res. 2022;317:114869. https://doi.org/10.1016/j.psychres.2022.114869.
Nikolakopoulou A, Higgins JPT, Papakonstantinou T, Chaimani A, Del Giovane C, Egger M, et al. CINeMA: an approach for assessing confidence in the results of a network meta-analysis. PLoS Med. 2020;17:e1003082. https://doi.org/10.1371/journal.pmed.1003082.
Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336:924–6. https://doi.org/10.1136/bmj.39489.470347.AD.
Brignardello-Petersen R, Florez ID, Izcovich A, Santesso N, Hazlewood G, Alhazanni W, et al. GRADE approach to drawing conclusions from a network meta-analysis using a minimally contextualised framework. BMJ. 2020;371:m3900. https://doi.org/10.1136/bmj.m3900.
Jayaram M, Wood SM, Kane RL, Yang L-Y, Chung KC. Association of open reduction and internal fixation with volar locking plate for distal radius fractures with patient-reported outcomes in older adults: a network meta-analysis. JAMA Netw Open. 2023;6:e2318715. https://doi.org/10.1001/jamanetworkopen.2023.18715.
Papola D, Miguel C, Mazzaglia M, Franco P, Tedeschi F, Romero SA, et al. Psychotherapies for generalized anxiety disorder in adults: a systematic review and network meta-analysis of randomized clinical trials. JAMA Psychiatry. 2024;81:250–9. https://doi.org/10.1001/jamapsychiatry.2023.3971.
Rasmussen SA, Noren G, Greenberg BD, Marsland R, McLaughlin NC, Malloy PJ, et al. Gamma ventral capsulotomy in intractable obsessive-compulsive disorder. Biol Psychiatry. 2018;84:355–64. https://doi.org/10.1016/j.biopsych.2017.11.034.
Rück C, Karlsson A, Steele JD, Edman G, Meyerson BA, Ericson K, et al. Capsulotomy for obsessive-compulsive disorder: long-term follow-up of 25 patients. Arch Gen Psychiatry. 2008;65:914. https://doi.org/10.1001/archpsyc.65.8.914.
McLaughlin NCR, Lauro PM, Patrick MT, Pucci FG, Barrios-Anderson A, Greenberg BD, et al. Magnetic resonance imaging-guided laser thermal ventral capsulotomy for intractable obsessive-compulsive disorder. Neurosurgery. 2021;88:1128–35. https://doi.org/10.1093/neuros/nyab050.
Zhang C, Kim S-G, Li J, Zhang Y, Lv Q, Zeljic K, et al. Anterior limb of the internal capsule tractography: relationship with capsulotomy outcomes in obsessive-compulsive disorder. J Neurol Neurosurg Psychiatry. 2021;92:637–44. https://doi.org/10.1136/jnnp-2020-323062.
Satzer D, Mahavadi A, Lacy M, Grant JE, Warnke P. Interstitial laser anterior capsulotomy for obsessive–compulsive disorder: lesion size and tractography correlate with outcome. J Neurol Neurosurg Psychiatry. 2022;93:317–23. https://doi.org/10.1136/jnnp-2021-327730.
Santos BFDO, Gorgulho A, Saraiva CWC, Lopes AC, Gomes JGR, Pássaro AM, et al. Understanding gamma ventral capsulotomy: potential implications of diffusion tensor image tractography on target selectivity. Surgical Neurol Int. 2019;10:136 https://doi.org/10.25259/SNI-65-2019.
Liu K, Zhang H, Liu C, Guan Y, Lang L, Cheng Y, et al. Stereotactic treatment of refractory obsessive compulsive disorder by bilateral capsulotomy with 3 years follow-up. J Clin Neurosci. 2008;15:622–9. https://doi.org/10.1016/j.jocn.2007.07.086.
Gong F, Li P, Li B, Zhang S, Zhang X, Yang S, et al. A study of cognitive function in treatment-refractory obsessive-compulsive disorder treated with capsulotomy. J Neurosurg. 2018;128:583–95. https://doi.org/10.3171/2016.9.JNS152494.
Zhan S, Liu W, Li D, Pan S, Pan Y, Li Y, et al. Long-term follow-up of bilateral anterior capsulotomy in patients with refractory obsessive-compulsive disorder. Clin Neurol Neurosurg. 2014;119:91–5. https://doi.org/10.1016/j.clineuro.2014.01.009.
Gong F, Li B, Zhang S, Wang Y, Gao Y, Xu Y, et al. The suitability of different subtypes and dimensions of obsessive-compulsive disorder for treatment with anterior capsulotomy: a long-term follow-up study. Stereotact Funct Neurosurg. 2019;97:319–36. https://doi.org/10.1159/000500137.
Lai Y, Wang T, Zhang C, Lin G, Voon V, Chang J, et al. Effectiveness and safety of neuroablation for severe and treatment-resistant obsessive–compulsive disorder: a systematic review and meta-analysis. jpn. 2020;45:356–69. https://doi.org/10.1503/jpn.190079.
Schlaepfer TE, Bewernick BH, Kayser S, Hurlemann R, Coenen VA. Deep brain stimulation of the human reward system for major depression-rationale, outcomes and outlook. Neuropsychopharmacology. 2014;39:1303–14. https://doi.org/10.1038/npp.2014.28.
Baldermann JC, Melzer C, Zapf A, Kohl S, Timmermann L, Tittgemeyer M, et al. Connectivity profile predictive of effective deep brain stimulation in obsessive-compulsive disorder. Biol Psychiatry. 2019;85:735–43. https://doi.org/10.1016/j.biopsych.2018.12.019.
Lee DJ, Dallapiazza RF, De Vloo P, Elias GJB, Fomenko A, Boutet A, et al. Inferior thalamic peduncle deep brain stimulation for treatment-refractory obsessive-compulsive disorder: A phase 1 pilot trial. Brain Stimulation. 2019;12:344–52. https://doi.org/10.1016/j.brs.2018.11.012.
Lebow MA, Chen A. Overshadowed by the amygdala: the bed nucleus of the stria terminalis emerges as key to psychiatric disorders. Mol Psychiatry. 2016;21:450–63. https://doi.org/10.1038/mp.2016.1.
Suetens K, Nuttin B, Gabriëls L, Van Laere K. Differences in metabolic network modulation between capsulotomy and deep-brain stimulation for refractory obsessive-compulsive disorder. J Nucl Med. 2014;55:951–9. https://doi.org/10.2967/jnumed.113.126409.
Graat I, Mocking RJT, Liebrand LC, van den Munckhof P, Bot M, Schuurman PR, et al. Tractography-based versus anatomical landmark-based targeting in vALIC deep brain stimulation for refractory obsessive-compulsive disorder. Mol Psychiatry. 2022;27:5206–12. https://doi.org/10.1038/s41380-022-01760-y.
Meyer DM, Spanier S, Kilian HM, Reisert M, Urbach H, Sajonz BE, et al. Efficacy of superolateral medial forebrain bundle deep brain stimulation in obsessive-compulsive disorder. Brain Stimulation. 2022;15:582–5. https://doi.org/10.1016/j.brs.2022.03.004.
Voon V, Droux F, Morris L, Chabardes S, Bougerol T, David O, et al. Decisional impulsivity and the associative-limbic subthalamic nucleus in obsessive-compulsive disorder: stimulation and connectivity. Brain. 2017;140:442–56. https://doi.org/10.1093/brain/aww309.
Jiménez F, Nicolini H, Lozano AM, Piedimonte F, Salín R, Velasco F. Electrical stimulation of the inferior thalamic peduncle in the treatment of major depression and obsessive compulsive disorders. World Neurosurg. 2013;80:S30.e17–S30.e25. https://doi.org/10.1016/j.wneu.2012.07.010.
Welter M-L, Alves Dos Santos JF, Clair A-H, Lau B, Diallo HM, Fernandez-Vidal S, et al. Deep brain stimulation of the subthalamic, accumbens, or caudate nuclei for patients with severe obsessive-compulsive disorder: a randomized crossover controlled study. Biol Psychiatry. 2021;90:e45–7. https://doi.org/10.1016/j.biopsych.2020.07.013.
Funding
This work is funded by the National Natural Science Foundation of China (82501753, 82171442 and 82171309).
Author information
Authors and Affiliations
Contributions
Conceptualization and supervision: JGZ and ZW; Investigation and writing original draft: TX, YJQ, and XZL; Data curation: MJX and HTX, software and formal analysis: WW and ZQC; Methodology and visualization: YTB; Review and editing: JGZ and ZW; Validation: ACY and FGM. Resources and Funding Acquisition: ZW. All authors have read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Xue, T., Qiu, Y., Li, X. et al. Comparative efficacy and safety of different surgical strategies for refractory obsessive-compulsive disorder: evidence from network meta-analysis. Mol Psychiatry (2026). https://doi.org/10.1038/s41380-025-03438-7
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41380-025-03438-7