Abstract
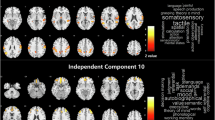
Social cognitive impairments, including theory of mind (ToM), in schizophrenia more strongly predict functional outcomes than psychotic symptoms or nonsocial cognitive deficits. Despite their clinical importance, current medications do not improve these deficits. The current study investigated the hypothesis that oxytocin, a neuropeptide implicated in social behavior, would normalize neural abnormalities in schizophrenia during ToM, and that this normalization would correlate improvement in ToM behavior. In this cross-over, double-blind, and placebo-controlled functional magnetic resonance imaging study, a single dose of 40 IU of oxytocin was administered via nasal spray to male individuals with a schizophrenia spectrum disorder (schizophrenia and schizoaffective disorder, n = 23) and healthy controls (n = 25). Participants completed two ToM tasks in the scanner, the False Belief and Person Description tasks. During both tasks, on placebo day, schizophrenia was associated with reduced accuracy, hypo-activity in the right temporo-parietal junction (rTPJ; extended into the posterior superior temporal sulcus), and hypo-connectivity between the rTPJ and medial prefrontal cortex (mPFC) compared to healthy controls. Oxytocin, relative to placebo, significantly increased accuracy and rTPJ activation for ToM but not control stories in schizophrenia. Furthermore, a significant positive correlation was found between oxytocin induced increases in rTPJ activity and accuracy, indicating that oxytocin improved rTPJ activity in schizophrenia predicted behavioral improvement. Oxytocin also significantly improved connectivity between rTPJ and mPFC in schizophrenia. These findings suggest that rTPJ activity during ToM might be a potential neural target for the treatment of social cognitive deficits in schizophrenia.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Fett AK, Viechtbauer W, Dominguez MD, Penn DL, van Os J, Krabbendam L. The relationship between neurocognition and social cognition with functional outcomes in schizophrenia: a meta-analysis. Neurosci Biobehav Rev. 2011;35:573–88.
Premack DG, Woodruff G. Does the chimpanzee have a theory of mind? Behav Brain Sci. 1978;1:515–26.
Couture SM, Granholm EL, Fish SC. A path model investigation of neurocognition, theory of mind, social competence, negative symptoms, and real-world functioning in schizophrenia. Schizophr Res. 2011;125:152–60.
Mancuso F, Horan WP, Kern RS, Green MF. Social cognition in psychosis: multidimensional structure, clinical correlates, and relationship with functional outcome. Schizophr Res. 2011;125:143–51.
Kurtz MM, Richardson CL. Social cognitive training for schizophrenia: a meta-analytic investigation of controlled research. Schizophr Bull. 2012;38:1092–104.
Brunet E, Sarfati Y, Hardy-Baylé MC. Reasoning about physical causality and other’s intentions in schizophrenia. Cogn Neuropsychiatry. 2003;8:129–39.
Brüne MD. “Theory of Mind” in schizophrenia: a review of the literature. Schizophr Bull. 2005;31:21–42.
Lee Y, Quintana J, Nori P, Green MF. Theory of mind in schizophrenia: exploring neural mechanisms of belief attribution. Soc Neurosci. 2011;6:569–81.
Das P, Lagopoulos J, Coulston CM, Henderson AF, Malhi GS. Mentalizing impairment in schizophrenia: a functional MRI study. Schizophr Res. 2012;134:158–64.
Dodell-Feder D, DeLisi LE, Hooker CI. Neural disruption to theory of mind predicts daily social functioning in individuals at familial high-risk for schizophrenia. Soc Cogn Affect Neurosci. 2014a;9:1914–25.
Dodell-Feder D, Tully LM, Lincoln SH, Hooker CI. The neural basis of theory of mind and its relationship to social functioning and social anhedonia in individuals with schizophrenia. Neuroimage Clin. 2014b;4:154–63.
Kucharska-Pietura K, Mortimer A. Can antipsychotics improve social cognition in patients with schizophrenia? CNS Drugs. 2013;27:335–43.
Kosfeld M, Heinrichs M, Zak PJ, Fischbacher U, Fehr E. Oxytocin increases trust in humans. Nature. 2005;435:673–6.
Baumgartner T, Heinrichs M, Volanthen A, Fischbacher U, Fehr E. Oxytocin shapes the neural circuitry of trust and trust adaptation in humans. Neuron. 2008;58:639–50.
Kéri S, Benedek G. Oxytocin enhances the perception of biological motion in humans. Cogn Affect Behav Neurosci. 2009;9:237–41.
Hurlemann R, Patin A, Onur OA, Cohen MX, Baumgartner T, Metzler S, et al. Oxytocin enhances amygdala dependent, socially reinforced learning and emotional empathy in humans. J Neurosci. 2010;30:4999–5007.
Marsh AA, Yu HH, Pine DS, Blair RJR. Oxytocin improves specific recognition of positive facial expressions. Psychopharmacology. 2010;209:225–32.
Perry A, Bentin S, Shalev I, Israel S, Uzefovsky F, Bar-On D, et al. Intranasal oxytocin modulates EEG mu/alpha and beta rhythms during perception of biological motion. Psychoneuroendocrinology. 2010;35:1446–53.
Pederson CA, Gibson CM, Rau SW, Salimi K, Smedley KL, Casey RL, et al. Intranasal oxytocin reduces psychotic symptoms and improves theory of mind and social perception in schizophrenia. Schizophr Res. 2011;132:50–3.
Davis MC, Lee J, Horan WP, Clarke AD, McGee MR, Green MF, et al. Effects of single dose intranasal oxytocin on social cognition in schizophrenia. Schizophr Res. 2013;147:393–7.
Woolley JD, Chuang B, Lam O, Lai W, O’Donovan A, Rankin KP, et al. Oxytocin administration enhances controlled social cognition in patients with schizophrenia. Psychoneuroendocrinology. 2014;47:116–25.
Bradley ER, Woolley JD. oxytocin effects in schizophrenia: reconciling mixed findings and moving forward. Neurosci Biobehav Rev. 2017;80:36–56.
Williams D, Bürkner P. Effects of intranasal oxytocin on symptoms of schizophrenia: a multivariate Bayesian meta-analysis. Psychoneuroendocrinology. 2017;75:141–51.
Insel TR. Translating oxytocin neuroscience to the clinic: a National Institute of Mental Health perspective. Biol Psychiatry. 2016;79:153–4.
Shin NY, Park HY, Jung WH, Park JW, Yun JY, Jang JH, et al. Effects of oxytocin on neural response to facial expressions in patients with schizophrenia. Neuropsychopharmacology. 2015;40:1919–27.
Dey A, Rao N. Effects of oxytocin on neural response to facial emotion recognition in schizophrenia. Schizophr Bull. 2017;43:S75–S76.
Bora E, Yucel M, Pantelis C. Theory of mind impairment in schizophrenia: meta-analysis. Schizophr Res. 2009;109:1–9.
Chung YS, Barch D, Strube M. A meta-analysis of mentalizing impairments in adults with schizophrenia and autism spectrum disorder. Schizophr Bull. 2013;40:602–16.
Roux P, Smith P, Passerieux C, Ramus F. Preserved implicit mentalizing in schizophrenia despite poor explicit performance: evidence from eye tracking. Sci Rep. 2016;6:1–9.
Wimmer H, Perner J. Beliefs about beliefs: representation and constraining function of wrong beliefs in young children’s understanding of deception. Cognition. 1983;13:103–28.
Saxe R, Kanwisher N. People thinking about thinking people: the role tempo-parietal junction “theory mind”. Neuroimage. 2003;19:1835–42.
Saxe R, Powell LJ. It’s the thought that counts: specific brain regions for one component of theory of mind. Psychol Sci. 2006;17:692–9.
Meyer-Lindenberg A, Domes G, Kirsch P, Heinrichs M. Oxytocin and vasopressin in the human brain: social neuropeptides for translational medicine. Nat Rev Neurosci. 2011;12:524–38.
Feifel D, Macdonald K, Nguyen A, Cobb P, Warlan H, Galangue B, et al. Adjunctive intranasal oxytocin reduces symptoms in schizophrenia patients. Biol Psychiatry. 2010;68:678–80.
Dodell-Feder D, Koster-Hale J, Bedny M, Saxe R. fMRI item analysis in a theory of mind task. Neuroimage. 2011;55:705–12.
R core team (2018). R: A language and environment for statistical computing. R foundation for Statistical Computing, Vienna, Austria. https://www.R-project.org/.
McLaren DG, Ries ML, Xu G, Johnson SC. A generalized form of context-dependent psychophysiological interactions (gPPI): a comparison to standard approaches. Neuroimage. 2012;61:1277–86.
Saxe R, Wexler A. Making sense of another mind: the role of the right temporo-parietal junction. Neuropsychologia. 2005;43:1391–9.
Moessnang C, Otto K, Bilek E, Schäfer A, Baumeister S, Hohmann S, et al. Differential responses to the dorsomedial prefrontal cortex and right posterior superior temporal sulcus to spontaneous mentalizing. Hum Brain Mapp. 2017;38:3791–803.
Hein G, Knight RT. Superior temporal sulcus—it’s my area: or is it? J Cogn Neurosci. 2008;20:2125–36.
Mier D, Eisenacher S, Rausch F, Englisch S, Gerchen MF, Zamoscik V, et al. Aberrant activity and connectivity of the posterior superior sulcus during social cognition in schizophrenia. Eur Arch Psychiatry Clin Neurosci. 2017;267:597–610.
Kronbichler L, Tschernegg M, Martin AI, Schurz M, Kronbichler M. Abnormal brain activation during theory of mind tasks in schizophrenia: a meta-analysis. Schizophr Bull. 2017;43:1240–50.
Xin F, Zhou F, Zhou X, Ma X, Geng Y, Zhao W, et al. Oxytocin modulates the intrinsic dynamics between attention-related large-scale networks. Cerebral Cortex. 2018;bhy295. https://doi.org/10.1093/cercor/bhy295.
Djupesland PG. Nasal drug delivery devices: characteristics and performance in a clinical perspective—a review. Drug Deliv Transl Res. 2013;3:42–62.
Leng G, Ludwig M. Intranasal oxytocin: myths and delusions. Biol Psychiatry. 2016;79:243–50.
Quintana DS, Woolley JD. Intranasal oxytocin mechanisms can be better understood but its effects on social cognition and behavior are not to be sniffed at. Biol Psychiatry. 2016;79:e49–e50.
Neumann ID, Landgraf R. Balance of brain oxytocin and vasopressin: implications for anxiety, depression, and social behaviors. Trends Neurosci. 2012;35:649–59.
Bartz JA, Zaki J, Bolger N, Oschner KN. Social effects of oxytocin in humans: context and person matter. Trends Cogn Sci. 2011;15:301–9.
Shen H. Neuroscience: the hard science of oxytocin. Nature. 2015;522:410–2.
Aoki Y, Yahata N, Watanabe T, Takano Y, Kawakubo Y, Kuwabara H, et al. Oxytocin improves behavioral and neural deficits in inferring others’ social emotions in autism. Brain. 2014;137:3073–86.
Acknowledgements
The authors would like to thank Christine Hooker for providing the stimulus materials.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
De Coster, L., Lin, L., Mathalon, D.H. et al. Neural and behavioral effects of oxytocin administration during theory of mind in schizophrenia and controls: a randomized control trial. Neuropsychopharmacol. 44, 1925–1931 (2019). https://doi.org/10.1038/s41386-019-0417-5
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41386-019-0417-5
This article is cited by
-
The medial prefrontal cortex as a proposed regulatory structure in the relationship between anxiety and perceived social support: a review
BMC Psychology (2025)
-
Linking childhood trauma to the psychopathology of schizophrenia: the role of oxytocin
Schizophrenia (2024)
-
The Role of Intranasal Oxytocin on Social Cognition: an Integrative Human Lifespan Approach
Current Behavioral Neuroscience Reports (2020)