Abstract
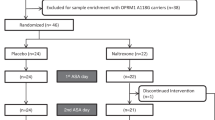
Glutamate and opioid systems play important roles in alcohol drinking behaviors. We examined if combined treatment with the NMDA antagonist memantine and the opioid antagonist naltrexone, when compared with naltrexone alone, would have a greater influence on alcohol drinking behaviors. Fifty-six, non-treatment-seeking heavy drinkers, with alcohol dependence and a positive family history (FHP) of alcoholism, participated in a randomized, double-blind, crossover trial, including two 6–8 days treatment periods, separated by a 6-day washout, and 3 alcohol drinking paradigm (ADP) sessions. After the first baseline (BAS) ADP1 session, participants were randomized to receive either naltrexone (NTX; 50 mg/day) + placebo memantine, or NTX (50 mg/day) + memantine (MEM; 20 mg/day), during the first treatment period, following which they completed ADP2. After a 6-day washout, participants were crossed over to the treatment they did not receive during the first treatment period, following which they completed ADP3. During each ADP, participants received a priming drink of alcohol followed by 3 1-hour, self-administration periods during which they had ad-lib access to 12 drinks. Individually, both NTX and NTX + MEM, when compared to BAS ADP1, significantly reduced the number of drinks consumed (p’s < 0.001) and craving (p’s < 0.001). When comparing NTX + MEM vs. NTX on number of drinks consumed, there was a significant treatment* sequence interaction (p = 0.004). Specifically, when NTX + MEM followed NTX alone, NTX + MEM resulted in a further reduction in drinking (mean: −1.94; 95% CI: −2.6, −0.8, p = 0.0005). However, when NTX alone followed NTX + MEM, NTX alone did not lead to further reduction in drinking (mean: 0.59; 95% CI: −0.67, 1.43, p = 0.47). Similar patterns were observed for alcohol craving; specifically, a significant reduction in craving was observed when NTX + MEM followed NTX alone (p = 0.009), but craving reduction was maintained when NTX + MEM was followed by NTX alone. Neither treatment condition significantly influenced alcohol-induced stimulation or sedation. Memantine (at a dose of 20 mg/day) enhances the efficacy of naltrexone (50 mg/day) in reducing alcohol drinking and craving among FHP drinkers with beneficial effects that appear to carryover after discontinuation of memantine treatment.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Grant KA, Lovinger DM. Cellular and behavioral neurobiology of alcohol: receptor-mediated neuronal processes. Clin Neurosci. 1995;3:155–64.
Gass JT, Olive MF. Glutamatergic substrates of drug addiction and alcoholism. Biochem Pharm. 2008;75:218–65.
Woodward JJ. Ionotropic glutamate receptors as sites of action for ethanol in the brain. Neurochem Int. 1999;35:107–13.
Krystal JH, Petrakis IL, Mason G, Trevisan L, D’Souza DC. N-methyl-D-aspartate glutamate receptors and alcoholism: reward, dependence, treatment, and vulnerability. Pharm Ther. 2003a;99:79–94.
Petrakis IL, Limoncelli D, Gueorguieva R, Jatlow P, Boutros NN, Trevisan L, et al. Altered NMDA glutamate receptor antagonist response in individuals with a family vulnerability to alcoholism. Am J Psychiatry. 2004;161:1776–82.
Yoon G, Pittman B, Limoncelli D, Krystal JH, Petrakis IL. Familial alcoholism risk and the ratio of stimulant to sedative effects of ketamine. Biol Psychiatry. 2016;79:e69–70.
Krystal JH, Petrakis IL, Trevisan L, D’Souza DC. NMDA receptor antagonism and the ethanol intoxication signal: From alcoholism risk to pharmacotherapy. Ann N Y Acad Sci. 2003b;1003:176–84.
Acosta G, Hasenkamp W, Daunais JB, Friedman DP, Grant KA, Hemby SE. Ethanol self-administration modulation of NMDA receptor subunit and related synaptic protein mRNA expression in prefrontal cortical fields in cynomolgus monkeys. Brain Res. 2010;1318:144–54.
Clapp P, Gibson ES, Dell’acqua ML, Hoffman PL. Phosphorylation regulates removal of synaptic N-methyl-D-aspartate receptors after withdrawal from chronic ethanol exposure. J Pharm Exp Ther. 2010;332:720–9.
Roberto M, Varodayan FP. Synaptic targets: chronic alcohol actions. Neuropharmacology. 2017;122:85–99.
Prisciandaro JJ, Schacht JP, Prescot AP, Brenner HM, Renshaw PF, Brown TR, et al. Intraindividual changes in brain GABA, glutamate, and glutamine during monitored abstinence from alcohol in treatment-naive individuals with alcohol use disorder. Addict Biol. 2019;1:e12810.
Escher T, Call SB, Blaha CD, Mittleman G. Behavioral effects of aminoadamantane class NMDA receptor antagonists on schedule-induced alcohol and self-administration of water in mice. Psychopharmacol (Berl). 2006;187:424–34.
Krupitsky EM, Neznanova O, Masalov D, Burakov AM, Didenko T, Romanova T, et al. Effect of memantine on cue-induced alcohol craving in recovering alcohol-dependent patients. Am J Psychiatry. 2007a;164:519–23.
Krupitsky EM, Rudenko AA, Burakov AM, Slavina TY, Grinenko AA, Pittman B, et al. Antiglutamatergic strategies for ethanol detoxification: comparison with placebo and diazepam. Alcohol Clin Exp Res. 2007b;31:604–11.
Arias AJ, Feinn R, Covault J, Kranzler HR. Memantine for alcohol dependence: an open-label pilot study. Addictive Disord Their Treat. 2007;6:77–83.
Bisaga A, Evans SM. Acute effects of memantine in combination with alcohol in moderate drinkers. Psychopharmacol (Berl). 2004;172:16–24.
Lee SY, Wang TY, Chen SL, Chang YH, Chen PS, Huang SY, et al. Add-on memantine treatment for bipolar II disorder comorbid with alcohol dependence: a 12-week follow-up study. Alcohol Clin Exp Res. 2018;42:1044–50.
Jamadar S, DeVito EE, Jiantonio RE, Meda SA, Stevens MC, Potenza MN, et al. Memantine, an NMDA receptor antagonist, differentially influences Go/No-Go performance and fMRI activity in individuals with and without a family history of alcoholism. Psychopharmacol (Berl). 2012;222:129–40.
Krishnan-Sarin S, O’Malley SS, Franco N, Cavallo DA, Morean M, Shi J, et al. N-methyl-D-aspartate receptor antagonism has differential effects on alcohol craving and drinking in heavy drinkers. Alcohol Clin Exp Res. 2015;39:300–7.
Alasmari F, Goodwani S, McCullumsmith RE, Sari Y. Role of glutamatergic system and mesocorticolimbic circuits in alcohol dependence. Prog Neurobiol. 2018;171:32–49.
Koob GF, Volkow ND. Neurobiology of addiction: a neurocircuitry analysis. Lancet Psychiatry. 2016;3:760–73.
Chartoff EH, Connery HS. It’s MORe exciting than mu: crosstalk between mu opioid receptors and glutamatergic transmission in the mesolimbic dopamine system. Front Pharm. 2014;5:116.
Gracy KN, Svingos AL, Pickel VM. Dual ultrastructural localization of mu-opioid receptors and NMDA-type glutamate receptors in the shell of the rat nucleus accumbens. J Neurosci. 1997;17:4839–48.
Huang J, Wang H, Pickel VM. Rostrocaudal variation in targeting of N-methyl-D-aspartate and mu-opioid receptors in the rat medial nucleus of the solitary tract. J Comp Neurol. 2000;421:400–11.
Danysz W, Kozela E, Parsons CG, Sladek M, Bauer T, Popik P. Peripherally acting NMDA receptor/glycineB site receptor antagonists inhibit morphine tolerance. Neuropharmacology. 2005;48:360–71.
Harris AC, Rothwell PE, Gewirtz JC. Effects of the NMDA receptor antagonist memantine on the expression and development of acute opiate dependence as assessed by withdrawal-potentiated startle and hyperalgesia. Psychopharmacol (Berl). 2008;196:649–60.
Popik P, Kozela E, Danysz W. Clinically available NMDA receptor antagonists memantine and dextromethorphan reverse existing tolerance to the antinociceptive effects of morphine in mice. Naunyn Schmiedebergs Arch Pharm. 2000;361:425–32.
Trujillo KA, Akil H. Inhibition of morphine tolerance and dependence by the NMDA receptor antagonist MK-801. Science. 1991;251:85–87.
Trujillo KA, Akil H. Inhibition of opiate tolerance by non-competitive N-methyl-D-aspartate receptor antagonists. Brain Res. 1994;633:178–88.
Krystal JH, Madonick S, Perry E, Gueorguieva R, Brush L, Wray Y, et al. Potentiation of low dose ketamine effects by naltrexone: potential implications for the pharmacotherapy of alcoholism. Neuropsychopharmacology. 2006;31:1793–800.
Nie Z, Yuan X, Madamba SG, Siggins GR. Ethanol decreases glutamatergic synaptic transmission in rat nucleus accumbens in vitro: naloxone reversal. J Pharm Exp Ther. 1993;266:1705–12.
Krishnan-Sarin S, Krystal JH, Shi J, Pittman B, O’Malley SS. Family history of alcoholism influences naltrexone-induced reduction in alcohol drinking. Biol Psychiatry. 2007;62:694–7.
Reus VI, Fochtmann LJ, Bukstein O, Eyler AE, Hilty DM, Horvitz-Lennon M, et al. The American Psychiatric Association Practice Guideline for the pharmacological treatment of patients with alcohol use disorder. Am J Psychiatry. 2018;175:86–90.
George DT, Herion DW, Jones CL, Phillips MJ, Hersh J, Hill D, et al. Rimonabant (SR141716) has no effect on alcohol self-administration or endocrine measures in nontreatment-seeking heavy alcohol drinkers. Psychopharmacol (Berl). 2010;208:37–44.
Anton RF, Drobes DJ, Voronin K, Durazo-Avizu R, Moak D. Naltrexone effects on alcohol consumption in a clinical laboratory paradigm: temporal effects of drinking. Psychopharmacol (Berl). 2004;173:32–40.
McKee SA, Harrison EL, O’Malley SS, Krishnan-Sarin S, Shi J, Tetrault JM, et al. Varenicline reduces alcohol self-administration in heavy-drinking smokers. Biol Psychiatry. 2009;66:185–90.
McKee SA, O’Malley SS, Shi J, Mase T, Krishnan-Sarin S. Effect of transdermal nicotine replacement on alcohol responses and alcohol self-administration. Psychopharmacol (Berl). 2008;196:189–200.
O’Malley SS, Krishnan-Sarin S, Farren C, Sinha R, Kreek MJ. Naltrexone decreases craving and alcohol self-administration in alcohol-dependent subjects and activates the hypothalamo-pituitary-adrenocortical axis. Psychopharmacol (Berl). 2002;160:19–29.
Voronin K, Randall P, Myrick H, Anton R. Aripiprazole effects on alcohol consumption and subjective reports in a clinical laboratory paradigm–possible influence of self-control. Alcohol Clin Exp Res. 2008;32:1954–61.
NACAA. Recommended council guidelines on ethyl alcohol adminstration in human experimentation. 2006. https://www.niaaa.nih.gov/Resources/ResearchResources/job22.htm.
Sobell L, Sobell M. Timeline Follow-back: A technique for assessing self-reported alcohol consumption. In: Litten R, Allen J, (eds). Measuring alcohol consumption:psychological and biological methods. New Jersey: Humana Press; 1992. p. 41–72.
Rice JP, Reich T, Bucholz KK, Neuman RJ, Fishman R, Rochberg N, et al. Comparison of direct interview and family history diagnoses of alcohol dependence. Alcohol Clin Exp Res. 1995;19:1018–23.
First MB, Spitzer RL, Gibbon M, Williams, JB. Structured llinical interview for the DSM-IV Axis I disorders. 1996.
Sullivan JT, Sykora K, Schneiderman J, Naranjo CA, Sellers EM. Assessment of alcohol withdrawal: the revised clinical institute withdrawal assessment for alcohol scale (CIWA-Ar). Br J Addict. 1989;84:1353–7.
Watson PE (1989). Total body water and alcohol levels:updating the fundamentals. In: Krow KE, Batt RD (eds). Human metabolism of alcohol. CRC press, pp. 41-66.
Bohn MJ, Krahn DD, Staehler BA. Development and initial validation of a measure of drinking urges in abstinent alcoholics. Alcohol Clin Exp Res. 1995;19:600–6.
Martin CS, Earleywine M, Musty RE, Perrine MW, Swift RM. Development and validation of the Biphasic Alcohol Effects Scale. Alcohol Clin Exp Res. 1993;17:140–6.
Rueger SY, King AC. Validation of the brief Biphasic Alcohol Effects Scale (B-BAES). Alcohol Clin Exp Res. 2013;37:470–6.
Morean ME, DeMartini KS, Leeman RF, Pearlson GD, Anticevic A, Krishnan-Sarin S, et al. Psychometrically improved, abbreviated versions of three classic measures of impulsivity and self-control. Psychol Assess. 2014;26:1003–20.
Levine J, Schooler NR. SAFTEE: a technique for the systematic assessment of side effects in clinical trials. Psychopharmacol Bull. 1986;22:343–81.
Ross HE, Gavin DR, Skinner HA. Diagnostic validity of the MAST and the alcohol dependence scale in the assessment of DSM-III alcohol disorders. J Stud Alcohol. 1990;51:506–13.
Croop RS, Faulkner EB, Labriola DF. The safety profile of naltrexone in the treatment of alcoholism. Results from a multicenter usage study. The Naltrexone Usage Study Group. Arch Gen Psychiatry. 1997;54:1130–5.
Gomolin IH, Smith C, Jeitner TM. Once-daily memantine: pharmacokinetic and clinical considerations. J Am Geriatr Soc. 2010;58:1812–3.
Liu MY, Meng SN, Wu HZ, Wang S, Wei MJ. Pharmacokinetics of single-dose and multiple-dose memantine in healthy chinese volunteers using an analytic method of liquid chromatography-tandem mass spectrometry. Clin Ther. 2008;30:641–53.
Noetzli M, Eap CB. Pharmacodynamic, pharmacokinetic and pharmacogenetic aspects of drugs used in the treatment of Alzheimer’s disease. Clin Pharmacokinet. 2013;52:225–41.
Periclou A, Ventura D, Rao N, Abramowitz W. Pharmacokinetic study of memantine in healthy and renally impaired subjects. Clin Pharm Ther. 2006;79:134–43.
Danysz W, Parsons CG, Kornhuber J, Schmidt WJ, Quack G. Aminoadamantanes as NMDA receptor antagonists and antiparkinsonian agents–preclinical studies. Neurosci Biobehav Rev. 1997;21:455–68.
Schmidt WJ, Zadow B, Kretschmer BD, Hauber W. Anticataleptic potencies of glutamate-antagonists. Amino Acids. 1991;1:225–37.
Wenk GL, Danysz W, Mobley SL. MK-801, memantine and amantadine show neuroprotective activity in the nucleus basalis magnocellularis. Eur J Pharm. 1995;293:267–70.
Luckenbaugh DA, Ibrahim L, Brutsche N, Franco-Chaves J, Mathews D, Marquardt CA, et al. Family history of alcohol dependence and antidepressant response to an N-methyl-D-aspartate antagonist in bipolar depression. Bipolar Disord. 2012;14:880–7.
Niciu MJ, Luckenbaugh DA, Ionescu DF, Richards EM, Vande Voort JL, Ballard ED, et al. Ketamine’s antidepressant efficacy is extended for at least four weeks in subjects with a family history of an alcohol use disorder. Int J Neuropsychopharmacol. 2014;18:pii: pyu039.
Phelps LE, Brutsche N, Moral JR, Luckenbaugh DA, Manji HK, Zarate CA Jr. Family history of alcohol dependence and initial antidepressant response to an N-methyl-D-aspartate antagonist. Biol Psychiatry. 2009;65:181–4.
Fink K, Gothert M. Both ethanol and ifenprodil inhibit NMDA-evoked release of various neurotransmitters at different, yet proportional potency: potential relation to NMDA receptor subunit composition. Naunyn Schmiedebergs Arch Pharm. 1996;354:312–9.
Kash TL, Matthews RT, Winder DG. Alcohol inhibits NR2B-containing NMDA receptors in the ventral bed nucleus of the stria terminalis. Neuropsychopharmacology. 2008;33:1379–90.
Lovinger DM. Developmental decrease in ethanol inhibition of N-methyl-D-aspartate receptors in rat neocortical neurons: relation to the actions of ifenprodil. J Pharm Exp Ther. 1995;274:164–72.
Bisaga A, Comer SD, Ward AS, Popik P, Kleber HD, Fischman MW. The NMDA antagonist memantine attenuates the expression of opioid physical dependence in humans. Psychopharmacol (Berl). 2001;157:1–10.
Gonzalez G, DiGirolamo G, Romero-Gonzalez M, Smelson D, Ziedonis D, Kolodziej M. Memantine improves buprenorphine/naloxone treatment for opioid dependent young adults. Drug Alcohol Depend. 2015;156:243–53.
Bisaga A, Sullivan MA, Cheng WY, Carpenter KM, Mariani JJ, Levin FR, et al. A placebo controlled trial of memantine as an adjunct to oral naltrexone for opioid dependence. Drug Alcohol Depend. 2011;119:e23–29.
Bisaga A, Sullivan MA, Glass A, Mishlen K, Carpenter KM, Mariani JJ, et al. A placebo-controlled trial of memantine as an adjunct to injectable extended-release naltrexone for opioid dependence. J Subst Abus Treat. 2014;46:546–52.
Chen SL, Tao PL, Chu CH, Chen SH, Wu HE, Tseng LF, Hong JS, Lu RB. Low-dose memantine attenuated morphine addictive behavior through its anti-inflammation and neurotrophic effects in rats. J Neuroimmune Pharmacol. 2012;7:444–53..
Ray LA, Bujarski S, Yardley MM, Roche DJO, Hartwell EE. Differences between treatment-seeking and non-treatment-seeking participants in medication studies for alcoholism: do they matter? Am J Drug Alcohol Abus. 2017;43:703–10.
Rohn MC, Lee MR, Kleuter SB, Schwandt ML, Falk DE, Leggio L. Differences between treatment-seeking and nontreatment-seeking alcohol-dependent research participants: an exploratory analysis. Alcohol Clin Exp Res. 2017;41:414–20.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Krishnan-Sarin, S., O’Malley, S.S., Franco, N. et al. Influence of combined treatment with naltrexone and memantine on alcohol drinking behaviors: a phase II randomized crossover trial. Neuropsychopharmacol. 45, 319–326 (2020). https://doi.org/10.1038/s41386-019-0536-z
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41386-019-0536-z
This article is cited by
-
Predicting individual treatment response in alcohol use disorders: a reverse translational proof-of-concept study
Translational Psychiatry (2025)
-
Memantine: updates from the past decade and implications for future novel therapeutic applications
Journal of Neural Transmission (2025)
-
Quadruple pharmacotherapy for alcohol use disorder tolerable yet insufficient: a case report
Substance Abuse Treatment, Prevention, and Policy (2024)
-
Application of Real-World Data and the REWARD Framework to Detect Unknown Benefits of Memantine and Identify Potential Disease Targets for New NMDA Receptor Antagonists
CNS Drugs (2021)