Abstract
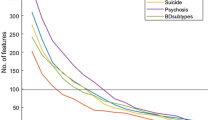
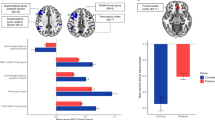
Bipolar disorder (BD) is a chronic condition characterized by recurrent mood episodes and persistent cognitive deficits that span multiple domains, ultimately impacting daily functioning. Understanding the neural underpinnings of these impairments is crucial. In a systematic review and meta-analysis examining 80 studies (with 50 meeting criteria for meta-analysis) of adults with BD, relationships between structural brain measures and cognitive performance were evaluated. Participants were diagnosed according to standard criteria, underwent structural and diffusion-weighted MRI, and completed standardized cognitive assessments. The meta-analyses indicated significant associations between both grey matter and white matter indices and cognitive functioning, reflected in moderate effect sizes. Notably, these associations exhibited substantial heterogeneity. Meta-regression revealed that bipolar subtype and current mood state moderated the observed brain-cognition relationships, with bipolar I and euthymic individuals showing higher associations with grey matter metrics. Cognitive domain differences also played a key role, indicating that certain cognitive functions are more strongly linked to structural brain measures than others. Brain networks emerged as a global influence on cognition, with limited differences in pairwise comparisons. Age, sex, psychosis, and mania were not found to significantly moderate these relationships. Overall, this work suggests that structural alterations in grey and white matter in individuals with BD may contribute meaningfully to cognitive difficulties, while brain networks may provide a broad integrative framework for these associations. These findings underscore the importance of considering both global and specific neural factors when exploring the pathophysiology of cognitive impairment in BD.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 13 print issues and online access
$259.00 per year
only $19.92 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
Extracted data is included in the supplemental information.
References
Bourne C, Aydemir Ö, Balanzá-Martínez V, Bora E, Brissos S, Cavanagh JT, et al. Neuropsychological testing of cognitive impairment in euthymic bipolar disorder: An individual patient data meta-analysis. Acta Psychiatr Scand. 2013;128:149–62.
Lopes R, Fernandes L. Bipolar disorder: clinical perspectives and implications with cognitive dysfunction and dementia. Depress Res Treat. 2012;2012:275957.
Jones BDM, Fernandes BS, Husain MI, Ortiz A, Rajji TK, Blumberger DM, et al. A cross-sectional study of cognitive performance in bipolar disorder across the lifespan: the cog-BD project. Psychol Med 1–9 2022 https://doi.org/10.1017/S0033291722003622.
Favre P, Pauling M, Stout J, Hozer F, Sarrazin S, Abé C, et al. Widespread white matter microstructural abnormalities in bipolar disorder: evidence from mega- and meta-analyses across 3033 individuals. Neuropsychopharmacology. 2019;44:2285–93.
Hibar DP, Westlye LT, Doan NT, Jahanshad N, Cheung JW, Ching CRK, et al. Cortical abnormalities in bipolar disorder: an MRI analysis of 6503 individuals from the ENIGMA Bipolar Disorder Working Group. Mol Psychiatry. 2018;23:932.
Van Rheenen TE, Lewandowski KE, Bauer IE, Kapczinski F, Miskowiak K, Burdick KE, et al. Current understandings of the trajectory and emerging correlates of cognitive impairment in bipolar disorder: An overview of evidence. Bipolar Disord. 2020;22:13–27.
Mesbah R, Koenders MA, van der Wee NJA, Giltay EJ, van Hemert AM, de Leeuw M. Association between the fronto-limbic network and cognitive and emotional functioning in individuals with bipolar disorder: a systematic review and meta-analysis. JAMA Psychiatry. 2023;80:432–40.
Schumer MC, Chase HW, Rozovsky R, Eickhoff SB, Phillips ML. Prefrontal, parietal, and limbic condition-dependent differences in bipolar disorder: a large-scale meta-analysis of functional neuroimaging studies. Mol Psychiatry. 2023;28:2826–38.
Caruana GF, Carruthers SP, Berk M, Rossell SL, Van Rheenen TE. To what extent does white matter map to cognition in bipolar disorder? A systematic review of the evidence. Prog Neuropsychopharmacol Biol Psychiatry. 2024;128:110868.
Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (prisma-p) 2015: Elaboration and explanation. BMJ 2015. https://doi.org/10.1136/bmj.g7647.
Association, A. P. Diagnostic and statistical manual of mental disorders: DSM-5. 2013.
WHO. The ICD-10 Classification of Mental and Behavioural Disorders Clinical Descriptions and Diagnostic Guidelines World Health Organization.
Nuechterlein KH, Green MF, Kern RS, Baade LE, Barch DM, Cohen JD, et al. The MATRICS consensus cognitive battery, part 1: Test selection, reliability, and validity. Am J Psychiatry. 2008;165:203–13.
Young RC, Biggs JT, Ziegler VE, Meyer DA. A rating scale for mania: Reliability, validity and sensitivity. Br J Psychiatry. 1978;133:429–35.
Montgomery SA, Asberg M. A new depression scale designed to be sensitive to change. Br J Psychiatry. 1979;134:382–9.
Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62.
Yeo BT, Krienen FM, Sepulcre J, Sabuncu MR, Lashkari D, Hollinshead M, et al. The organization of the human cerebral cortex estimated by intrinsic functional connectivity. J Neurophysiol. 2011;106:1125–65.
Wakana S, Jiang H, Nagae-Poetscher LM, van Zijl PCM, Mori S. Fiber tract-based atlas of human white matter anatomy. Radiology. 2004;230:77–87.
Wells G Shea B, O’Connell D, Robertson J, Peterson J, Welch V, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of non randomised studies in meta-analyses. http://www.ohrica/programs/clinical_epidemiology/oxford htm (2009).
Khalil M, Hollander P, Raucher-Chéné D, Lepage M, Lavigne KM. Structural brain correlates of cognitive function in schizophrenia: a meta-analysis. Neurosci Biobehav Rev. 2022;132:37–49.
Kanai R, Rees G. The structural basis of inter-individual differences in human behaviour and cognition. Nat Rev Neurosci. 2011;12:231–42.
Penke L, Maniega SM, Bastin ME, Hernandez V, Murray C, Royle NA, et al. Brain white matter tract integrity as a neural foundation for general intelligence. Mol Psychiatry. 2012;17:1026–30.
Park DC, Reuter-Lorenz P. The adaptive brain: aging and neurocognitive scaffolding. Annu Rev Psychol. 2009;60:173–96.
Magioncalda P, Martino M. A unified model of the pathophysiology of bipolar disorder. Mol Psychiatry. 2022;27:202–11.
Kloiber S, Rosenblat JD, Husain MI, Ortiz A, Berk M, Quevedo J, et al. Neurodevelopmental pathways in bipolar disorder. Neurosci Biobehav Rev. 2020;112:213–26.
Wu Y, Su Y-A, Zhu L, Li J, Si T. Advances in functional MRI research in bipolar disorder: from the perspective of mood states. Gen Psychiatr. 2024;37:e101398.
Wu YK, Su YA, Li L, Zhu LL, Li K, Li JT, et al. Brain functional changes across mood states in bipolar disorder: from a large-scale network perspective. Psychol Med. 2024;54:763–74.
Funding
This work was supported by a CIHR Postdoctoral Fellowship to BDMJ.
Author information
Authors and Affiliations
Contributions
All co-authors contributed to the conception of the work, drafting the work, and final approval of the version published.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Jones, B.D.M., Gallucci, J., Jones, O.Y. et al. Associations between structural brain measures and cognitive function in bipolar disorder: a systematic review and meta-analysis. Neuropsychopharmacol. 50, 1256–1264 (2025). https://doi.org/10.1038/s41386-025-02096-1
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41386-025-02096-1