Abstract
Background
The Neonatal Resuscitation Program recommends initial resuscitation of preterm infants with low oxygen (O2) followed by titration to target preductal saturations (SpO2). We studied the effect of resuscitation with titrated O2 on gas exchange, pulmonary, and systemic hemodynamics.
Methodology
Twenty-nine preterm lambs (127 d gestation) were randomized to resuscitation with 21% O2 (n = 7), 100% O2 (n = 6), or initiation at 21% and titrated to target SpO2 (n = 16). Seven healthy term control lambs were ventilated with 21% O2.
Results
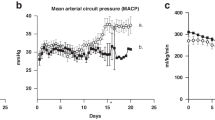
Preductal SpO2 achieved by titrating O2 was within the desired range similar to term lambs in 21% O2. Resuscitation of preterm lambs with 21% and 100% O2 resulted in SpO2 below and above the target, respectively. Ventilation of preterm lambs with 100% O2 and term lambs with 21% O2 effectively decreased pulmonary vascular resistance (PVR). In contrast, preterm lambs with 21% O2 and titrated O2 demonstrated significantly higher PVR than term lambs on 21% O2.
Conclusion(s)
Initial resuscitation with 21% O2 followed by titration of O2 led to suboptimal pulmonary vascular transition at birth in preterm lambs. Ventilation with 100% O2 in preterm lambs caused hyperoxia but reduced PVR similar to term lambs on 21% O2. Studies evaluating the initiation of resuscitation at a higher O2 concentration followed by titration based on SpO2 in preterm neonates are needed.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Perlman, J. M., et al. Neonatal Resuscitation Chapter C 2015 Part 7: Neonatal Resuscitation: 2015 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations. Circulation 132, S204–S241 (2015).
Wyckoff, M. H. et al. Part 13: Neonatal Resuscitation: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 132, S543–S560 (2015).
American Academy of Pediatrics & American Heart Association. Textbook of Neonatal Resuscitation (NRP) 7th edn, p. 326 (2016).
Armanian, A. M. & Badiee, Z. Resuscitation of preterm newborns with low concentration oxygen versus high concentration oxygen. J. Res Pharm. Pract. 1, 25–29 (2012).
Kapadia, V. S. et al. Resuscitation of preterm neonates with limited versus high oxygen strategy. Pediatrics 132, e1488–e1496 (2013).
Lundstrom, K. E., Pryds, O. & Greisen, G. Oxygen at birth and prolonged cerebral vasoconstriction in preterm infants. Arch. Dis. Child Fetal Neonatal Ed. 73, F81–F86 (1995).
Rabi, Y., Singhal, N. & Nettel-Aguirre, A. Room-air versus oxygen administration for resuscitation of preterm infants: the ROAR study. Pediatrics 128, e374–e381 (2011).
Rook, D. et al. Resuscitation of preterm infants with different inspired oxygen fractions. J. Pediatr. 164, 1322–1326 e1323 (2014).
Vento, M. et al. Preterm resuscitation with low oxygen causes less oxidative stress, inflammation, and chronic lung disease. Pediatrics 124, e439–e449 (2009).
Wang, C. L. et al. Resuscitation of preterm neonates by using room air or 100% oxygen. Pediatrics 121, 1083–1089 (2008).
Oei, J. L., et al. Targeted oxygen in the resuscitation of preterm infants, a randomized clinical trial. Pediatrics 139 (2017).
Rabi, Y. et al. Outcomes of preterm infants following the introduction of room air resuscitation. Resuscitation 96, 252–259 (2015).
Chandrasekharan, P., et al. Continuous capnography monitoring during resuscitation in a transitional large mammalian model of asphyxial cardiac arrest. Pediatr Res. 81, 898–904 (2017).
Chandrasekharan, P. K. et al. Continuous end-tidal carbon dioxide monitoring during resuscitation of asphyxiated term lambs. Neonatology 109, 265–273 (2016).
Smolich, J. J., Soust, M., Berger, P. J. & Walker, A. M. Indirect relation between rises in oxygen consumption and left ventricular output at birth in lambs. Circ. Res 71, 443–450 (1992).
Rawat, M. et al. Neonatal resuscitation adhering to oxygen saturation guidelines in asphyxiated lambs with meconium aspiration. Pediatr. Res 79, 583–588 (2016).
Askie, L. M. et al. NeOProM: Neonatal Oxygenation Prospective Meta-analysis Collaboration study protocol. BMC Pediatr. 11, 6 (2011).
Dupont, W. D. & Plummer, W. D. Jr. Power and sample size calculations. A review and computer program. Control Clin. Trials 11, 116–128 (1990).
Lakshminrusimha, S. et al. Pulmonary hemodynamics in neonatal lambs resuscitated with 21%, 50%, and 100% oxygen. Pediatr. Res 62, 313–318 (2007).
Crossley, K. J. et al. Dynamic changes in the direction of blood flow through the ductus arteriosus at birth. J. Physiol. 587, 4695–4704 (2009).
Konduri, G. G. & Kim, U. O. Advances in the diagnosis and management of persistent pulmonary hypertension of the newborn. Pediatr. Clin. North Am. 56, 579–600 (2009). [Epub ahead of print, October 7, 2017].
Lakshminrusimha, S. & Keszler, M. Persistent pulmonary hypertension of the newborn. Neoreviews 16, e680–e692 (2015).
Lang, J. A. et al. Increase in pulmonary blood flow at birth: role of oxygen and lung aeration. J. Physiol. 594, 1389–1398 (2016).
Dawson, J. A. et al. Defining the reference range for oxygen saturation for infants after birth. Pediatrics 125, e1340–e1347 (2010).
Phillipos, E. et al. Oxygen saturation and heart rate ranges in very preterm infants requiring respiratory support at birth. J. Pediatr. 182, 41–46 e42 (2017).
Lakshminrusimha, S., Manja, V., Mathew, B. & Suresh, G. K. Oxygen targeting in preterm infants: a physiological interpretation. J. Perinatol. 35, 8–15 (2015).
Oei, J. L., et al. Outcomes of oxygen saturation targeting during delivery room stabilisation of preterm infants. Arch. Dis. Child Fetal Neonatal Ed. (2017), [Epub ahead of print, October 7, 2017].
Oei J. L., Wright, I. M. & Saugstad, O. D. Authors’ response. Pediatrics 139 (2017).
Vento, M. et al. Resuscitation with room air instead of 100% oxygen prevents oxidative stress in moderately asphyxiated term neonates. Pediatrics 107, 642–647 (2001).
Coalson, J. J., Winter, V. & deLemos, R. A. Decreased alveolarization in baboon survivors with bronchopulmonary dysplasia. Am. J. Respir. Crit. Care Med 152, 640–646 (1995).
Jobe, A. H. & Bancalari, E. Bronchopulmonary dysplasia. Am. J. Respir. Crit. Care Med 163, 1723–1729 (2001).
Warner, B. B., Stuart, L. A., Papes, R. A. & Wispe, J. R. Functional and pathological effects of prolonged hyperoxia in neonatal mice. Am. J. Physiol. 275, L110–L117 (1998).
Lakshminrusimha, S. et al. Pulmonary hemodynamics and vascular reactivity in asphyxiated term lambs resuscitated with 21 and 100% oxygen. J. Appl. Physiol. (1985) 111, 1441–1447 (2011).
Patel, A. et al. Exposure to supplemental oxygen downregulates antioxidant enzymes and increases pulmonary arterial contractility in premature lambs. Neonatology 96, 182–192 (2009).
Castillo, A. et al. Pulse oxygen saturation levels and arterial oxygen tension values in newborns receiving oxygen therapy in the neonatal intensive care unit: is 85% to 93% an acceptable range? Pediatrics 121, 882–889 (2008).
Lakshminrusimha, S. et al. Pulmonary arterial contractility in neonatal lambs increases with 100% oxygen resuscitation. Pediatr. Res 59, 137–141 (2006).
Polglase, G. R. et al. Respiratory support for premature neonates in the delivery room: effects on cardiovascular function and the development of brain injury. Pediatr. Res 75, 682–688 (2014).
Rudolph, A. M. Fetal and neonatal pulmonary circulation. Am. Rev. Respir. Dis. 115, 11–18 (1977).
Kluckow, M. Low systemic blood flow and pathophysiology of the preterm transitional circulation. Early Hum. Dev. 81, 429–437 (2005).
Leahy, F. A., Cates, D., MacCallum, M. & Rigatto, H. Effect of CO2 and 100% O2 on cerebral blood flow in preterm infants. J. Appl. Physiol. Respir. Environ. Exerc Physiol. 48, 468–472 (1980).
Niijima, S., Shortland, D. B., Levene, M. I. & Evans, D. H. Transient hyperoxia and cerebral blood flow velocity in infants born prematurely and at full term. Arch. Dis. Child 63, 1126–1130 (1988).
Thing, M., Sorensen, L. C. & Pryds, O. Transient hyperoxia does not affect regional cerebral tissue oxygen saturation in moderately preterm or term newborns. Acta Paediatr. 104, 657–662 (2015).
Saugstad, O. D. Hyperoxia and cerebral vasoconstriction in healthy newborns. Acta Paediatr. 104, 645–646 (2015).
Gerstner, B. et al. Hyperoxia causes maturation-dependent cell death in the developing white matter. J. Neurosci. 28, 1236–1245 (2008).
Hooper, S. B. et al. The timing of umbilical cord clamping at birth: physiological considerations. Matern Health Neonatol. Perinatol. 2, 4 (2016).
Katheria, A. C., Truong, G., Cousins, L., Oshiro, B. & Finer, N. N. Umbilical cord milking versus delayed cord clamping in preterm infants. Pediatrics 136, 61–69 (2015).
Vali, P., et al. Evaluation of timing and route of epinephrine in a neonatal model of asphyxial arrest. J. Am. Heart Assoc. 6 (2017), [Epub ahead of print, February 18, 2017].
Vali, P. et al. Hemodynamics and gas exchange during chest compressions in neonatal resuscitation. PLoS ONE 12, e0176478 (2017).
Oei, J. L., Saugstad, O. D. & Vento, M. Oxygen and preterm infant resuscitation: what else do we need to know? Curr. Opin. Pediatr. 30 192–198 (2018).
Funding
1R01HD072929 to S.L. and Salary support from University at Buffalo—Dr. Henry C. and Bertha H. Buswell Grant to P.C.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Chandrasekharan, P., Rawat, M., Gugino, S.F. et al. Effect of various inspired oxygen concentrations on pulmonary and systemic hemodynamics and oxygenation during resuscitation in a transitioning preterm model. Pediatr Res 84, 743–750 (2018). https://doi.org/10.1038/s41390-018-0085-x
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-018-0085-x
This article is cited by
-
Cardiorespiratory interactions during the transitional period in extremely preterm infants: a narrative review
Pediatric Research (2025)
-
Preterm infants are not small term infants: Should the resuscitation of a <26-week preterm infant be initiated with 100% oxygen?
Journal of Perinatology (2024)
-
Hemodynamic consequences of respiratory interventions in preterm infants
Journal of Perinatology (2022)
-
Placental transfusion during neonatal resuscitation in an asphyxiated preterm model
Pediatric Research (2022)
-
Stimulating and maintaining spontaneous breathing during transition of preterm infants
Pediatric Research (2021)