Abstract
Background
In sick neonates admitted to the NICU, improper fluid balance can lead to fluid overload. We report the impact of fluid balance in the first postnatal week on outcomes in critically ill near-term/term neonates.
Methods
This analysis includes infants ≥36 weeks gestational age from the Assessment of Worldwide Acute Kidney injury Epidemiology in Neonates (AWAKEN) study (N = 645). Fluid balance: percent weight change from birthweight. Primary outcome: mechanical ventilation (MV) on postnatal day 7.
Results
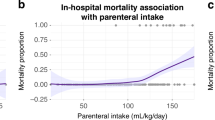
The median peak fluid balance was 1.0% (IQR: −0.5, 4.6) and occurred on postnatal day 3 (IQR: 1, 5). Nine percent required MV at postnatal day 7. Multivariable models showed the peak fluid balance (aOR 1.12, 95%CI 1.08–1.17), lowest fluid balance in 1st postnatal week (aOR 1.14, 95%CI 1.07–1.22), fluid balance on postnatal day 7 (aOR 1.12, 95%CI 1.07–1.17), and negative fluid balance at postnatal day 7 (aOR 0.3, 95%CI 0.16–0.67) were independently associated with MV on postnatal day 7.
Conclusions
We describe the impact of fluid balance in critically ill near-term/term neonates over the first postnatal week. Higher peak fluid balance during the first postnatal week and higher fluid balance on postnatal day 7 were independently associated with MV at postnatal day 7.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Askenazi, D., Griffin, R., McGwin, G., Carlo, W. & Ambalavanan, N. Acute kidney injury is independently associated with mortality in very low birthweight infants: a matched case-control analysis. Pediatr. Nephrol. 24, 991–997 (2009).
Gadepalli, S. K., Selewski, D. T., Drongowski, R. A. & Mychaliska, G. B. Acute kidney injury in congenital diaphragmatic hernia requiring extracorporeal life support: an insidious problem. J. Pediatr. Surg. 46, 630–635 (2011).
Sarkar, S. et al. Relationship between acute kidney injury and brain MRI findings in asphyxiated newborns after therapeutic hypothermia. Pediatr. Res. 75, 431–435 (2014).
Selewski, D. T., Jordan, B. K., Askenazi, D. J., Dechert, R. E. & Sarkar, S. Acute kidney injury in asphyxiated newborns treated with therapeutic hypothermia. J. Pediatr. 162, 725–729 e721 (2013).
Koralkar, R. et al. Acute kidney injury reduces survival in very low birth weight infants. Pediatr. Res. 69, 354–358 (2011).
Zwiers, A. J. et al. Acute kidney injury is a frequent complication in critically ill neonates receiving extracorporeal membrane oxygenation: a 14-year cohort study. Crit. Care. 17, R151 (2013).
Jetton, J. G. et al. Assessment of worldwide acute kidney injury epidemiology in neonates: design of a retrospective cohort study. Front. Pediatr. 4, 68 (2016).
Jetton, J. G. et al. Incidence and outcomes of neonatal acute kidney injury (AWAKEN): a multicentre, multinational, observational cohort study. Lancet Child Adolesc. Health 1, 184–194 (2017).
Arikan, A. A. et al. Fluid overload is associated with impaired oxygenation and morbidity in critically ill children. Pediatr. Crit. Care. Med. 13, 253–258 (2012).
Bhaskar, P., Dhar, A. V., Thompson, M., Quigley, R. & Modem, V. Early fluid accumulation in children with shock and ICU mortality: a matched case-control study. Intensive Care Med. 41, 1445–1453 (2015).
Flori, H. R., Church, G., Liu, K. D., Gildengorin, G. & Matthay, M. A. Positive fluid balance is associated with higher mortality and prolonged mechanical ventilation in pediatric patients with acute lung injury. Crit. Care Res. Pract. 2011, 854142 (2011).
Foland, J. A. et al. Fluid overload before continuous hemofiltration and survival in critically ill children: a retrospective analysis. Crit. Care Med. 32, 1771–1776 (2004).
Goldstein, S. L. et al. Outcome in children receiving continuous venovenous hemofiltration. Pediatrics 107, 1309–1312 (2001).
Goldstein, S. L. et al. Pediatric patients with multi-organ dysfunction syndrome receiving continuous renal replacement therapy. Kidney Int. 67, 653–658 (2005).
Hassinger, A. B., Wald, E. L. & Goodman, D. M. Early postoperative fluid overload precedes acute kidney injury and is associated with higher morbidity in pediatric cardiac surgery patients. Pediatr. Crit. Care. Med. 15, 131–138 (2014).
Hayes, L. W., Oster, R. A., Tofil, N. M. & Tolwani, A. J. Outcomes of critically ill children requiring continuous renal replacement therapy. J. Crit. Care 24, 394–400 (2009).
Hazle, M. A., Gajarski, R. J., Yu, S., Donohue, J. & Blatt, N. B. Fluid overload in infants following congenital heart surgery. Pediatr. Crit. Care. Med. 14, 44–49 (2013).
Schmidt, B. et al. Indomethacin prophylaxis, patent ductus arteriosus, and the risk of bronchopulmonary dysplasia: further analyses from the Trial of Indomethacin Prophylaxis in Preterms (TIPP). J. Pediatr. 148, 730–734 (2006).
Zappitelli, M. et al. Developing a neonatal acute kidney injury research definition: a report from the NIDDK neonatal AKI workshop. Pediatr. Res. 82, 569–573 (2017).
Askenazi, D. J. et al. Fluid overload and mortality are associated with acute kidney injury in sick near-term/term neonate. Pediatr. Nephrol. 28, 661–666 (2013).
Payen, D. et al. A positive fluid balance is associated with a worse outcome in patients with acute renal failure. Crit. Care. 12, R74 (2008).
Seguin, J. et al. Extent, risk factors, and outcome of fluid overload after pediatric heart surgery*. Crit. Care Med. 42, 2591–2599 (2014).
Selewski, D. T. et al. Fluid overload and fluid removal in pediatric patients on extracorporeal membrane oxygenation requiring continuous renal replacement therapy. Crit. Care Med. 40, 2694–2699 (2012).
Selewski, D. T. et al. Weight-based determination of fluid overload status and mortality in pediatric intensive care unit patients requiring continuous renal replacement therapy. Intensive Care Med. 37, 1166–1173 (2011).
Sutherland, S. M. et al. Fluid overload and mortality in children receiving continuous renal replacement therapy: the prospective pediatric continuous renal replacement therapy registry. Am. J. Kidney Dis. 55, 316–325 (2010).
Basu, R. K. et al. Acute kidney injury based on corrected serum creatinine is associated with increased morbidity in children following the arterial switch operation. Pediatr. Crit. Care. Med. 14, e218–e224 (2013).
van Asperen, Y., Brand, P. L. & Bekhof, J. Reliability of the fluid balance in neonates. Acta Paediatr. 101, 479–483 (2012).
Acknowledgements
The authors would also like to thank the outstanding work of the following clinical research personnel and colleagues for their involvement in AWAKEN: Ariana Aimani, Samantha Kronish, Ana Palijan, MD, and Michael Pizzi—Montreal Children’s Hospital, McGill University Health Centre, Montreal, Quebec, Canada. Laila Ajour, BS, Julia Wrona, BS—University of Colorado, Children’s Hospital Colorado, Aurora, Colorado. Melissa Bowman, RN—University of Rochester, Rochester, New York. Teresa Cano, RN, Marta G. Galarza, MD, Wendy Glaberson, MD, Aura Arenas Morales, MD, Denisse Cristina Pareja Valarezo, MD—Holtz Children’s Hospital, University of Miami, Miami, Florida. Sarah Cashman, BS, Madeleine Stead, BS—University of Iowa Children’s Hospital, Iowa City, Iowa. Jonathan Davis, MD, Julie Nicoletta, MD—Floating Hospital for Children at Tufts Medical Center, Tufts University School of Medicine, Boston, Massachusetts. Alanna DeMello—British Columbia Children’s Hospital, Vancouver, British Columbia, Canada. Lynn Dill, RN—University of Alabama at Birmingham, Birmingham, Alabama. Ellen Guthrie, RN—MetroHealth Medical Center, Case Western Reserve University, Cleveland, Ohio. Nicholas L. Harris, BS, Susan M. Hieber, MSQM—C.S. Mott Children’s Hospital, University of Michigan, Ann Arbor, Michigan. Katherine Huang, Rosa Waters—University of Virginia Children’s Hospital, Charlottesville, Virginia. Judd Jacobs, Ryan Knox, BS, Hilary Pitner, MS, Tara Terrell— Cincinnati Children’s Hospital Medical Center, Cincinnati, Ohio. Nilima Jawale, MD—Maimonides Medical Center, Brooklyn, New York. Emily Kane—Australian National University, Canberra, Australia. Vijay Kher, DM, Puneet Sodhi, MBBS—Medanta Kidney Institute, The Medicity Hospital, Gurgaon, Haryana, India. Grace Mele—New York College of Osteopathic Medicine, Westbury, New York. Patricia Mele, DNP—Stony Brook Children’s Hospital, Stony Brook, New York. Charity Njoku, Tennille Paulsen, Sadia Zubair—Texas Children’s Hospital, Baylor College of Medicine, Houston, Texas. Emily Pao—University of Washington, Seattle Children’s Hospital, Seattle, Washington. Becky Selman, RN, Michele Spear, CCRC—University of New Mexico Health Sciences Center Albuquerque, New Mexico. Melissa Vega, PA-C—The Children’s Hospital at Montefiore, Bronx, New York, USA. Leslie Walther, RN—Washington University, St. Louis, Missouri. Funding sources: Cincinnati Children’s Hospital Center for Acute Care Nephrology provided funding to create and maintain the AWAKEN Medidata Rave electronic database. The Pediatric and Infant Center for Acute Nephrology (PICAN) provided support for web meetings, for the NKC steering committee annual meeting at the University of Alabama at Birmingham (UAB), as well as support for some of the AWAKEN investigators at UAB (LJB., R.G.). PICAN is part of the Department of Pediatrics at the University of Alabama at Birmingham (UAB), and is funded by Children’s of Alabama Hospital, the Department of Pediatrics, UAB School of Medicine, and UAB’s Center for Clinical and Translational Sciences (CCTS, NIH grant UL1TR001417). Finally, the AWAKEN study at the University of New Mexico was supported by the Clinical and Translational Science Center (CTSC, NIH grant UL1TR001449) and by the University of Iowa Institute for Clinical and Translational Science (U54TR001356). C.L.A. was supported by the Micah Batchelor Foundation. A.A.A. and C.J.R. were supported by the Section of Pediatric Nephrology, Department of Pediatrics, Texas Children’s Hospital. J.R.C. and J.R.S. were supported by a grant from 100 Women Who Care. F.S.C. and K.T.D. were supported by the Edward Mallinckrodt Department of Pediatrics at Washington University School of Medicine. J.F. and A.K. supported by the Canberra Hospital Private Practice Fund. R.G. and E.R. were supported by the Department of Pediatrics, Golisano Children’s Hospital, University of Rochester. P.E.R. was supported by R01 HL-102497, R01 DK 49419. S.S. and D.T.S. were supported by the Department of Pediatrics & Communicable Disease, C.S. Mott Children’s Hospital, University of Michigan. S.S. and R.W. were supported by Stony Brook Children’s Hospital Department of Pediatrics funding.
AWAKEN investigators
The following individuals served as collaborators and site investigators for the AWAKEN study and are collaborators on this manuscript and should be indexed in PubMed as collaborators on this manuscript (named authors above have been removed from this list): Sunny Juul41, Namasivayam Ambalavanan16, Subrata Sarkar17, Alison Kent18, Jeffery Fletcher18, Carolyn L. Abitbol19, Marissa DeFreitas19, Shahnaz Duara19, Jennifer R. Charlton20, Jonathan R. Swanson20, Carl D’Angio21, Ayesa Mian21, Erin Rademacher21, Maroun J. Mhanna22, Rupesh Raina22, Deepak Kumar22, Jennifer G. Jetton23, Patrick D. Brophy23, Tarah T. Colaizy23, Jonathan M. Klein23, Christopher J. Rhee24, Juan C. Kupferman25, Alok Bhutada25, Shantanu Rastogi25, Susan Ingraham26, F. Sessions Cole27, T. Keefe Davis27, Lawrence Milner28, Alexandra Smith28, Mamta Fuloria29, Frederick J. Kaskel29, Danielle E. Soranno30, Jason Gien30, Aftab S. Chishti31, Sangeeta Hingorani32, Michelle Starr32, Craig S. Wong33, Tara DuPont33, Robin Ohls33, Surender Khokhar34, Sofia Perazzo35, Patricio E. Ray35, Mary Revenis35, Sidharth K. Sethi36, Smriri Rohatgi36, Cherry Mammen37, Anne Synnes37, Sanjay Wazir38, Michael Zappitelli39, Robert Woroniecki40, Shanty Sridhar40
Author information
Authors and Affiliations
Consortia
Contributions
All listed authors provided substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data, drafting the article or revising it critically for and final approval of the version to be published.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Members of the AWAKEN study group are listed at the end of the paper.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Selewski, D.T., Akcan-Arikan, A., Bonachea, E.M. et al. The impact of fluid balance on outcomes in critically ill near-term/term neonates: a report from the AWAKEN study group. Pediatr Res 85, 79–85 (2019). https://doi.org/10.1038/s41390-018-0183-9
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-018-0183-9
This article is cited by
-
Lung ultrasound score and left ventricular eccentricity index in preterm infants with respiratory failure – a pilot study
Journal of Perinatology (2026)
-
Early fluid status and severe intraventricular hemorrhage or death in extremely preterm infants
Pediatric Nephrology (2026)
-
Factors influencing the determination of dosing weight in the neonatal intensive care unit (NICU)
Scientific Reports (2025)
-
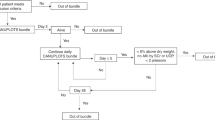
Reducing NICU ventilator days by preventing fluid overload with the CAN-U-P-LOTS standardized bundle
Pediatric Research (2025)
-
Is fluid balance in the first 14 days of life associated with respiratory outcomes in extremely premature neonates? EBM Lesson: Covariate selection in an observation study
Journal of Perinatology (2025)