Abstract
Background
In adults, distal baseline impedance (BI) is a determinant of esophageal mucosal integrity with values <900 Ω indicating inflammation. Relationships between acid gastroesophageal reflux (GER) and BI in neonates are unclear.
Methods
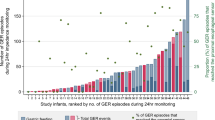
NICU infants (N = 198, 30.4 ± 0.3 weeks gestation) were evaluated at 43 ± 0.4 weeks postmenstrual age using 24-h pH-impedance. Ten randomly selected 1-min windows during rest from the distal impedance channel (Z6) were averaged. Chi-square, t-tests, and ANOVA were used to compare pH-impedance and symptom characteristics by BI severity (BI < 900 Ω, BI 900–2000 Ω, BI > 2000 Ω). Regression analysis was used to identify potential contributing factors of BI.
Results
In BI < 900 Ω: (1) pH-impedance characteristics were increased (acid reflux event frequency, duration, and severity, all P < 0.05 vs. BI > 2000 Ω), and (2) positive symptom correlations were noted with bolus (73%) and acid events (55%). Significant predictors of BI included chronological age, acid reflux index, and BPD diagnosis (all P < 0.05).
Conclusions
Low BI is associated with prolonged acid exposure, delayed clearance, and greater aerodigestive symptom prevalence, likely associated with inflammation and or increased mucosal permeability. BI > 2000 Ω likely involves little or no inflammation because acid exposure is minimal. Combination of SAP, pH-impedance metrics, and BI along with the clarification of dysmotility mechanisms provides the rationale for personalized anti-reflux therapies as needed.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Rosen, R. et al. Pediatric Gastroesophageal Reflux Clinical Practice Guidelines: Joint Recommendations of the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition and the European Society for Pediatric Gastroenterology, Hepatology, and Nutrition. J. Pediatr. Gastroenterol. Nutr. 66, 516–554 (2018).
Vandenplas, Y. et al. Pediatric gastroesophageal reflux clinical practice guidelines: joint recommendations of the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition (NASPGHAN) and the European Society for Pediatric Gastroenterology, Hepatology, and Nutrition (ESPGHAN). J. Pediatr. Gastroenterol. Nutr. 49, 498–547 (2009).
Jadcherla, S. R. et al. Practice variance, prevalence, and economic burden of premature infants diagnosed with GERD. Hosp. Pediatr. 3, 335–341 (2013).
Jadcherla, S. R. et al. Significance of gastroesophageal refluxate in relation to physical, chemical, and spatiotemporal characteristics in symptomatic intensive care unit neonates. Pediatr. Res. 70, 192–198 (2011).
Slaughter, J. L. et al. Neonatal histamine-2 receptor antagonist and proton pump inhibitor treatment at United States Children’s Hospitals. J. Pediatr. 174, 63–70.e63 (2016).
Jadcherla, S. R. et al. Spatiotemporal characteristics of acid refluxate and relationship to symptoms in premature and term infants with chronic lung disease. Am. J. Gastroenterol. 103, 720–728 (2008).
Sivalingam, M. et al. Effects of esophageal acidification on troublesome symptoms: an approach to characterize true acid GERD in dysphagic neonates. Dysphagia 32, 509–519 (2017).
Bredenoord, A. J. et al. Technology review: esophageal impedance monitoring. Am. J. Gastroenterol. 102, 187–194 (2007).
Loots, C. M.et al. Esophageal impedance baselines in infants before and after placebo and proton pump inhibitor therapy. Neurogastroenterol. Motil. 24, 758–762, e351–e352 (2012).
Zhong, C. et al. Esophageal intraluminal baseline impedance is associated with severity of acid reflux and epithelial structural abnormalities in patients with gastroesophageal reflux disease. J. Gastroenterol. 48, 601–610 (2013).
Borrelli, O. et al. Relationship between baseline impedance levels and esophageal mucosal integrity in children with erosive and non-erosive reflux disease. Neurogastroenterol. Motil. 24, 828–e394 (2012).
Cohen Sabban, J. et al. Low-impedance baseline values predict severe esophagitis. J. Pediatr. Gastroenterol. Nutr. 65, 278–280 (2017).
van der Pol, R. J. et al. Outcomes of endoscopy and novel pH-impedance parameters in children: is there a correlation? J. Pediatr. Gastroenterol. Nutr. 56, 196–200 (2013).
Gupta, A. & Jadcherla, S. R. The relationship between somatic growth and in vivo esophageal segmental and sphincteric growth in human neonates. J. Pediatr. Gastroenterol. Nutr. 43, 35–41 (2006).
Ummarino, D. et al. Esophageal impedance baseline according to different time intervals. Eur. J. Med. Res. 17, 18 (2012).
Bredenoord, A. J., Weusten, B. L. & Smout, A. J. Symptom association analysis in ambulatory gastro-oesophageal reflux monitoring. Gut 54, 1810–1817 (2005).
Farre, R. et al. Evaluation of oesophageal mucosa integrity by the intraluminal impedance technique. Gut 60, 885–892 (2011).
Silny, J. Intraluminal multiple electric impedance procedure for measurement of gastrointestinal motility. Wiley Online Libr. 3, 151–162 (1991).
Barlow, J. D., Gregersen, H. & Thompson, D. G. Identification of the biomechanical factors associated with the perception of distension in the human esophagus. Am. J. Physiol. Gastrointest. Liver Physiol. 282, G683–G689 (2002).
Kessing, B. F. et al. Esophageal acid exposure decreases intraluminal baseline impedance levels. Am. J. Gastroenterol. 106, 2093–2097 (2011).
Barlow, W. J. & Orlando, R. C. The pathogenesis of heartburn in nonerosive reflux disease: a unifying hypothesis. Gastroenterology 128, 771–778 (2005).
Salvatore, S. et al. Behind the (impedance) baseline in children. Dis. Esophagus 27, 726–731 (2014).
Slaughter, J. L., Stenger, M. R. & Reagan, P. B. Variation in the use of diuretic therapy for infants with bronchopulmonary dysplasia. Pediatrics 131, 716–723 (2013).
Qureshi, A. et al. The role of sleep in the modulation of gastroesophageal reflux and symptoms in NICU neonates. Pediatr. Neurol. 53, 226–232 (2015).
Sankaran, J. et al. Effect of severity of esophageal acidification on sleep vs wake periods in infants presenting with brief resolved unexplained events. J. Pediatr. 179, 42–48 e41 (2016).
Bhat, R. Y. et al. Acid gastroesophageal reflux in convalescent preterm infants: effect of posture and relationship to apnea. Pediatr. Res. 62, 620–623 (2007).
Jadcherla, S. R. et al. Mechanisms of cough provocation and cough resolution in neonates with bronchopulmonary dysplasia. Pediatr. Res. 78, 462–469 (2015).
Hasenstab, K. A. & Jadcherla, S. R. Respiratory events in infants presenting with apparent life threatening events: is there an explanation from esophageal motility? J. Pediatr. 165, 250–255 e251 (2014).
Ravi, K., et al. Baseline impedance measured during high-resolution esophageal impedance manometry reliably discriminates GERD patients. Neurogastroenterol. Motil. 29, 1–8 e12974 (2017).
Heard, R. et al. Characterization of patients with low baseline impedance on multichannel intraluminal impedance-pH reflux testing. J. Clin. Gastroenterol. 46, e55–e57 (2012).
Jadcherla, S. R. et al. Impact of personalized feeding program in 100 NICU infants: pathophysiology-based approach for better outcomes. J. Pediatr. Gastroenterol. Nutr. 54, 62–70 (2012).
Jadcherla, S. R. et al. Feeding methods at discharge predict long-term feeding and neurodevelopmental outcomes in preterm infants referred for gastrostomy evaluation. J. Pediatr. 181, 125–130 e121 (2017).
Tambucci, R. et al. Clinical relevance of esophageal baseline impedance measurement: just an innocent bystander. J. Pediatr. Gastroenterol. Nutr. 60, 776–782 (2015).
Jadcherla, S. R. Inflammation inhibits muscarinic signaling in in vivo canine colonic circular smooth muscle cells. Pediatr. Res. 52, 756–762 (2002).
Salvatore, S. et al. Esophageal impedance baseline is age dependent. J. Pediatr. Gastroenterol. Nutr. 57, 506–513 (2013).
Salvatore, S. et al. Low mean impedance in 24-hour tracings and esophagitis in children: a strong connection. Dis. Esophagus 29, 10–14 (2016).
Mousa, H. et al. Testing the association between gastroesophageal reflux and apnea in infants. J. Pediatr. Gastroenterol. Nutr. 41, 169–177 (2005).
Salvatore, S. et al. Esophageal impedance in children: symptom-based results. J. Pediatr. 157, 949–954.e1–2 (2010).
Rosen, R. & Nurko, S. The importance of multichannel intraluminal impedance in the evaluation of children with persistent respiratory symptoms. Am. J. Gastroenterol. 99, 2452–2458 (2004).
Rosen, R. et al. The utility of endoscopy and multichannel intraluminal impedance testing in children with cough and wheezing. Pediatr. Pulmonol. 49, 1090–1096 (2014).
Ghezzi, M. et al. Acid and weakly acid gastroesophageal refluxes and type of respiratory symptoms in children. Respir. Med. 105, 972–978 (2011).
Borrelli, O. et al. Role of gastroesophageal reflux in children with unexplained chronic cough. J. Pediatr. Gastroenterol. Nutr. 53, 287–292 (2011).
Francavilla, R. et al. Comparison of esophageal pH and multichannel intraluminal impedance testing in pediatric patients with suspected gastroesophageal reflux. J. Pediatr. Gastroenterol. Nutr. 50, 154–160 (2010).
Corvaglia, L. et al. The frequency of apneas in very preterm infants is increased after non-acid gastro-esophageal reflux. Neurogastroenterol. Motil. 23, 303–307, e152 (2011).
Mattioli, G. et al. Esophageal impedance/pH monitoring in pediatric patients: preliminary experience with 50 cases. Dig. Dis. Sci. 51, 2341–2347 (2006).
ACKNOWLEDGMENTS
We are grateful to Rebecca Moore, BSN RN, for helping with IRB coordination, demographic data extraction, and verification. The study was supported in part by RO1 NIH DK 068158.
Author information
Authors and Affiliations
Contributions
S.R.J. developed the concepts, study design, obtained grant funding and ethical approvals from IRB. S.N. and K.A.H. were also associated with analysis design. N.H. and K.A.H. acquired data and performed analysis. S.N. performed statistical analysis. N.H. created figures. S.R.J., N.H., K.A.H., and S.N. were all involved with data verification, interpretation of results, writing, editing, and approval of final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Jadcherla, S.R., Hanandeh, N., Hasenstab, K.A. et al. Differentiation of esophageal pH-impedance characteristics classified by the mucosal integrity marker in human neonates. Pediatr Res 85, 355–360 (2019). https://doi.org/10.1038/s41390-018-0237-z
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-018-0237-z
This article is cited by
-
Distinct gastroesophageal reflux characteristics in preterm-born infants fed human milk versus formula: insights for clinical practice on outcomes
Journal of Perinatology (2025)
-
Characteristics of esophageal refluxate and symptoms in infants compared between pre-treatment and on treatment with proton pump inhibitors
Journal of Perinatology (2024)
-
Differentiating esophageal sensitivity phenotypes using pH–impedance in intensive care unit infants referred for gastroesophageal reflux symptoms
Pediatric Research (2021)