Abstract
Background
Langerhans cell histiocytosis (LCH) is a histiocytic disorder driven by a constitutive activation of the MAPK signaling pathway in myeloid cells. In 50–60% of cases, it is caused by the BRAFV600E mutation. There is evidence that levels of BRAFV600E in the peripheral blood of patients with LCH correlate with disease burden and could be used as marker for disease extent and response to therapy. However, there is currently no consensus on how testing for minimal disseminated disease should be performed.
Methods
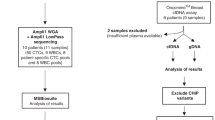
Different approaches to determine the mutation load in patients with LCH were assessed and longitudinal evaluation of patient DNA during treatment with chemotherapy and/or the RAF inhibitor vemurafenib was performed. DNA was isolated from whole blood, different leukocyte subsets, and circulating cell-free DNA (ccf-DNA).
Results
We show that determining BRAF levels from whole blood is superior to using ccfDNA. Furthermore, it is important to identify the clinically relevant BRAF-mutated cellular subpopulations such as CD14+ monocytes or CD1c+ DCs, since other blood cells can also harbor the mutation and therefore confound whole blood or ccfDNA measurements.
Conclusion
Our data support the view that single-agent treatment with an RAF inhibitor reduces disease activity but does not cure LCH.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Haroche, J. et al. Histiocytoses: emerging neoplasia behind inflammation. Lancet Oncol. 18, e113–e125 (2017).
Emile, J. F. et al. Revised classification of histiocytoses and neoplasms of the macrophage-dendritic cell lineages. Blood 127, 2672–2681 (2016).
Gadner, H. et al. Therapy prolongation improves outcome in multisystem Langerhans cell histiocytosis. Blood 121, 5006–5014 (2013).
Badalian-Very, G. et al. Recurrent BRAF mutations in Langerhans cell histiocytosis. Blood 116, 1919–1923 (2010).
Durham, B. H., Diamond, E. L. & Abdel-Wahab, O. Histiocytic neoplasms in the era of personalized genomic medicine. Curr. Opin. Hematol. 23, 416–425 (2016).
Kolenová. A., et al. Targeted inhibition of the MAPK pathway: emerging salvage option for progressive life-threatening multisystem LCH. Blood Adv. 1, 352–356 (2017)
Thierry, A. R. et al. Clinical validation of the detection of KRAS and BRAF mutations from circulating tumor DNA. Nat. Med. 20, 430–435 (2014).
Lopez-Rios, F. et al. Comparison of molecular testing methods for the detection of EGFR mutations in formalin-fixed paraffin-embedded tissue specimens of non-small cell lung cancer. J. Clin. Pathol. 66, 381–385 (2013).
Siravegna G., et al. Integrating liquid biopsies into the management of cancer. Nat. Rev. Clin. Oncol. 14, 531–548 (2017).
Milne P., et al. Hematopoietic origin of Langerhans cell histiocytosis and Erdheim Chester disease in adults. Blood 130, 167–175 (2017).
Heritier, S. et al. BRAF mutation correlates with high-risk langerhans cell histiocytosis and increased resistance to first-line therapy. J. Clin. Oncol. 34, 3023–3030 (2016).
Heritier, S. et al. Circulating cell-free BRAF(V600E) as a biomarker in children with Langerhans cell histiocytosis. Br. J. Haematol. 178, 457–467 (2017).
Janku, F. et al. BRAF V600E mutations in urine and plasma cell-free DNA from patients with Erdheim-Chester disease. Oncotarget 5, 3607–3610 (2014).
Kobayashi, M. & Tojo, A. The BRAF-V600E mutation in circulating cell-free DNA is a promising biomarker of high-risk adult Langerhans cell histiocytosis. Blood 124, 2610–2611 (2014).
Pichler, H. et al. Peripheral blood late mixed chimerism in leucocyte subpopulations following allogeneic stem cell transplantation for childhood malignancies: does it matter? Br. J. Haematol. 173, 905–917 (2016).
Yang, Y. et al. Detection of EGFR and BRAF mutations by competitive allele-specific TaqMan polymerase chain reaction in lung adenocarcinoma. Oncol. Lett. 15, 3295–3304 (2018).
Taylor, S. C., Laperriere, G. & Germain, H. Droplet digital PCR versus qPCR for gene expression analysis with low abundant targets: from variable nonsense to publication quality data. Sci. Rep. 7, 2409 (2017).
Heisig, A. et al. Vemurafenib in Langerhans cell histiocytosis: report of a pediatric patient and review of the literature. Oncotarget 9, 22236–22240 (2018).
Medina Diaz, I. et al. Performance of streck cfDNA blood collection tubes for liquid biopsy testing. PLoS One 11, e0166354 (2016).
Berres, M. L. et al. BRAF-V600E expression in precursor versus differentiated dendritic cells defines clinically distinct LCH risk groups. J. Exp. Med 212, 281 (2015).
Milne P., et al. CD1c+ blood dendritic cells have Langerhans cell potential. Blood 125, 470–473 (2015).
Schwentner R., et al. JAG2 signaling induces differentiation of CD14(+) monocytes into Langerhans cell histiocytosis-like cells. J. Leukoc. Biol. 1–11 (2018).
Allen, C. E., Merad, M. & McClain, K. L. Langerhans-cell histiocytosis. N. Engl. J. Med. 379, 856–868 (2018).
Schwarzenbach, H., Hoon, D. S. & Pantel, K. Cell-free nucleic acids as biomarkers in cancer patients. Nat. Rev. Cancer 11, 426–437 (2011).
Rothwell, D. G. et al. Genetic profiling of tumours using both circulating free DNA and circulating tumour cells isolated from the same preserved whole blood sample. Mol. Oncol. 10, 566–574 (2016).
Swinkels, D. W. et al. Effects of blood-processing protocols on cell-free DNA quantification in plasma. Clin. Chem. 49, 525–526 (2003).
Egeler, R. M. et al. Langerhans cell histiocytosis is a neoplasm and consequently its recurrence is a relapse: In memory of Bob Arceci. Pediatr. Blood Cancer 63, 1704–1712 (2016).
Braier, J. Is Langerhans cell histiocytosis a neoplasia? Pediatr. Blood Cancer 64, e26267 (2017).
Acknowledgments
The authors thank Dieter Printz, Julia Stemberger, Angela Schumich, and Elke Zipperer for flow cytometry analysis and cell sorting, and Oskar Haas, Karin Nebral, and Margit König for FISH analysis. This work was supported by a Clinical Investigator-driven grant from the St Anna Kinderkrebsforschung and the Histiozytosehilfe e.V.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Schwentner, R., Kolenová, A., Jug, G. et al. Longitudinal assessment of peripheral blood BRAFV600E levels in patients with Langerhans cell histiocytosis. Pediatr Res 85, 856–864 (2019). https://doi.org/10.1038/s41390-018-0238-y
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-018-0238-y
This article is cited by
-
Disease response criteria in Langerhans cell histiocytosis: a global view
International Journal of Hematology (2025)
-
Current State of Targeted Therapy in Adult Langerhans Cell Histiocytosis and Erdheim–Chester Disease
Targeted Oncology (2024)
-
Optimal timing of liver transplantation for liver cirrhosis caused by sclerosing cholangitis in a patient with Langerhans cell histiocytosis: a case report
International Journal of Hematology (2023)
-
Detection of BRAF V600E mutation in radiological Langerhans cell histiocytosis-associated neurodegenerative disease using droplet digital PCR analysis
International Journal of Hematology (2023)
-
The coming of age of Langerhans cell histiocytosis
Nature Immunology (2020)