Abstract
Background
Maternal smoking impairs fetal growth; however, if postnatal growth differs between children born small for gestational age (SGA) with smoking and non-smoking mother is unknown.
Methods
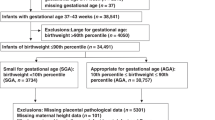
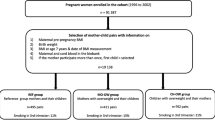
Cohort-study of term born children born appropriate for gestational age with non-smoking mother (AGA-NS, n = 30,561), SGA (birthweight <10th percentile) with smoking mother (SGA-S, n = 171) or SGA with non-smoking mother (SGA-NS, n = 1761). Means of height and weight measurements, collected at birth, 1.5, 3, 4, and 5 years, were compared using a generalized linear mixed effect model. Relative risks of short stature (<10th percentile) were expressed as adjusted risk ratios (aRR).
Results
At birth, children born SGA-S were shorter than SGA-NS, but they did not differ in weight. At 1.5 years, SGA-S had reached the same height as SGA-NS. At 5 years, SGA-S were 1.1 cm taller and 1.2 kg heavier than SGA-NS. Compared with AGA-NS, SGA-S did not have increased risk of short stature at 1.5 or 5 years, while SGA-NS had increased risk of short stature at both ages; aRRs 3.0 (95% CI 2.6;3.4) and 2.3 (95% CI 2.0;2.7), respectively.
Conclusions
Children born SGA-S have a more rapid catch-up growth than SGA-NS. This may have consequences for metabolic and cardiovascular health in children with smoking mothers.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Ahlsten, G., Cnattingius, S. & Lindmark, G. Cessation of smoking during pregnancy improves foetal growth and reduces infant morbidity in the neonatal period. A population-based prospective study. Acta Paediatr. 82, 177–181 (1993).
Vik, T., Jacobsen, G., Vatten, L. & Bakketeig, L. S. Pre- and post-natal growth in children of women who smoked in pregnancy. Early Hum. Dev. 45, 245–255 (1996).
Rogers, J. M. Tobacco and pregnancy. Reprod. Toxicol. 28, 152–160 (2009).
Sabra, S., Gratacos, E. & Gomez Roig, M. D. Smoking-induced changes in the maternal immune, endocrine, and metabolic pathways and their impact on fetal growth: a topical review. Fetal Diagn. Ther. 41, 241–250 (2017).
Wit, J. M. & Boersma, B. Catch-up growth: definition, mechanisms, and models. J. Pediatr. Endocrinol. Metab. 15(Suppl 5), 1229–1241 (2002).
Finkielstain, G. P., Lui, J. C. & Baron, J. Catch-up growth: cellular and molecular mechanisms. World Rev. Nutr. Diet. 106, 100–104 (2013).
Hokken-Koelega, A. C. S. et al. Children born small for gestational age: do they catch up[quest]. Pediatr. Res 38, 267–271 (1995).
Karlberg, J. & Albertsson-Wikland, K. Growth in full-term small-for-gestational-age infants: from birth to final height. Pediatr. Res. 38, 733–739 (1995).
Eriksson, J. G., Forsen, T., Tuomilehto, J., Osmond, C. & Barker, D. J. Early growth and coronary heart disease in later life: longitudinal study. BMJ 322, 949–953 (2001).
Ong, K. K., Ahmed, M. L., Emmett, P. M., Preece, M. A. & Dunger, D. B. Association between postnatal catch-up growth and obesity in childhood: prospective cohort study. BMJ 320, 967–971 (2000).
Castanys-Munoz, E. et al. Systematic review indicates postnatal growth in term infants born small-for-gestational-age being associated with later neurocognitive and metabolic outcomes. Acta Paediatr. 106, 1230–1238 (2017).
Soto, N. et al. Insulin sensitivity and secretion are related to catch-up growth in small-for-gestational-age infants at age 1 year: results from a prospective cohort. J. Clin. Endocrinol. Metab. 88, 3645–3650 (2003).
Aris, I. M. et al. Infant body mass index peak and early childhood cardio-metabolic risk markers in a multi-ethnic Asian birth cohort. Int J. Epidemiol. 46, 513–525 (2017).
Chen, L. W. et al. Associations of maternal macronutrient intake during pregnancy with infant BMI peak characteristics and childhood BMI. Am. J. Clin. Nutr. 105, 705–713 (2017).
Eny, K. M. et al. Breastfeeding duration, maternal body mass index, and birth weight are associated with differences in body mass index growth trajectories in early childhood. Am. J. Clin. Nutr. 107, 584–592 (2018).
Bell, S. et al. Duration of breastfeeding, but not timing of solid food, reduces the risk of overweight and obesity in children aged 24 to 36 months: findings from an Australian cohort study. Int J. Environ. Res Public Health 15, E599 (2018).
Kramer, M. S. et al. Infant feeding and growth: putting the horse before the cart. Am. J. Clin. Nutr. 107, 635–639 (2018).
Vielwerth, S. E., Jensen, R. B., Larsen, T. & Greisen, G. The impact of maternal smoking on fetal and infant growth. Early Hum. Dev. 83, 491–495 (2007).
Ong, K. K., Preece, M. A., Emmett, P. M., Ahmed, M. L. & Dunger, D. B. Size at birth and early childhood growth in relation to maternal smoking, parity and infant breast-feeding: longitudinal birth cohort study and analysis. Pediatr. Res. 52, 863–867 (2002).
Day, N. L., Richardson, G. A., Geva, D. & Robles, N. Alcohol, marijuana, and tobacco: effects of prenatal exposure on offspring growth and morphology at age six. Alcohol Clin. Exp. Res. 18, 786–794 (1994).
Fenercioglu, A. K., Tamer, I., Karatekin, G. & Nuhoglu, A. Impaired postnatal growth of infants prenatally exposed to cigarette smoking. Tohoku J. Exp. Med. 218, 221–228 (2009).
Rantakallio, P. A follow-up study up to the age of 14 of children whose mothers smoked during pregnancy. Acta Paediatr. Scand. 72, 747–753 (1983).
Niklasson, A. et al. An update of the Swedish reference standards for weight, length and head circumference at birth for given gestational age (1977–1981). Acta Paediatr. Scand. 80, 756–762 (1991).
Wikland, K. A., Luo, Z. C., Niklasson, A. & Karlberg, J. Swedish population-based longitudinal reference values from birth to 18 years of age for height, weight and head circumference. Acta Paediatr. 91, 739–754 (2002).
Cnattingius, S., Ericson, A., Gunnarskog, J. & Kallen, B. A quality study of a medical birth registry. Scand. J. Soc. Med. 18, 143–148 (1990).
George, L., Granath, F., Johansson, A. L. & Cnattingius, S. Self-reported nicotine exposure and plasma levels of cotinine in early and late pregnancy. Acta Obstet. Gynecol. Scand. 85, 1331–1337 (2006).
Wallby, T. & Hjern, A. Child health care uptake among low-income and immigrant families in a Swedish county. Acta Paediatr. 100, 1495–1503 (2011).
Griffiths, L. J., Dezateux, C. & Cole, T. J. Differential parental weight and height contributions to offspring birthweight and weight gain in infancy. Int J. Epidemiol. 36, 104–107 (2007).
Naeye, R. L. Influence of maternal cigarette smoking during pregnancy on fetal and childhood growth. Obstet. Gynecol. 57, 18–21 (1981).
Koch, S., Vilser, C., Gross, W. & Schleussner, E. Smoking during pregnancy: risk for intrauterine growth retardation and persisting microsomia. Z. Geburtshilfe Neonatol. 216, 77–81 (2012).
Chrestani, M. A., Santos, I. S., Horta, B. L., Dumith, S. C. & de Oliveira Dode, M. A. Associated factors for accelerated growth in childhood: a systematic review. Matern Child Health J. 17, 512–519 (2013).
Zheng, W. et al. Maternal smoking during pregnancy and growth in infancy: a covariance structure analysis. J. Epidemiol. 25, 44–49 (2015).
Nafstad, P. et al. Weight gain during the first year of life in relation to maternal smoking and breast feeding in Norway. J. Epidemiol. Community Health 51, 261–265 (1997).
Horta, B. L., Kramer, M. S. & Platt, R. W. Maternal smoking and the risk of early weaning: a meta-analysis. Am. J. Public Health 91, 304–307 (2001).
Sebastiani, G. et al. The sequence of prenatal growth restraint and post-natal catch-up growth leads to a thicker intima-media and more pre-peritoneal and hepatic fat by age 3–6 years. Pediatr. Obes. 11, 251–257 (2016).
Leunissen, R. W., Kerkhof, G. F., Stijnen, T. & Hokken-Koelega, A. C. Effect of birth size and catch-up growth on adult blood pressure and carotid intima-media thickness. Horm. Res Paediatr. 77, 394–401 (2012).
Skilton, M. R. et al. Weight gain in infancy and vascular risk factors in later childhood. Pediatrics 131, e1821–e1828 (2013).
Cianfarani, S., Ladaki, C. & Geremia, C. Hormonal regulation of postnatal growth in children born small for gestational age. Horm. Res 65(Suppl 3), 70–74 (2006).
Author information
Authors and Affiliations
Contributions
Study concept and design: L.L, A.-K.W, E.B, A.M-L, F.A. and M.L. Acquisition of data: L.L and U.H. Analysis and interpretation of data: L.L, A.-K.W. and M.L. Statistical analysis, first draft, and revision of the manuscript: L.L. Critical revision of the manuscript for important intellectual content: L.L., A.-K.W., E.B, A.M.-L., U.H., F.A., M.L.
Corresponding author
Ethics declarations
Funding:
The project was funded by the Gillbergska foundation and Födelsefonden (LL). A.-K.W. is supported by the Swedish Research Council (grant 2014–3561). F.A. is supported by the Gillbergska foundation and HRH Crown Princess Lovisas association for pediatric care.
Competing interests:
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Lindström, L., Wikström, AK., Bergman, E. et al. Postnatal growth in children born small for gestational age with and without smoking mother. Pediatr Res 85, 961–966 (2019). https://doi.org/10.1038/s41390-019-0352-5
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-019-0352-5