Abstract
Background
Cardiorespiratory stability of preterm infants is a prerequisite for discharge from the neonatal intensive care unit (NICU) but very difficult to predict. We aimed to assess whether characterizing heart rate fluctuation (HRF) within the first days of life has prognostic utility.
Methods
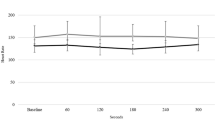
We conducted a prospective cohort study in 90 preterm infants using a previously validated surface diaphragmatic electromyography (sEMG) method to derive interbeat intervals. We characterized HRF by time series parameters including sample entropy (SampEn) and scaling exponent alpha (ScalExp) obtained from daily 3-h measurements. Data were analyzed by multivariable, multilevel linear regression.
Results
We obtained acceptable raw data from 309/330 sEMG measurements in 76/90 infants born at a mean (range) of 30.2 (24.7–34.0) weeks gestation. We found a significant negative association of SampEn with duration of respiratory support (R2 = 0.53, p < 0.001) and corrected age at discontinuation of caffeine therapy (R2 = 0.35, p < 0.001) after adjusting for sex, gestational age, birth weight z-score, and sepsis.
Conclusions
Baseline SampEn calculated over the first 5 days of life carries prognostic utility for an estimation of subsequent respiratory support and pre-discharge cardiorespiratory stability in preterm infants, both important for planning of treatment and utilization of health care resources.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
American Academy of Pediatrics. Task Force on Prolonged Infantile Apnea. Prolonged infantile apnea: 1985. Pediatrics 76, 129–131 (1985).
Henderson-Smart, D. J. & De Paoli, A. G. Methylxanthine treatment for apnoea in preterm infants. Cochrane Database Syst. Rev. CD000140 (2010).
Poets, C. F. et al. Association between intermittent hypoxemia or bradycardia and late death or disability in extremely preterm infants. JAMA 314, 595–603 (2015).
Lemyre, B., Davis, P. G. & de Paoli, A. G. Nasal intermittent positive pressure ventilation (NIPPV) versus nasal continuous positive airway pressure (NCPAP) for apnea of prematurity. Cochrane Database Syst. Rev. CD002272 (2002).
Schmidt B., et al. Caffeine therapy for apnea of prematurity. N. Engl. J. Med. 354, 2112–2121 (2006).
Zupancic, J. A., Richardson, D. K., O’Brien, B. J., Eichenwald, E. C. & Weinstein, M. C. Cost-effectiveness analysis of predischarge monitoring for apnea of prematurity. Pediatrics 111, 146–152 (2003).
Eichenwald, E. C. et al. Variation in diagnosis of apnea in moderately preterm infants predicts length of stay. Pediatrics 127, e53–e58 (2011).
Poets, C. F. Apnea of prematurity: what can observational studies tell us about pathophysiology? Sleep Med. 11, 701–707 (2010).
Jardine, L. A., Inglis, G. D. & Davies, M. W. Strategies for the withdrawal of nasal continuous positive airway pressure (NCPAP) in preterm infants. Cochrane Database Syst. Rev. CD006979 (2011).
Eichenwald, E. C. & Committee on Fetus and Newborn Apnea of Prematurity. Pediatrics 137, e20153757 (2016).
Fyfe, K. L. et al. The effect of gestational age at birth on post-term maturation of heart rate variability. Sleep 38, 1635–1644 (2015).
Griffin, M. P., Lake, D. E., O’Shea, T. M. & Moorman, J. R. Heart rate characteristics and clinical signs in neonatal sepsis. Pediatr. Res. 61, 222–227 (2007).
Sullivan, B. A. et al. Early heart rate characteristics predict death and morbidities in preterm infants. J. Pediatr. 174, 57–62 (2016).
Lake, D. E., Richman, J. S., Griffin, M. P. & Moorman, J. R. Sample entropy analysis of neonatal heart rate variability. Am. J. Physiol. Regul. Integr. Comp. Physiol. 283, R789–R797 (2002).
Peng, C. K. et al. Fractal mechanisms and heart rate dynamics. Long-range correlations and their breakdown with disease. J. Electrocardiol. 28, 59–65 (1995). Suppl.
Peng, C. K., Havlin, S., Stanley, H. E. & Goldberger, A. L. Quantification of scaling exponents and crossover phenomena in nonstationary heartbeat time series. Chaos 5, 82–87 (1995).
Jost, K. et al. Surface electromyography for analysis of heart rate variability in preterm infants. Physiol. Meas. 39, 015004 (2017).
Kraaijenga, J. V., Hutten, G. J., de Jongh, F. H. & van Kaam, A. H. Transcutaneous electromyography of the diaphragm: a cardio-respiratory monitor for preterm infants. Pedia. Pulmonol. 50, 889–895 (2015).
Berry, R. B. Fundamentals of Sleep Medicine (Elsevier/Saunders, Philadelphia, 2012).
Mirmiran, M., Maas, Y. G. & Ariagno, R. L. Development of fetal and neonatal sleep and circadian rhythms. Sleep Med. Rev. 7, 321–334 (2003).
Cremer, M. et al. Immediate effects of phototherapy on sleep in very preterm neonates: an observational study. J. Sleep. Res. 25, 517–523 (2016).
Heart rate variability: standards of measurement, physiological interpretation and clinical use. Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Circulation 93, 1043–1065 (1996).
Kleiger, R. E., Stein, P. K. & Bigger, J. T. Jr. Heart rate variability: measurement and clinical utility. Ann. Noninvasive Electrocardiol. 10, 88–101 (2005).
Richman, J. S. & Moorman, J. R. Physiological time-series analysis using approximate entropy and sample entropy. Am. J. Physiol. Heart Circ. Physiol. 278, H2039–H2049 (2000).
Nakamura, T., Horio, H., Miyashita, S., Chiba, Y. & Sato, S. Identification of development and autonomic nerve activity from heart rate variability in preterm infants. Biosystems 79, 117–124 (2005).
Yum, M. K., Park, E. Y., Kim, C. R. & Hwang, J. H. Alterations in irregular and fractal heart rate behavior in growth restricted fetuses. Eur. J. Obstet. Gynecol. Reprod. Biol. 94, 51–58 (2001).
Bell, R. S. Neonatal necrotizing enterocolitis. N. Engl. J. Med. 283, 153–154 (1970).
Papile, L. A., Burstein, J., Burstein, R. & Koffler, H. Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1,500 gm. J. Pediatr. 92, 529–534 (1978).
Cohen, J. Power Analysis for the Behavioral Sciences (Academic Press, New York, 1988).
Cohen, J., Cohen, P., West, S. & Aiken, L. Applied Multiple Regression/Correlation Analysis for the Behavioral Sciences (Lawrence Erlbaum Associates, Mahwah, NJ, 2003).
Casolo, G. C. et al. Heart rate variability during the acute phase of myocardial infarction. Circulation 85, 2073–2079 (1992).
Singh, N., Mironov, D., Armstrong, P. W., Ross, A. M. & Langer, A. Heart rate variability assessment early after acute myocardial infarction. Pathophysiological and prognostic correlates. GUSTO ECG Substudy Investigators. Global Utilization of Streptokinase and TPA for Occluded Arteries. Circulation 93, 1388–1395 (1996).
Griffin, M. P., Lake, D. E. & Moorman, J. R. Heart rate characteristics and laboratory tests in neonatal sepsis. Pediatrics 115, 937–941 (2005).
Moorman, J. R. et al. Cardiovascular oscillations at the bedside: early diagnosis of neonatal sepsis using heart rate characteristics monitoring. Physiol. Meas. 32, 1821–1832 (2011).
Moorman, J. R. et al. Mortality reduction by heart rate characteristic monitoring in very low birth weight neonates: a randomized trial. J. Pediatr. 159, 900–906 e901 (2011).
Goulding, R. M. et al. Heart rate variability in hypoxic ischemic encephalopathy: correlation with EEG grade and 2-y neurodevelopmental outcome. Pediatr. Res. 77, 681–687 (2015).
Fairchild, K. D. et al. Abnormal heart rate characteristics are associated with abnormal neuroimaging and outcomes in extremely low birth weight infants. J. Perinatol. 34, 375–379 (2014).
Kemper, K. J., Hamilton, C. & Atkinson, M. Heart rate variability: impact of differences in outlier identification and management strategies on common measures in three clinical populations. Pediatr. Res. 62, 337–342 (2007).
Schechtman, V. L., Kluge, K. A. & Harper, R. M. Time-domain system for assessing variation in heart rate. Med Biol. Eng. Comput. 26, 367–373 (1988).
Vanoli, E. et al. Heart rate variability during specific sleep stages. A comparison of healthy subjects with patients after myocardial infarction. Circulation 91, 1918–1922 (1995).
Acknowledgements
We thank research nurses K. Gerber, A. Imolesi, A. Padiyath, M. Weber, and N. Wellauer (all affiliated to University Children’s Hospital Basel, Basel, Switzerland) for their help in data acquisition and medical students M. Cremer, A. Gensmer, K. Ledergerber, R. Marchetti, N. Schoenfeld, and N. Schwob (all affiliated to University Children’s Hospital Basel, Basel, Switzerland) for their assistance in video analysis. This study was supported by the Swiss National Science Foundation (No. 141206). The funding body had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
K.J.: Substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; drafting the article; and final approval of the version to be published. A.N.D.: Substantial contributions to conception and design, and interpretation of data; revising the article critically for important intellectual content; and final approval of the version to be published. U.P.F. and B.S.: Substantial contributions to conception and design, analysis and interpretation of data; revising the article critically for important intellectual content; and final approval of the version to be published. S.M.S.: Substantial contributions to conception and design, acquisition of data, analysis and interpretation of data; revising the article critically for important intellectual content; and final approval of the version to be published.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Jost, K., Datta, A.N., Frey, U.P. et al. Heart rate fluctuation after birth predicts subsequent cardiorespiratory stability in preterm infants. Pediatr Res 86, 348–354 (2019). https://doi.org/10.1038/s41390-019-0424-6
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-019-0424-6
This article is cited by
-
Sample entropy of oxygen saturation in preterm infants
Scientific Reports (2025)
-
Future perspectives of heart rate and oxygenation monitoring in the neonatal intensive care unit – a narrative review
Journal of Clinical Monitoring and Computing (2025)
-
Sample entropy correlates with intraventricular hemorrhage and mortality in premature infants early in life
Pediatric Research (2024)
-
Novel approaches to capturing and using continuous cardiorespiratory physiological data in hospitalized children
Pediatric Research (2023)
-
The rhythm of a preterm neonate’s life: ultradian oscillations of heart rate, body temperature and sleep cycles
Journal of Pharmacokinetics and Pharmacodynamics (2021)