Abstract
Background
Fetal concentrations of GFAP and UCH-L1 are elevated in umbilical arterial (UmA) blood of neonates with birth asphyxia plus neonatal encephalopathy (NE), but their source and role of placental clearance/synthesis is unknown.
Methods
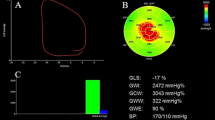
Prospective cohort study of term neonates to (a) determine UmA and venous (UmV) blood concentrations of GFAP and UCH-L1 in term uncomplicated pregnancies and their placental synthesis and/or clearance and (b) compare UmA concentrations in uncomplicated pregnancies with those complicated by fetal hypoxia–asphyxia+NE. Three term groups were studied: uncomplicated cesarean delivery without labor (Group 1, n = 15), uncomplicated vaginal delivery with labor (Group 2, n = 15), and perinatal hypoxia–asphyxia+NE (Group 3, n = 8).
Results
UmA GFAP concentrations were lower in Group 1 vs. 2 (P = 0.02) and both demonstrated 100% placental clearance. In contrast, UmA and UmV UCH-L1 concentrations were not unaffected by labor. Group 3 UmA GFAP concentrations were 30- and 8-fold higher than Groups 1 and 2, respectively, P = 0.02, whereas UmA UCH-L1 concentrations were similar in all groups.
Conclusions
UmA GFAP is derived from the fetus, and circulating levels, which are modulated by placental clearance, increase during uncomplicated labor and more so in the presence of fetal hypoxia–asphyxia+NE, providing a better biomarker than UCH-L1 for hypoxia–asphyxia+NE.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Kurinczuk, J. J., White-Koning, M. & Badawi, N. Epidemiology of neonatal encephalopathy and hypoxic-ischaemic encephalopathy. Early Hum. Dev. 86, 329–338 (2010).
Shankaran, S., Woldt, E., Koepke, T., Bedard, M. P. & Nandyal, R. Acute neonatal morbidity and long-term central nervous system sequelae of perinatal asphyxia in term infants. Early Hum. Dev. 25, 135–148 (1991).
Volpe, J. J. Neonatal encephalopathy: an inadequate term for hypoxic-ischemic encephalopathy. Ann. Neurol. 72, 156–166 (2012).
de Vries, L. S. & Jongmans, M. J. Long-term outcome after neonatal hypoxic-ischaemic encephalopathy. Arch. Dis. Child Fetal Neonatal Ed. 95, F220–F224 (2010).
Marlow, N., Rose, A. S., Rands, C. E. & Draper, E. S. Neuropsychological and educational problems at school age associated with neonatal encephalopathy. Arch. Dis. Child Fetal Neonatal Ed. 90, F380–F387 (2005).
Gonzalez, F. F. & Miller, S. P. Does perinatal asphyxia impair cognitive function without cerebral palsy? Arch. Dis. Child Fetal Neonatal Ed. 91, F454–F459 (2006).
Finer, N. N., Robertson, C. M., Richards, R. T., Pinnell, L. E. & Peters, K. L. Hypoxic-ischemic encephalopathy in term neonates: perinatal factors and outcome. J. Pediatr. 98, 112–117 (1981).
Sarnat, H. B. & Sarnat, M. S. Neonatal encephalopathy following fetal distress. A clinical and electroencephalographic study. Arch. Neurol. 33, 696–705 (1976).
Eng, L. F., Ghirnikar, R. S. & Lee, Y. L. Glial fibrillary acidic protein: GFAP-thirty-one years (1969-2000). Neurochem. Res. 25, 1439–1451 (2000).
Thompson, R. J., Doran, J. F., Jackson, P., Dhillon, A. P. & Rode, J. PGP 9.5--a new marker for vertebrate neurons and neuroendocrine cells. Brain Res. 278, 224–228 (1983).
Day, I. N. & Thompson, R. J. UCHL1 (PGP 9.5): neuronal biomarker and ubiquitin system protein. Prog. Neurobiol. 90, 327–362 (2010).
Douglas-Escobar, M. et al. A pilot study of novel biomarkers in neonates with hypoxic-ischemic encephalopathy. Pediatr. Res. 68, 531–536 (2010).
Ennen, C. S. et al. Glial fibrillary acidic protein as a biomarker for neonatal hypoxic-ischemic encephalopathy treated with whole-body cooling. Am. J. Obstet. Gynecol. 205, 251 e1-7 (2011).
Massaro, A. N. et al. Serum biomarkers of MRI brain injury in neonatal hypoxic ischemic encephalopathy treated with whole-body hypothermia: a pilot study. Pediatr. Crit. Care Med. 14, 310–317 (2013).
Chalak, L. F. et al. Biomarkers for severity of neonatal hypoxic-ischemic encephalopathy and outcomes in newborns receiving hypothermia therapy. J. Pediatr. 164, 468–474 e1 (2014).
Mir, I. N. & Chalak, L. F. Serum biomarkers to evaluate the integrity of the neurovascular unit. Early Hum. Dev. 90, 707–711 (2014).
Douglas-Escobar, M. V. et al. UCH-L1 and GFAP serum levels in neonates with hypoxic-ischemic encephalopathy: a single center pilot study. Front. Neurol. 5, 273 (2014).
Jiang, S. H., Wang, J. X., Zhang, Y. M. & Jiang, H. F. Effect of hypothermia therapy on serum GFAP and UCH-L1 levels in neonates with hypoxic-ischemic encephalopathy. Zhongguo Dang Dai Er Ke Za Zhi 16, 1193–1196 (2014).
Zaigham, M., Lundberg, F., Hayes, R., Unden, J. & Olofsson, P. Umbilical cord blood concentrations of ubiquitin carboxy-terminal hydrolase L1 (UCH-L1) and glial fibrillary acidic protein (GFAP) in neonates developing hypoxic-ischemic encephalopathy. J. Matern. Fetal Neonatal Med. 29, 1822–1828 (2016).
Sekiguchi, S. et al. Immunohistochemical analysis of protein gene product 9.5, a ubiquitin carboxyl-terminal hydrolase, during placental and embryonic development in the mouse. Exp. Anim. 52, 365–369 (2003).
Sekiguchi, S. et al. Localization of ubiquitin carboxyl-terminal hydrolase-L1 in cynomolgus monkey placentas. Placenta 26, 99–103 (2005).
Shankaran, S. et al. Whole-body hypothermia for neonates with hypoxic-ischemic encephalopathy. N. Engl. J. Med. 353, 1574–1584 (2005).
Barbera, A. et al. Relationship of umbilical vein blood flow to growth parameters in the human fetus. Am. J. Obstet. Gynecol. 181, 174–179 (1999).
Kunzel, W., Jovanovic, V. & Grussner, S. Blood flow in the umbilical vein and artery in pregnancy. Geburtshilfe Frauenheilkd. 51, 513–522 (1991).
Link, G., Clark, K. E. & Lang, U. Umbilical blood flow during pregnancy: evidence for decreasing placental perfusion. Am. J. Obstet. Gynecol. 196, 489 e1-7 (2007).
Ioannidis, J. P. A. & Bossuyt, P. M. M. Waste, leaks, and failures in the biomarker pipeline. Clin. Chem. 63, 963–972 (2017).
Mir, I. N. et al. Fetal-placental crosstalk occurs through fetal cytokine synthesis and placental clearance. Placenta 69, 1–8 (2018).
Zaretsky, M. V., Alexander, J. M., Byrd, W. & Bawdon, R. E. Transfer of inflammatory cytokines across the placenta. Obstet. Gynecol. 103, 546–550 (2004).
Dahlgren, J., Samuelsson, A. M., Jansson, T. & Holmang, A. Interleukin-6 in the maternal circulation reaches the rat fetus in mid-gestation. Pediatr. Res. 60, 147–151 (2006).
Rosenfeld, C. R., Gresores, A., Roy, T. A. & Magness, R. R. Comparison of ANG II in fetal and pregnant sheep: metabolic clearance and vascular sensitivity. Am. J. Physiol. 268, E237–E247 (1995).
Johnson, A. R., Skidgel, R. A., Gafford, J. T. & Erdos, E. G. Enzymes in placental microvilli: angiotensin I converting enzyme, angiotensinase A, carboxypeptidase, and neutral endopeptidase (“enkephalinase”). Peptides 5, 789–796 (1984).
Schofield, J. N., Day, I. N., Thompson, R. J. & Edwards, Y. H. PGP9.5, a ubiquitin C-terminal hydrolase; pattern of mRNA and protein expression during neural development in the mouse. Brain Res. Dev. Brain Res. 85, 229–238 (1995).
Kent, C. & Clarke, P. J. The immunolocalisation of the neuroendocrine specific protein PGP9.5 during neurogenesis in the rat. Brain Res. Dev. Brain Res. 58, 147–150 (1991).
Wilson, P. O. et al. The immunolocalization of protein gene product 9.5 using rabbit polyclonal and mouse monoclonal antibodies. Br. J. Exp. Pathol. 69, 91–104 (1988).
Wilkinson, K. D. et al. The neuron-specific protein PGP 9.5 is a ubiquitin carboxyl-terminal hydrolase. Science 246, 670–673 (1989).
Kon, Y., Endoh, D. & Iwanaga, T. Expression of protein gene product 9.5, a neuronal ubiquitin C-terminal hydrolase, and its developing change in sertoli cells of mouse testis. Mol. Reprod. Dev. 54, 333–341 (1999).
Kwon, J. et al. Characterization of the testis in congenitally ubiquitin carboxy-terminal hydrolase-1 (Uch-L1) defective (gad) mice. Exp. Anim. 52, 1–9 (2003).
Acknowledgements
This work was supported by an NIH grant R01NS102617-01 awarded to L.F.C.
Author information
Authors and Affiliations
Contributions
All authors contributed to drafting the article or revising it critically for important intellectual content and final approval of the submitted version. Specifically, I.N.M. participated in concept, study design, sample and data acquisition and interpretation, performed the statistical analysis and drafted the first version of the manuscript, and finalized the manuscript for submission after comments from the other authors. L.S.B. performed the statistical analysis, participated in data interpretation and review, revision of the manuscript, and reviewed the final version. C.R.R. and L.F.C. participated in concept, study design, data interpretation and review, revision of the manuscript, and participated in finalizing the manuscript after comments from the other authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mir, I.N., Steven Brown, L., Rosenfeld, C.R. et al. Placental clearance/synthesis of neurobiomarkers GFAP and UCH-L1 in healthy term neonates and those with moderate–severe neonatal encephalopathy. Pediatr Res 86, 500–504 (2019). https://doi.org/10.1038/s41390-019-0439-z
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-019-0439-z