Abstract
Background
Asphyxia of newborns is a severe and frequent challenge of the peri- and postnatal period.
Methods
Forty-four neonatal piglets underwent asphyxia and hemorrhage (AH), followed by resuscitation with blood or crystalloid transfusion. In this study, 15 piglets (blood n = 9, NaCl n = 6, mean age 31 h) were randomly chosen. Four hours after return of spontaneous circulation, heart tissue and blood were collected. Analyses of heart fatty acid binding protein (HFABP), cardiac troponin I (TnI) levels, and activation of the complement system were performed. Histological staining for connexin 43 (Cx43) and complement C5a receptor 1 (C5aR1) was performed.
Results
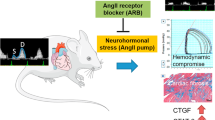
Following AH, systemic elevation of cardiac TnI and HFABP revealed cardiac damage in both groups. Systemic activation of the complement system and the appearance of extracellular histones in plasma of the blood transfusion group were observed. The Cx43 was translocated from the intercalated discs to the cytosol after AH. Cardiac glycogen concentration was reduced in both groups. A significant reduction of C5aR1 in the left ventricle and a significant elevation of the heart injury score were investigated after blood transfusion.
Conclusion
AH leads to alteration of the heart, particularly in Cx43 and glycogen reserves, as well as local inflammation.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Gillam-Krakauer, M. & Gowen Jr., C. W. Birth asphyxia. Treasure Island: StatPearls; 2019. www.ncbi.nlm.nih.gov/pubmed/28613533
Correale, M. et al. Troponin in newborns and pediatric patients. Cardiovasc. Hematol. Agents Med. Chem. 7, 270–278 (2009).
Zupan Simunek, V. Definition of intrapartum asphyxia and effects on outcome [Definition de l’asphyxie intrapartum et consequences sur le devenir]. J. Gynecol. Obstet. Biol. Reprod. (Paris) 37(Suppl. 1), S7–S15 (2008).
Shahidi, M., Evazi, G. & Afkhamzadeh, A. Echocardiographic evaluation of cardiovascular complications after birth asphyxia in term neonates. Pak. J. Med. Sci. 33, 1220–1224 (2017).
Donnelly, W. H., Bucciarelli, R. L. & Nelson, R. M. Ischemic papillary muscle necrosis in stressed newborn infants. J. Pediatr. 96, 295–300 (1980).
Simovic, A. M. et al. The role of biochemical markers as early indicators of cardiac damage and prognostic parameters of perinatal asphyxia. Vojn. Pregl. 71, 149–155 (2014).
Mair, J. et al. How is cardiac troponin released from injured myocardium? Eur. Heart J. Acute Cardiovasc. Care https://doi.org/10.1177/2048872617748553 (2017).
El-Khuffash, A. F. & Molloy, E. J. Serum troponin in neonatal intensive care. Neonatology 94, 1–7 (2008).
Doroszko, A. et al. Cardiac dysfunction in an animal model of neonatal asphyxia is associated with increased degradation of MLC1 by MMP-2. Basic Res. Cardiol. 104, 669–679 (2009).
Doroszko, A. et al. Neonatal asphyxia induces the nitration of cardiac myosin light chain 2 that is associated with cardiac systolic dysfunction. Shock 34, 592–600 (2010).
Yu, H., Qing, H. & Lei, Z. Cytidine diphosphate choline improves the outcome of cardiac arrest vs epinephrine in rat model. Am. J. Emerg. Med. 31, 1022–1028 (2013).
Agullo-Pascual, E., Cerrone, M. & Delmar, M. Arrhythmogenic cardiomyopathy and Brugada syndrome: diseases of the connexome. FEBS Lett. 588, 1322–1330 (2014).
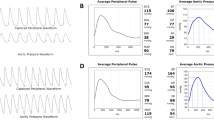
Kalbitz, M. et al. Cardiac depression in pigs after multiple trauma—characterization of posttraumatic structural and functional alterations. Sci. Rep. 7, 17861 (2017).
Kalbitz, M. et al. Complement destabilizes cardiomyocyte function in vivo after polymicrobial sepsis and in vitro. J. Immunol. 197, 2353–2361 (2016).
Mendler, M. R. et al. Successful resuscitation in a model of asphyxia and hemorrhage to test different volume resuscitation strategies. a study in newborn piglets after transition. Front. Pediatr. 6, 192 (2018).
Kalbitz, M. et al. Role of extracellular histones in the cardiomyopathy of sepsis. FASEB J. 29, 2185–2193 (2015).
Bosmann, M. et al. Extracellular histones are essential effectors of C5aR- and C5L2-mediated tissue damage and inflammation in acute lung injury. FASEB J. 27, 5010–5021 (2013).
Braun, C. K. et al. Early structural changes of the heart after experimental polytrauma and hemorrhagic shock. PLoS ONE 12, e0187327 (2017).
Bancalari, A. et al. Myocardial damage following neonatal severe asphyxia [Dano miocardico secundario a asfixia neonatal grave]. Rev. Chil. Pediatr. 62, 232–237 (1991).
Paradis, A. N., Gay, M. S., Wilson, C. G. & Zhang, L. Newborn hypoxia/anoxia inhibits cardiomyocyte proliferation and decreases cardiomyocyte endowment in the developing heart. Role of endothelin-1. PLoS ONE 10, e0116600 (2015).
Haubner, B. J. et al. Functional recovery of a human neonatal heart after severe myocardial infarction. Circ. Res. 118, 216–221 (2016).
Price, J. F. Unique Aspects of Heart Failure in the Neonate (Springer, London, 2011).
Xanthos, T., Vasileiou, P. V. S., Kakavas, S., Syggelou, A. & Iacovidou, N. The potential role of erythropoietin as a pleiotropic agent in post-cardiac arrest syndrome. Curr. Pharm. Des. 17, 1517–1529 (2011).
Miller, A. C., Rosati, S. F., Suffredini, A. F. & Schrump, D. S. A systematic review and pooled analysis of CPR-associated cardiovascular and thoracic injuries. Resuscitation 85, 724–731 (2014).
Zheng, L., Tian, M., Zhang, Y., Dong, P. & Yang, H. Neutrophil extracellular traps were released during intraoperative blood salvage in posterior lumbar surgery. Transfus. Apher. Sci. 57, 259–264 (2018).
Nizet, V. & Johnson, R. S. Interdependence of hypoxic and innate immune responses. Nat. Rev. Immunol. 9, 609–617 (2009).
Marlinge, M. et al. Physiological stress markers during breath-hold diving and SCUBA diving. Physiol. Rep. 7, e14033 (2019).
van den Berg, C. W. et al. Mechanism of neutrophil dysfunction: neutrophil serine proteases cleave and inactivate the C5a receptor. J. Immunol. 192, 1787–1795 (2014).
Wei, Y., Xu, J., Xu, T., Fan, J. & Tao, S. Left ventricular systolic function of newborns with asphyxia evaluated by tissue Doppler imaging. Pediatr. Cardiol. 30, 741–746 (2009).
Sehgal, A., Wong, F. & Mehta, S. Reduced cardiac output and its correlation with coronary blood flow and troponin in asphyxiated infants treated with therapeutic hypothermia. Eur. J. Pediatr. 171, 1511–1517 (2012).
Kalbitz, M. et al. Experimental blunt chest trauma-induced myocardial inflammation and alteration of gap-junction protein connexin 43. PLoS ONE 12, e0187270 (2017).
Dhein, S. Cardiac ischemia and uncoupling: gap junctions in ischemia and infarction. Adv. Cardiol. 42, 198–212 (2006).
Wang, J., Khoury, D. S., Yue, Y., Torre-Amione, G. & Nagueh, S. F. Left ventricular untwisting rate by speckle tracking echocardiography. Circulation 116, 2580–2586 (2007).
Breatnach, C. R., Levy, P. T., James, A. T., Franklin, O. & El-Khuffash, A. Novel echocardiography methods in the functional assessment of the newborn heart. Neonatology 110, 248–260 (2016).
Downing, S. E. & Chen, V. Myocardial hibernation in the ischemic neonatal heart. Circ. Res. 66, 763–772 (1990).
Saha, D. et al. Association of hypoglycemia, hypocalcemia and hypomagnesemia in neonates with perinatal asphyxia. Mymensingh Med J. 24, 244–250 (2015).
Nishino, Y. et al. Ischemic preconditioning activates AMPK in a PKC-dependent manner and induces GLUT4 up-regulation in the late phase of cardioprotection. Cardiovasc. Res. 61, 610–619 (2004).
Kim, J. et al. The responses of tissues from the brain, heart, kidney, and liver to resuscitation following prolonged cardiac arrest by examining mitochondrial respiration in rats. Oxid. Med. Cell. Longev. 2016, 7463407 (2016).
Acknowledgements
We acknowledge support from the Core Facility Konfokale und Multiphotonen Mikroskopie, University of Ulm, which is a multiuser imaging facility. This work was conducted in the framework of the CRC 1149 funded by the Deutsche Forschungsgemeinschaft (DFG, German Research Foundation)—Project number 251293561.
Author information
Authors and Affiliations
Contributions
Substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data: B.W., M.R.M., I.L., J.P., S.H., C.K.B., H.H., S.S., M.K. Drafting the article or revising it critically for important intellectual content: B.W., M.R.M., I.L., M.H.-L., H.H. M.K. Final approval of the version: B.W., M.R.M., I.L., J.P., M.H.-L., S.H., C.K.B., H.H., S.S., M.K.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Weber, B., Mendler, M.R., Lackner, I. et al. Tissue damage in the heart after cardiac arrest induced by asphyxia and hemorrhage in newborn pigs. Pediatr Res 86, 709–718 (2019). https://doi.org/10.1038/s41390-019-0505-6
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-019-0505-6
This article is cited by
-
Early myocardial damage (EMD) and valvular insufficiency result in impaired cardiac function after multiple trauma in pigs
Scientific Reports (2021)
-
Early myocardial damage (EMD) and valvular dysfunction after femur fracture in pigs
Scientific Reports (2021)