Abstract
Background
Psychosocial adversity escalates medical risk for poor outcomes in infants born <30 weeks gestation. Neonatal neurobehavior and maternal psychological and socioenvironmental assessments may identify the earliest specific intervention needs. We hypothesized that maternal prenatal anxiety, depression, and adverse medical and socioenvironmental conditions would be associated with less optimal neonatal neurobehavior at neonatal intensive care unit (NICU) discharge.
Methods
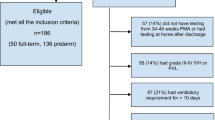
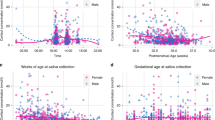
We studied 665 infants at 9 university NICUs. Risk indices of socioenvironmental, maternal, and neonatal medical factors were obtained from standardized, structured maternal interviews and medical record reviews. Brain injuries were classified by consensus ultrasonogram readings. NICU Network Neurobehavioral Scale (NNNS) exams were conducted at NICU discharge.
Results
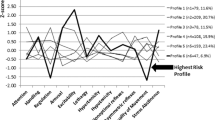
On the NNNS, generalized estimating equations indicated infants of mothers with prenatal anxiety had less optimal attention, and those born to mothers with prenatal depression had increased lethargy. Maternal medical complications predicted suboptimal reflexes. Socioenvironmental risk predicted lower self-regulation and movement quality. Infants with more severe neonatal medical complications had lower attention, increased lethargy, and suboptimal reflexes.
Conclusions
Combined information from the observed associations among adverse prenatal maternal medical and psychosocial conditions, and neonatal complications may assist in the early identification of infants at elevated neurobehavioral risk.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Field, T. Prenatal depression risk factors, developmental effects and interventions: a review. J. Pregnancy Child Health 4, 301 (2017).
Wadhwa, P. D. et al. The contribution of maternal stress to preterm birth: issues and considerations. Clin. Perinatol. 38, 351–384 (2011).
Vohr, B. R. et al. Neurodevelopment: the impact of nutrition and inflammation during preconception and pregnancy in low-resource settings. Pediatrics 139, S38–S49 (2017).
Montagna, A. & Nosarti, C. Socio-emotional development following very preterm birth: pathways to psychopathology. Front. Psychol. 7, 80–80 (2016).
El-Dib, M. et al. Neurobehavioral assessment as a predictor of neurodevelopmental outcome in preterm infants. J. Perinatol. 32, 299–303 (2012).
Bangma, J. T. et al. 2019 Early life antecedents of positive child health among 10-year-old children born extremely preterm. Pediatr. Res. Apr 20. https://doi.org/10.1038/s41390-019-0404-x. [Epub ahead of print].
Montirosso, R. et al. Developmental care, neonatal behavior and postnatal maternal depressive symptomatology predict internalizing problems at 18 months for very preterm children. J. Perinatol. 38, 191–195 (2018).
Hane, A. A. et al. The Welch Emotional Connection Screen: validation of a brief mother–infant relational health screen. Acta Paediatr. 108, 615–625 (2019).
Conradt, E. et al. The roles of DNA methylation of NR3C1 and 11beta-HSD2 and exposure to maternal mood disorder in utero on newborn neurobehavior. Epigenetics 8, 1321–1329 (2013).
Salisbury, A. L. et al. Newborn neurobehavioral patterns are differentially related to prenatal maternal major depressive disorder and serotonin reuptake inhibitor treatment. Depress Anxiety 28, 1008–1019 (2011).
Evans, G. W., Li, D. & Whipple, S. S. Cumulative risk and child development. Psychol. Bull. 139, 1342–1396 (2013).
Joseph, R. M. et al. Maternal educational status at birth, maternal educational advancement, and neurocognitive outcomes at age 10 years among children born extremely preterm. Pediatr. Res. 83, 767 (2017).
Everson, T. M. et al. Epigenome-wide analysis identifies genes and pathways linked to neurobehavioral variation in preterm infants. Sci. Rep. 9, 6322 (2019).
Lester, B. & Tronick, E. The Neonatal Intensive Care Unit Network Neurobehavioral Scale. Pediatrics 113(Suppl. 3, Part 2), 631–695 (2004).
Liu, J. et al. Neonatal neurobehavior predicts medical and behavioral outcome. Pediatrics 125, e90–e98 (2010).
O’Shea, T. M. et al. The ELGAN study of the brain and related disorders in extremely low gestational age newborns. Early Hum. Dev. 85, 719–725 (2009).
Walden, R. V. et al. Major congenital anomalies place extremely low birth weight infants at higher risk for poor growth and developmental outcomes. Pediatrics 120, e1512–e1519 (2007).
Hollingshead, A. B. Four Factor Index of Social Status (Yale Univ., New Haven, CT, 1975).
Vermont-Oxford Network. Manual of Operations (Part 2). http://www.vtoxford.org/tools/manualofoperationspart2.pdf (2013).
Bassler, D. et al. Using a count of neonatal morbidities to predict poor outcome in extremely low birth weight infants: added role of neonatal infection. Pediatrics 123, 313–318 (2009).
Jensen, E. A. et al. The diagnosis of bronchopulmonary dysplasia in very preterm infants: an evidence-based approach. Am. J. Respir. Crit. Care Med. 200, 751–759 (2019).
Kuban, K. et al. Observer variability assessing US scans of the preterm brain: the ELGAN study. Pediatr. Radiol. 37, 1201–1208 (2007).
Pineda, R. G. et al. Patterns of altered neurobehavior in preterm infants within the neonatal intensive care unit. J. Pediatr. 162, 470–476.e471 (2013).
Eeles, A. L. et al. Continuum of neurobehaviour and its associations with brain MRI in infants born preterm. BMJ Paediatr. Open 1, e000136 (2017).
Provenzi, L. et al. NICU Network Neurobehavioral Scale: 1-month normative data and variation from birth to 1 month. Pediatr. Res. 83, 1104–1109 (2018).
McElrath, T. F. et al. Pregnancy disorders that lead to delivery before the 28th week of gestation: an epidemiologic approach to classification. Am. J. Epidemiol. 168, 980–989 (2008).
Stoll, B. J. et al. Neonatal outcomes of extremely preterm infants from the NICHD Neonatal Research Network. Pediatrics 126, 443–456 (2010).
Klass, P. Saving tiny tim—pediatrics and childhood poverty in the United States. N. Engl. J. Med. 374, 2201–2205 (2016).
Lester, B. M. et al. Single-family room care and neurobehavioral and medical outcomes in preterm infants. Pediatrics 134, 754–760 (2014).
Reynolds, L. C. et al. Parental presence and holding in the neonatal intensive care unit and associations with early neurobehavior. J. Perinatol. 33, 636–641 (2013).
Hofheimer, J. A. et al. Respiratory sinus arrhythmia and social interaction patterns in preterm newborns. Infant Behav. Dev. 18, 233–245 (1995).
Lester, B. M. et al. Infant neurobehavioral dysregulation: behavior problems in children with prenatal substance exposure. Pediatrics 124, 1355–1362 (2009).
Spittle, A. J. et al. Neurobehaviour at term-equivalent age and neurodevelopmental outcomes at 2 years in infants born moderate-to-late preterm. Dev. Med. Child Neurol. 59, 207–215 (2017).
Stephens, B. et al. Neurobehavioral assessment predicts motor outcome in preterm infants. J. Pediatr. 156, 366–371 (2010).
Ryckman, J. et al. Sensory processing disorder in preterm infants during early childhood and relationships to early neurobehavior. Early Hum. Dev. 113, 18–22 (2017).
McKinney, J. et al. ACOG Committee Opinion No. 736: optimizing postpartum care. Obstet. Gynecol. 132, 784–785 (2018).
Milgrom, J. et al. Towards parenthood: an antenatal intervention to reduce depression, anxiety and parenting difficulties. J. Affect. Disord. 130, 385–394 (2011).
Melnyk, B. M. et al. Maternal anxiety and depression after a premature infant’s discharge from the neonatal intensive care unit: explanatory effects of the creating opportunities for parent empowerment program. Nurs. Res. 57, 383–394 (2008).
Milgrom, J. et al. Early sensitivity training for parents of preterm infants: impact on the developing brain. Pediatr. Res. 67, 330–335 (2010).
Welch, M. G. et al. Family nurture intervention in the neonatal intensive care unit improves social-relatedness, attention, and neurodevelopment of preterm infants at 18 months in a randomized controlled trial. J. Child Psychol. Psychiatry 56, 1202–1211 (2015).
Acknowledgements
This work was funded by National Institutes of Health (NIH)/Eunice Kennedy Shriver National Institute of Child Health & Human Development (NICHD) Grant R01HD072267. We greatly appreciate the individuals whose expertise has so enriched the NOVI Study: We thank colleagues at the University of North Carolina at Chapel Hill, Samantha Meltzer-Brody, M.D., and Alison Stuebe, M.D., for consultation regarding maternal assessments and well-being; Victoria Childers, RN, Nanette Coulon, Wayne Price, M.D., Carl Seashore, M.D., Karen Wood, M.D., for assistance with multisite NNNS training, Carl Bose, MD, and Martin McCaffrey, MD, for consultation regarding neonatal medical data collection; Brown University faculty Linda LaGasse, Ph.D., for early leadership with the NOVI Data Center, and Lynne Andreozzi Fontaine, Ph.D., for consultation on NNNS training; and ELGAN Study investigators (NIH grant 1U01 NS 40069, Alan Leviton, PI), generously provided us with materials for training and diagnostic criteria regarding brain abnormalities. Our immense gratitude goes to our NOVI families, whose participation has made our study successful, and to the data collection site teams of Co-PIs, coordinators, NNNS examiners, and neuroradiologists listed below, for their commitment to our families and study goals. In memory of Zack Boukydis, PhD, whose caring ways with vulnerable babies and their parents continue to inspire us.
Brown Alpert Medical School and Women and Infants Hospital, Providence, RI: Amy Salisbury, Ph.D., Elizabeth Danella MOT, OTR/L, Lynne Andreozzi, Ph.D., Erica Oliveira, BA, Brenda Rosario Perez, BA, BS.
Children’s Mercy Hospital, Kansas City, MO: Howard Kilbride, M.D., Anne Holmes, RN, MSN, CCRC, Allison Knutson, RNC-NIC, Denise Smith, RN, MSN, RNC, NNP.
Harbor-UCLA Medical Center, Torrance, CA: Lucinda Santos, MHA, Jennifer Huynh, RN.
Miller Children’s and Women’s Hospital Long Beach, Long Beach, CA: Lucinda Santos, MHA, Aimee Burdick, PT, DPT, PCS, Alison Yamaguchi, PT.
Spectrum Health-Helen DeVos Hospital, Grand Rapids, MI: Edgar J. Beaumont, M.D., Virginia DeWitt, BSN, RN, BS, Stephanie Fagerman, MS, MB, Kathy Nystrom, BSN, RN, Emily Gleason, BSN, RN, Karen Pawloski, RN, Rebecca McCurdy, PNP-PC, Jason Powell, PT.
University of Hawaii John A. Burns School of Medicine, Honolulu, HI: Venkataraman Balaraman MBBS, Mari Uehara, M.D., Joann Cheung, MA, CCRC, Micah Tong, CCRP, Pattaraporn Chun, MD, Eydie Nakasone, Jayna Lee.
Wake Forest School of Medicine, Winston Salem, NC: Jennifer Check, M.D., MS, Shannon Green Hanson, Ph.D., MPH, April Stewart, Heather Vye, PT, MPT, PCS, Kerry Dudziak MS, OTR/L, Kristi Lanier, RN, BSN, Nancy Peters, RN, Caroline Ludwig, BS, Melissa Tuttle.
Ultrasound Neuroradiology Consultants: Steve Bezinque, DO, Heather Borders, M.D., Joseph Junewick, M.D., Brad Betz, M.D., Spectrum Health-Helen Devos Hospital; and Barbara Specter, M.D., Wake Forest School of Medicine.
Author information
Authors and Affiliations
Contributions
Dr. Hofheimer conceptualized, designed, drafted, and revised this manuscript with coauthors’ contributions, contributed to the conceptualization and design of the study, and lead the study site teams in protocol implementation and data collection. Drs. Smith, McGowan, Carter, and Neal contributed to the conceptualization and design of the study, reviewed and revised the manuscript, and led their respective sites’ study teams in protocol implementation. Drs. O’Shea and Lester led the conceptualization and design of the study, and critically reviewed and revised the manuscript. Drs. Helderman, Pastrynak, and Soliman reviewed and revised the manuscript, and led their respective sites’ study teams in protocol implementation. Ms. Dansereau developed the database for this manuscript, implemented the statistical analyses, and reviewed and revised the manuscript. Ms. DellaGrotta worked with the study site teams to execute the protocol, supervised data collection, designed the data collection instruments, and reviewed and revised the manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hofheimer, J.A., Smith, L.M., McGowan, E.C. et al. Psychosocial and medical adversity associated with neonatal neurobehavior in infants born before 30 weeks gestation. Pediatr Res 87, 721–729 (2020). https://doi.org/10.1038/s41390-019-0607-1
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-019-0607-1
This article is cited by
-
Neurobehavioral outcomes of preterm infants: toward a holistic approach
Pediatric Research (2025)
-
Early interventions with parental participation and their implications on the neurodevelopment of premature children: a systematic review and meta-analysis
European Child & Adolescent Psychiatry (2025)
-
Epigenetic associations in HPA axis genes related to bronchopulmonary dysplasia and antenatal steroids
Pediatric Research (2024)
-
Environmental influences on child health outcomes: cohorts of individuals born very preterm
Pediatric Research (2023)
-
Prenatal and perinatal factors associated with neonatal neurobehavioral profiles in the ECHO Program
Pediatric Research (2023)