Abstract
Background
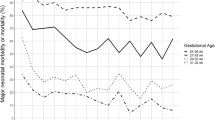
Although the complexity and length of treatment is connected to the newborn’s maturity and birth weight, most case-mix grouping schemes classify newborns by birth weight alone. The objective of this study was to determine whether the definition of thresholds based on a changepoint analysis of variability of birth weight and gestational age contributes to a more homogenous classification.
Methods
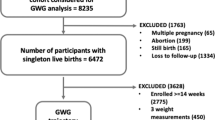
This retrospective observational study was conducted at a Tertiary Care Center with Level III Neonatal Intensive Care and included neonate cases from 2016 through 2018. The institutional database of routinely collected health data was used. The design of this cohort study was explorative. The cases were categorized according to WHO gestational age classes and SwissDRG birth weight classes. A changepoint analysis was conducted. Cut-off values were determined.
Results
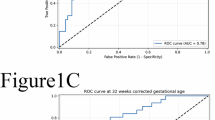
When grouping the cases according to the calculated changepoints, the variability within the groups with regard to case related costs could be reduced. A refined grouping was achieved especially with cases of >2500 g birth weight. An adjusted Grouping Grid for practical purposes was developed.
Conclusions
A novel method of classification of newborn cases by changepoint analysis was developed, providing the possibility to assign costs or outcome indicators to grouping mechanisms by gestational age and birth weight combined.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Blencowe, H. et al. Born too soon: the global epidemiology of 15 million preterm births. Reprod. Health 10, S2 (2013).
Jacob, J. et al. Cost effects of preterm birth: a comparison of health care costs associated with early preterm, late preterm, and full-term birth in the first 3 years after birth. Eur. J. Health Econ. 18, 1041–1046 (2016).
Petrou, S., Yiu, H. H. & Kwon, J. Economic consequences of preterm birth: a systematic review of the recent literature (2009–2017). Arch. Dis. Child. 104, 456–465 (2019).
Soilly, A. L., Lejeune, C., Quantin, C., Bejean, S. & Gouyon, J. B. Economic analysis of the costs associated with prematurity from a literature review. Public Health 128, 43–62, (2014).
Ballantyne, J. W. The problem of the premature infant. BMJ 1, 1196–1200 (1902).
Gilbert, W. M., Nesbitt, T. S. & Danielsen, B. The cost of prematurity: quantification by gestational age and birth weight. Obstet. Gynecol. 102, 488–492 (2003).
Norris, T. et al. Small-for-gestational age and large-for-gestational age thresholds to predict infants at risk of adverse delivery and neonatal outcomes: are current charts adequate? An observational study from the Born in Bradford cohort. BMJ Open 5, e006743 (2015).
Kohn, M. A., Vosti, C. L., Lezotte, D. & Jones, R. H. Optimal gestational age and birth-weight cutoffs to predict neonatal morbidity. Med. Decis. Mak. 20, 369–376 (2000).
Hoftiezer, L., Hukkelhoven, C. W., Hogeveen, M., Straatman, H. M. & van Lingen, R. A. Defining small-for-gestational-age: prescriptive versus descriptive birthweight standards. Eur. J. Pediatr. 175, 1047–1057 (2016).
Wilcox, A. J. On the importance—and the unimportance—of birthweight. Int. J. Epidemiol. 30, 1233–1241 (2001).
Koller-Smith, L. I. et al. Comparing very low birth weight versus very low gestation cohort methods for outcome analysis of high risk preterm infants. BMC Pediatr. 17, 166 (2017).
Lee, A. C. et al. Diagnostic accuracy of neonatal assessment for gestational age determination: a systematic review. Pediatrics 140, e20171423 (2017)
Urquia, M. L., Moineddin, R. & Frank, J. W. A mixture model to correct misclassification of gestational age. Ann. Epidemiol. 22, 151–159 (2012).
Zhang, G., Schenker, N., Parker, J. D. & Liao, D. Identifying implausible gestational ages in preterm babies with Bayesian mixture models. Stat. Med. 32, 2097–2113 (2013).
Tentoni, S., Astolfi, P., De Pasquale, A. & Zonta, L. A. Birthweight by gestational age in preterm babies according to a Gaussian mixture model. BJOG 111, 31–37 (2004).
Bundesamt für Statistik (BFS). Medizinische Statistik der Krankenhäuser [Internet]. Medizinische Stat. der Krankenhäuser - Var. der Medizinischen Stat. Spezifikationen gültig ab 1.1.2019. https://www.bfs.admin.ch/bfs/de/home/statistiken/gesundheit/erhebungen/ms.html (2019) [Accessed 12 Jun 2019].
SwissDRG AG. Definitionshandbuch AV 2019/2019. SwissDRG Syst. 8.0/2019. https://www.swissdrg.org/de/akutsomatik/swissdrg-system-80/definitionshandbuch (2019) [Accessed 12 Jun 2019].
Zhan, C. & Miller, M. R. Administrative data based patient safety research: a critical review. BMJ Qual. Saf. 12, ii58–ii63 (2003).
Reid, B., Palmer, G. & Aisbett, S. The performance of Australian DRGs. Aust. Health Rev. 23, 20–31 (2000).
Benson, T. & Grieve, G. in Principles of Health Interoperability 135–154 (Springer, Cham, 2016).
Knake, L. A. et al. Quality of EHR data extractions for studies of preterm birth in a tertiary care center: guidelines for obtaining reliable data. BMC Pediatr. 16, 59 (2016).
Schreyö, J., Stargardt, T., Tiemann, O. & Busse, R. Methods to determine reimbursement rates for diagnosis related groups (DRG): a comparison of nine European countries. Health Care Manag. 9, 215–223 (2006).
AU IHPA (IHPA). AR-DRG V8.0. Development of the Australian Refined Diagnosis Related Groups V8.0. IHPA. https://www.ihpa.gov.au/publications/development-australian-refined-diagnosis-related-groups-v80 (2015).
Cheah, I. G. S. Economic assessment of neonatal intensive care. Transl. Pediatr. 8, 246–256 (2019).
Battaglia, F. C. & Lubchenco, L. O. A practical classification of newborn infants by weight and gestational age. J. Pediatr. 71, 159–163 (1967).
Trautner, S. Vejledning i korrekt kodning af diagnose og procedurekoder for neonatale børn i DRG. https://static1.squarespace.com/static/5467abcce4b056d72594db79/t/58ed34635016e19ee2569939/1491940453312 (2017) [Accessed 12 Jun 2019].
Petrou, S. Health economic aspects of late preterm and early term birth. Semin. Fetal Neonatal Med. 24, 18–26 (2019).
Hughes, M. M., Black, R. E. & Katz, J. 2500-g low birth weight cutoff: history and implications for future research and policy. Matern. Child Health J. 21, 283–289 (2017).
Olsen, I. E. et al. BMI curves for preterm infants. Pediatrics 135, e572–e581 (2015).
Grantz, K. L., Hediger, M. L., Liu, D. & Buck Louis, G. M. Fetal growth standards: the NICHD fetal growth study approach in context with INTERGROWTH-21st and the World Health Organization Multicentre Growth Reference Study. Am. J. Obstet. Gynecol. 218, S641.e28–S655.e28 (2018).
Chauhan, S. P. et al. Neonatal morbidity of small- and large-for-gestational-age neonates born at term in uncomplicated pregnancies. Obstet. Gynecol. 130, 511–519 (2017).
Kiserud, T. et al. The World Health Organization fetal growth charts: a multinational longitudinal study of ultrasound biometric measurements and estimated fetal weight. PLOS Med. 14, e1002220 (2017).
Aluvaala, J., Collins, G. S., Maina, M., Berkley, J. A. & English, M. A systematic review of neonatal treatment intensity scores and their potential application in low-resource setting hospitals for predicting mortality, morbidity and estimating resource use. Syst. Rev. 6, 248 (2017).
Besson, P. Zertifizierungsverfahren REKOLE® – H+ Die Spitäler der Schweiz https://www.hplus.ch/de/rechnungswesen/zertifizierungsverfahren-rekole/ (2018) [Accessed 12 Jun 2019].
SwissDRG A. G. SwissDRG Antragsverfahren. https://antragsverfahren.swissdrg.org/swissdrg/issues/index_public?utf8=✓&search=gestation&organisation_with_permission%5B%5D=H%2B&commit=Suchen (2018) [Accessed 12 Jun 2019].
Killick, R., Fearnhead, P. & Eckley, I. A. Optimal detection of changepoints with a linear computational cost. J. Am. Stat. Assoc. 107, 1590–1598 (2012).
World Health Organization. International Statistical Classification of Diseases and Related Health Problems 10th Revision (ICD-10)-WHO Version 2016. https://icd.who.int/browse10/2016/en#!/P05.9 (2016) [Accessed 17 Jun 2019].
SwissDRG A. G. SwissDRG:: Definitionshandbuch. https://www.swissdrg.org/de/akutsomatik/swissdrg-system-70/definitionshandbuch (2018) [Accessed 17 Jun 2019].
Buck Louis, G. M., et al. Racial/ethnic standards for fetal growth: the NICHD Fetal Growth Studies. Am. J. Obstet. Gynecol. 213, 449.e1–449.e41 (2015).
Author information
Authors and Affiliations
Contributions
Conception and design: O.E., K.T., M.N., L.R. Acquisition of data: O.E., K.T. Analysis and interpretation of data and drafting the article or revising it critically for important intellectual content: O.E., K.T., N.T., C.T.N. Final approval of the version to be published: all authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Endrich, O., Triep, K., Torbica, N. et al. Changepoint analysis of gestational age and birth weight: proposing a refinement of Diagnosis Related Groups. Pediatr Res 87, 910–916 (2020). https://doi.org/10.1038/s41390-019-0669-0
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-019-0669-0
This article is cited by
-
A tree-structured multiobjective optimization framework for constructing diagnosis-related groups
npj Digital Medicine (2025)