Abstract
Background
There are sparse patient-level data available for children with novel coronavirus disease (COVID-19). Therefore, there is an urgent need for an updated systematic literature review that analyzes individual children rather than aggregated data in broad age groups.
Methods
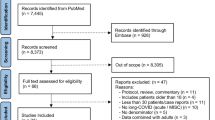
Six databases (MEDLINE, Scopus, Web of Science, CINAHL, Google Scholar, medRxiv) were searched for studies indexed from January 1 to May 15, 2020, with MeSH terms: children, pediatrics, COVID-19, SARS-CoV-2. 1241 records were identified, of which only unique papers in English with individual patient information and documented COVID-19 testing were included. This review of 22 eligible studies followed Preferred Reporting Items for Systematic Review and Meta-Analyses of individual participant data guidelines.
Results
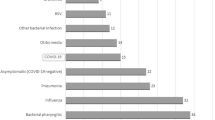
A total of 123 patients from five countries were identified. 46% were females. The median age was 5 years (IQR = 8). At presentation, 62% had a fever, 32% had a cough, 58% had a single symptom, and 21% were asymptomatic. Abnormal chest imaging was seen in 62% (65/105) of imaged and 76.9% (20/26) of asymptomatic children. A minority of children had elevated platelets, CRP, lactate dehydrogenase, and d-dimer.
Conclusion
Data from this independent participant data systematic review revealed that the majority of children with COVID-19 presented with either no symptoms or a single, non-respiratory symptom.
Impact
-
This systematic review revealed that the majority of children with COVID-19 presented with either no symptoms or a single, non-respiratory symptom.
-
By using an independent participant data approach, this analysis underscores the challenge of diagnosing COVID-19 in pediatric patients due to the wide variety of symptoms and seemingly poor correlation of imaging findings with symptomatic disease.
-
The data presented from individual patients from case series or cohort studies add more granularity to the current description of pediatric COVID-19.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Wu, Z. & McGoogan, J. M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) Outbreak in China: summary of a report of 72 314 cases from the Chinese center for disease control and prevention. JAMA 323, 1239–1242 (2020).
Dong, Y. et al. Epidemiology of COVID-19 among children in China. Pediatrics 145, e20200702 (2020).
Chang, T.-H., Wu, J.-L. & Chang, L.-Y. Clinical characteristics and diagnostic challenges of pediatric COVID-19: A systematic review and meta-analysis. J. Formos. Med. Assoc. 119, 982–989 (2020).
Castagnoli, R. et al. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection in children and adolescents: a systematic review. JAMA Pediatr. 174, 882–889 (2020).
Mustafa, N. M. & Selim, L. A. Characterisation of COVID-19 pandemic in paediatric age group: a systematic review and meta-analysis. J. Clin. Virol. 128, 104395 (2020).
Minotti, C., Tirelli, F., Barbieri, E., Giaquinto, C. & Donà, D. How is immunosuppressive status affecting children and adults in SARS-CoV-2 infection? A systematic review. J. Infect. 81, e61–e66 (2020).
Viner, R. M. & Whittaker, E. Kawasaki-like disease: emerging complication during the COVID-19 pandemic. Lancet 395, 1741–1743 (2020).
Jones, V. G. et al. COVID-19 and Kawasaki disease: novel virus and novel case. Hosp. Peds. 10, 537–540 (2020).
Riphagen, S., Gomez, X., Gonzalez-Martinez, C., Wilkinson, N. & Theocharis, P. Hyperinflammatory shock in children during COVID-19 pandemic. Lancet 395, 1607–1608 (2020).
Higgins, J. P. T. & Green, S. Cochrane Handbook for Systematic Reviews of Interventions (Wiley, 2008).
Stewart, L. A. et al. Preferred reporting items for systematic review and meta-analyses of individual participant data: the PRISMA-IPD statement. JAMA 313, 1657–1665 (2015).
Durieux, N., Pasluea, F., & Howick, J. OCEBM Levels of Evidence-CEBM. https://www.cebm.ox.ac.uk/resources/levels-of-evidence/ocebm-levels-of-evidence.
Cai, J. et al. A case series of children with 2019 novel coronavirus infection: clinical and epidemiological features. Clin. Infect. Dis. 28, ciaa198 (2020).
Xu, R. et al. CT imaging of one extended family cluster of corona virus disease 2019 (COVID-19) including adolescent patients and “silent infection”. Quant. Imaging Med. Surg. 10, 800–804 (2020).
Wei, M. et al. Novel coronavirus infection in hospitalized infants under 1 year of age in china. JAMA 323, 1313–1314 (2020).
Zhu, H. et al. Clinical analysis of 10 neonates born to mothers with 2019-nCoV pneumonia. Transl. Pediatr. 9, 51–60 (2020).
Li, W., Cui, H., Li, K., Fang, Y. & Li, S. Chest computed tomography in children with COVID-19 respiratory infection. Pediatr. Radio. 50, 796–799 (2020).
Xing, Y. H. et al. Prolonged viral shedding in feces of pediatric patients with coronavirus disease 2019. J. Microbiol. Immunol. Infect. 53, 473–480 (2020).
Xu, Y. et al. Characteristics of pediatric SARS-CoV-2 infection and potential evidence for persistent fecal viral shedding. Nat. Med. 26, 502–5 (2020).
Ji, L.-N. et al. Clinical features of pediatric patients with COVID-19: a report of two family cluster cases. World J. Pediatr. 16, 267–270 (2020).
Chen, Y. et al. Infants born to mothers with a new coronavirus (COVID-19). Front. pediatrics 8, 104 (2020).
Sun, D. et al. Clinical features of severe pediatric patients with coronavirus disease 2019 in Wuhan: a single center observational study. World J. Pediatr. 16, 251–259 (2020).
Liu, H. et al. Clinical and CT imaging features of the COVID-19 pneumonia: focus on pregnant women and children. J. Infect. 80, e7–13 (2020).
Lou, X. X., Shi, C. X., Zhou, C. C. & Tian, Y. S. Three children who recovered from novel coronavirus 2019 pneumonia. J. Paediatr. Child Health 56, 650–651 (2020).
Liu, M., Song, Z. & Xiao, K. High-resolution computed tomography manifestations of 5 pediatric patients with 2019 novel coronavirus. J. Comp. Assist. Tomogr. 44, 311–313 (2020).
Su, L. et al. The different clinical characteristics of corona virus disease cases between children and their families in China - the character of children with COVID-19. Emerg. Microbes Infect. 9, 707–713 (2020).
Zeng, L. et al. Neonatal early-onset infection with SARS-CoV-2 in 33 neonates born to mothers with COVID-19 in Wuhan, China. JAMA Pediatr. 174, 722–725 (2020).
Zhang, T. et al. Detectable SARS-CoV-2 viral RNA in feces of three children during recovery period of COVID-19 pneumonia. J. Med. Virol. 92, 909–914 (2020).
Liu, W. et al. Clinical characteristics of 19 neonates born to mothers with COVID-19. Front. Med. 14, 193–198 (2020).
Liu, W. et al. Detection of covid-19 in children in early January 2020 in Wuhan, China. N. Engl. J. Med. 382, 1370–1371 (2020).
Shen, Q. et al. Novel coronavirus infection in children outside of Wuhan, China. Pediatr. Pulmonol. 55, 1424–1429 (2020).
Yang, P. et al. Clinical characteristics and risk assessment of newborns born to mothers with COVID-19. J. Clin. Virol. 127, 104356 (2020).
Tan, Y.-P. et al. Epidemiologic and clinical characteristics of 10 children with coronavirus disease 2019 in Changsha, China. J. Clin. Virol. 127, 104353 (2020).
See, K. C. et al. COVID-19: four paediatric cases in Malaysia. Int. J. Infect. Dis. 94, 125–127 (2020).
Paret, M. et al. SARS-CoV-2 infection (COVID-19) in febrile infants without respiratory distress. Clin. Infect. Dis. ciaa452 (2020). https://doi.org/10.1093/cid/ciaa452.
Rahimzadeh, G. et al. COVID-19 infection in Iranian children: a case series of 9 patients. J. Pediatr. Rev. 8, 139–44 (2020).
Parri, N., Lenge, M., Buonsenso, D. & Pediatric Emergency Departments (CONFIDENCE) Research Group. Children with covid-19 in pediatric emergency departments in Italy. N. Engl. J. Med. 383, 187–190 (2020).
Verdoni, L. et al. An outbreak of severe Kawasaki-like disease at the Italian epicentre of the SARS-CoV-2 epidemic: an observational cohort study. Lancet 395, 1771–1778 (2020).
Zheng, F. et al. Clinical characteristics of children with coronavirus disease 2019 in Hubei, China. Curr. Med. Sci. 40, 275–280 (2020).
Xia, W. et al. Clinical and CT features in pediatric patients with COVID-19 infection: different points from adults. Pediatr. Pulmonol. 55, 1169–1174 (2020).
Ludvigsson, J. F. Children are unlikely to be the main drivers of the COVID-19 pandemic—a systematic review. Acta Paediatr. 109, 1525–1530 (2020).
Davies, N. G. et al. Age-dependent effects in the transmission and control of COVID-19 epidemics. Nat. Med. 26, 1205–1211 (2020).
Mantovani, A. et al. Coronavirus disease 2019 (COVID-19) in children and/or adolescents: a meta-analysis. Pediatr. Res. (2020). https://doi.org/10.1038/s41390-020-1015-2.
Mehta, N. S. et al. SARS-CoV-2 (COVID-19): what do we know about children? A systematic review. Clin. Infect. Dis. ciaa556 (2020). https://doi.org/10.1093/cid/ciaa556.
Mirzaee, S. M. M., Gonçalves, F. G., Mohammadifard, M., Tavakoli, S. M., & Vossough, A. Focal cerebral arteriopathy in a COVID-19 pediatric patient. Radiology 202197 (2020). https://doi.org/10.1148/radiol.2020202197.
Dallan, C. et al. Septic shock presentation in adolescents with COVID-19. Lancet Child Adolesc. Health. 4, e21–e23 (2020).
Toubiana, J. et al. Kawasaki-like multisystem inflammatory syndrome in children during the covid-19 pandemic in Paris, France: prospective observational study. BMJ 369, m2094 (2020).
Chiotos, K. et al. Multisystem inflammatory syndrome in children during the COVID-19 pandemic: a case series. J. Pediatr. Infect. Dis. Soc. 9, 393–398 (2020).
World Health Organization. Multisystem Inflammatory Syndrome in Children and Adolescents with COVID-19: Scientific Brief, 15 May 2020 (World Health Organization, 2020).
Rowley, A. H. Understanding SARS-CoV-2-related multisystem inflammatory syndrome in children. Nat. Rev. Immunol. 20, 453–454 (2020).
Capone, C. A. et al. Characteristics, cardiac involvement, and outcomes of multisystem inflammatory disease of childhood (MIS-C) associated with SARS-CoV-2 infection. J. Pediatr. 224, 141–145 (2020).
Dufort, E. et al. Multisystem inflammatory syndrome in children in New York State. New Eng. J. Med. 383, 347–358 (2020).
Feldstein, L. R. et al. Multisystem inflammatory syndrome in U.S. children and adolescents. New Eng. J. Med. 383, 334–346 (2020).
Funding
B.C. was supported by a Medical Scientist Training Program grant from the National Institute of General Medical Sciences of the National Institutes of Health under award number T32GM007739 to the Weill Cornell/Rockefeller/Sloan Kettering Tri-Institutional MD–Ph.D. Program. B.G.M. and I.C.M. were supported by the National Institute of Allergies and Infectious Diseases of the National Institutes of Health award number R25AI140490.
Author information
Authors and Affiliations
Contributions
B.C. conceptualized and designed the study, developed the search strategy and conducted the database search, analyzed the data, drafted the initial manuscript, reviewed and revised the manuscript, and approved the final manuscript for submission. B.G.M. and R.O. conducted the database search, analyzed the data, drafted the initial manuscript, reviewed and revised the manuscript, and approved the final manuscript for submission. W.T.P., T.S., and I.C.M. advised, reviewed and revised the manuscript, and approved the final manuscript for submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent
Patient consent was not required for this study as it analyzed anonymized, publicly available data.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Christophers, B., Gallo Marin, B., Oliva, R. et al. Trends in clinical presentation of children with COVID-19: a systematic review of individual participant data. Pediatr Res 91, 494–501 (2022). https://doi.org/10.1038/s41390-020-01161-3
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-020-01161-3
This article is cited by
-
The association of COVID- 19 parental immunization and transmission of disease to offspring: a retrospective study
Italian Journal of Pediatrics (2025)
-
The flow pattern of neuro-pediatric emergency visits during COVID-19 pandemic
The Egyptian Journal of Neurology, Psychiatry and Neurosurgery (2024)
-
Overlapping research efforts in a global pandemic: a rapid systematic review of COVID-19-related individual participant data meta-analyses
BMC Health Services Research (2023)
-
Implementing the Lolli-Method and pooled RT-qPCR testing for SARS-CoV-2 surveillance in schools: a pilot project
Infection (2023)
-
A snapshot of pediatric inpatients and outpatients with COVID-19: a point prevalence study from Turkey
European Journal of Pediatrics (2023)