Abstract
Background
The impact of pediatric chronic kidney disease (pCKD) on the brain remains poorly defined. The objective of this study was to compare brain morphometry between children with early-stage pCKD and typically developing peers using structural magnetic resonance imaging (MRI).
Methods
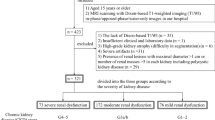
The sample age range was 6–16 years. A total of 18 children with a diagnosis of pCKD (CKD stages 1–3) due to congenital anomalies of the kidney and urinary tract and 24 typically developing peers were included. Volumetric data from MRI and neurocognitive testing were compared using linear models including pCKD status, age, maternal education level, and socioeconomic status.
Results
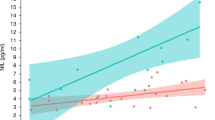
Cerebellar gray matter volume was significantly smaller in pCKD, t(38) = −2.71, p = 0.01. In contrast, cerebral gray matter volume was increased in pCKD, t(38) = 2.08, p = 0.04. Reduced cerebellum gray matter volume was associated with disease severity, operationalized as estimated glomerular filtration rate (eGFR), t(14) = 2.21, p = 0.04 and predicted lower verbal fluency scores in the pCKD sample. Enlarged cerebral gray matter in the pCKD sample predicted lower scores on mathematics assessment.
Conclusions
This study provides preliminary evidence for a morphometric underpinning to the cognitive deficits observed in pCKD.
Impact
-
The impact of pediatric chronic kidney disease (CKD) on the brain remains poorly defined, with no data linking brain morphometry and observed cognitive deficits noted in this population.
-
We explored the relationship between brain morphometry (using structural magnetic resonance imaging), cognition, and markers of CKD.
-
Cerebellar and cerebral gray matter volumes are different in early CKD. Volumetric decreases in cerebellar gray matter are predicted by lower eGFR, suggesting a link between disease and brain morphometry.
-
Reduced cerebellar gray matter predicted lower verbal fluency for those with pCKD. Enlarged cerebral gray matter in the pCKD sample predicted lower mathematics performance.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
The North American Pediatric Renal Trials and Collaborative Studies 2014 Annual Report. Available at: https://web.emmes.com/study/ped/annlrept/annlrept.html. Accessed 10 Jan 2020.
Hooper, S. R. et al. Neurocognitive functioning of children and adolescents with mild-to-moderate chronic kidney disease. Clin. J. Am. Soc. Nephrol. 6, 1824–1830 (2011).
Gerson, A. C. et al. Neurocognitive outcomes in children with chronic kidney disease: current findings and contemporary endeavors. Ment. Retard Dev. Disabil. Res. Rev. 12, 208–215 (2006).
Ruebner, R. L. et al. Neurocognitive dysfunction in children, adolescents, and young adults with CKD. Am. J. Kidney Dis. 67, 567–575 (2016).
Mendley, S. R. et al. Duration of chronic kidney disease reduces attention and executive function in pediatric patients. Kidney Int. 87, 800–806 (2015).
Hooper, S. R. et al. Executive functioning in children, adolescents, and young adults with chronic kidney disease. J. Dev. Behav. Pediatr. 36, 734–742 (2015).
Warady, B. A. & Chadha, V. Chronic kidney disease in children: the global perspective. Pediatr. Nephrol. 22, 1999–2009 (2007).
Moodalbail, D. G. et al. Systematic review of structural and functional neuroimaging findings in children and adults with CKD. Clin. J. Am. Soc. Nephrol. 8, 1429–1448 (2013).
Hartung, E. A. et al. Brain magnetic resonance imaging findings in children and young adults with CKD. Am. J. Kidney Dis. 72, 349–359 (2018).
Lenroot, R. K. et al. Sexual dimorphism of brain developmental trajectories during childhood and adolescence. Neuroimage 36, 1065–1073 (2007).
Schwartz, G. J. et al. Improved equations estimating GFR in children with chronic kidney disease using an immunonephelometric determination of cystatin C. Kidney Int. 82, 445–453 (2012).
Harris, P. A. et al. The REDCap consortium: building an international community of software platform partners. J. Biomed. Inf. 95, 103208 (2019).
Harris, P. A. et al. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inf. 42, 377–381 (2009).
White, N. et al. PROMO: real-time prospective motion correction in MRI using image-based tracking. Magn. Reson. Med. 63, 91–105 (2010).
Pierson, R. et al. Fully automated analysis using BRAINS: AutoWorkup. Neuroimage 54, 328–336 (2011).
Wang, H. et al. Multi-Atlas segmentation with joint label fusion. IEEE Trans. Pattern Anal. Mach. Intell. 35, 611–623 (2013).
Desikan, R. S. et al. An automated labeling system for subdividing the human cerebral cortex on MRI scans into gyral based regions of interest. Neuroimage 31, 968–980 (2006).
Fortin, J. P. et al. Harmonization of cortical thickness measurements across scanners and sites. Neuroimage 167, 104–120 (2018).
Johnson, W. E., Li, C. & Rabinovic, A. Adjusting batch effects in microarray expression data using empirical Bayes methods. Biostatistics 8, 118–127 (2007).
Koscik, T. R. ez.combat. www.github.com/TKosik/ez.combat (2018).
Liu, D. et al. The power-proportion method for intracranial volume correction in volumetric imaging analysis. Front. Neurosci. 8, 356 (2014).
Flynn, J. T., et al. Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics 140, e20171904 (2017).
Brown, T. T. & Jernigan, T. L. Brain development during the preschool years. Neuropsychol. Rev. 22, 313–333 (2012).
Furth, S. L. et al. Design and methods of the Chronic Kidney Disease in Children (CKiD) prospective cohort study. Clin. J. Am. Soc. Nephrol. 1, 1006–1015 (2006).
Lande, M. B. et al. Association of blood pressure variability and neurocognition in children with chronic kidney disease. Pediatr. Nephrol. 31, 2137–2144 (2016).
Amaral, D. G., Schumann, C. M. & Nordahl, C. W. Neuroanatomy of autism. Trends Neurosci. 31, 137–145 (2008).
Foster, N. E. et al. Structural gray matter differences during childhood development in autism spectrum disorder: a multimetric approach. Pediatr. Neurol. 53, 350–359 (2015).
Crump, C. et al. Preterm birth and risk of chronic kidney disease from childhood into mid-adulthood: national cohort study. BMJ 365, l1346 (2019).
Brumbaugh, J. E. et al. Altered brain function, structure, and developmental trajectory in children born late preterm. Pediatr. Res. 80, 197–203 (2016).
Adams-Chapman, I. et al. Neurodevelopmental impairment among extremely preterm infants in the neonatal research network. Pediatrics 141, e20173091 (2018).
Verbitsky, M. et al. Genomic disorders and neurocognitive impairment in pediatric CKD. J. Am. Soc. Nephrol. 28, 2303–2309 (2017).
Acknowledgements
This study was funded by the National Institute of Diabetes and Digestive and Kidney Diseases (K23DK110443 to L.A.H.).
Author information
Authors and Affiliations
Contributions
Research idea and study design: L.A.H., P.D.B., S.L.F., and P.C.N.; data acquisition: M.S., M.N., T.R.K., L.A.H.; data analysis/interpretation: M.S., L.A.H., K.E.L., E.v.P., T.R.K., J.L.S., A.L.C., P.C.N.; supervision or mentorship: L.A.H., P.C.N., P.D.B., and S.L.F. Primary responsibility to drafting the paper: M.S., L.A.H., E.v.P., J.L.S., M.N., P.C.N., P.D.B., and S.L.F. All authors contributed important intellectual content during iterative manuscript drafts or revisions, accepts personal accountability for the author’s own contributions, reviewed the document submitted for review, and agrees to ensure that questions pertaining to the accuracy or integrity of any portion of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Informed consent
Informed consent and/or assent, as applicable, was obtained from participants and legal guardians at the time of participation.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Solomon, M.A., van der Plas, E., Langbehn, K.E. et al. Early pediatric chronic kidney disease is associated with brain volumetric gray matter abnormalities. Pediatr Res 89, 526–532 (2021). https://doi.org/10.1038/s41390-020-01203-w
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-020-01203-w
This article is cited by
-
Neurodevelopmental outcomes in children with chronic kidney disease: a scoping review
Pediatric Nephrology (2025)
-
Systematic review of neuroimaging findings in children and young adults with chronic kidney disease
Pediatric Nephrology (2025)
-
Self-concept and academic achievement in children with chronic kidney disease
Pediatric Nephrology (2024)
-
Common mental health conditions and considerations in pediatric chronic kidney disease
Pediatric Nephrology (2024)
-
Risk factors for neurocognitive impairment and the relation with structural brain abnormality in children and young adults with severe chronic kidney disease
Pediatric Nephrology (2023)