Abstract
Background
Our aim was to investigate the effect of music therapy in combination with skin-to-skin care (SSC) on regional cerebral oxygenation (rSO2) measured with near-infrared spectroscopy (NIRS) in premature infants and to study physiological stability during the interventions.
Methods
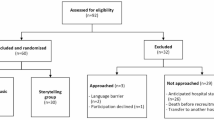
This was a prospective single-center observational cohort study conducted in a tertiary neonatal intensive care unit. The study consisted of four phases: (1) baseline measurements in an incubator for 30 min; (2) quiet SSC for 30 min (SSC-Pre); (3) SSC with live maternal singing accompanied by live guitar music for 20 min (SSC-Music); (4) final quiet SSC for another 30 min (SSC-Post).
Results
The primary outcome measure of mean rSO2 for the 31 preterm infants analyzed showed a significant increase from baseline during SSC-Music (76.87% vs 77.74%, p = 0.04) and SSC-Post (76.87% vs 78.0%, p = 0.03) phases. There were no significant changes observed in heart rate (HR), peripheral oxygen saturation (SpO2), and cerebral fractional tissue oxygen extraction (cFTOE). The coefficient of variation (CV) of rSO2 and SpO2 decreased during each intervention phase.
Conclusion
Combining music therapy with SSC appears to be safe in preterm neonates. The impact of the small increase in rSO2 and reduced variability of SpO2 and rSO2 warrants further investigation.
Impact
-
Music therapy combined with skin-to-skin care (SSC) is safe in clinically stable premature infants and could be encouraged as part of developmental care.
-
This is the first report where near-infrared spectroscopy (NIRS) was used to detect the simultaneous effect of music therapy and SSC on cerebral rSO2 in preterm infants.
-
Music therapy with SSC caused a modest increase in rSO2 and decreased the coefficient of variation of rSO2 and peripheral oxygen saturation (SpO2), which suggest short-term benefits for preterm infants.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Sizun, J. & Westrup, B. Early developmental care for preterm neonates: a call for more research. Arch. Dis. Child Fetal Neonatal Ed. 89, F384–F388 (2004).
Boundy, E. O. et al. Kangaroo mother care and neonatal outcomes: a meta-analysis. Pediatrics 137, e20152238 (2016).
Cirelli, L. K., Jurewicz, Z. B. & Trehub, S. E. Effects of maternal singing style on mother-infant arousal and behavior. J. Cogn. Neurosci. 26, 1–8 (2019).
Bieleninik, L., Ghetti, C. & Gold, C. Music therapy for preterm infants and their parents: a meta-analysis. Pediatrics 138, e20160971 (2016).
DeCasper, A. J. & Fifer, W. P. Of human bonding: newborns prefer their mothers’ voices. Science 208, 1174–1176 (1980).
Moon, C., Cooper, R. P. & Fifer, W. P. Two-days-olds prefer their native language. Infant Behav. Dev. 16, 495–500 (1993).
Loewy, J. NICU music therapy: song of kin as critical lullaby in research and practice. Ann. NY Acad. Sci. 1337, 178–185 (2015).
Shoemark, H., Hanson-Abromeit, D. & Stewart, L. Constructing optimal experience for the hospitalized newborn through neuro-based music therapy. Front. Hum. Neurosci. 9, 487 (2015).
O’Toole, A., Francis, K. & Pugsley, L. Does music positively impact preterm infant outcomes? Adv. Neonatal Care 17, 192–202 (2017).
Filippa, M., Devouche, E., Arioni, C., Imberty, M. & Gratier, M. Live maternal speech and singing have beneficial effects on hospitalized preterm infants. Acta Paediatr. 102, 1017–1020 (2013).
Loewy, J., Stewart, K., Dassler, A. M., Telsey, A. & Homel, P. The effects of music therapy on vital signs, feeding, and sleep in premature infants. Pediatrics 131, 902–918 (2013).
Chorna, O. D., Slaughter, J. C., Wang, L., Stark, A. R. & Maitre, N. L. A pacifier-activated music player with mother’s voice improves oral feeding in preterm infants. Pediatrics 133, 462–468 (2014).
Wolf, M. & Greisen, G. Advances in near-infrared spectroscopy to study the brain of the preterm and term neonate. Clin. Perinatol. 36, 807–834 (2009).
Phillip, A. A., Chan, F. H., Zheng, M. M., Krassioukov, A. V. & Ainslie, P. N. Neurovascular coupling in humans: physiology, methodological advances and clinical implications. J. Cereb. Blood Flow Metab. 36, 647–664 (2016).
da Costa, C. S., Greisen, G. & Austin, T. Is near-infrared spectroscopy clinically useful in the preterm infant? Arch. Dis. Child Fetal Neonatal Ed. 100, F558–F561 (2015).
Hyttel-Sorensen, S. et al. Cerebral near infrared spectroscopy oximetry in extremely preterm infants: phase II randomised clinical trial. BMJ 350, g7635 (2015).
Satti, R. et al. The application of the extended Poincaré plot in the analysis of physiological variabilities. Front. Physiol. 10, 116 (2019).
de Roever, I. et al. Investigation of the pattern of the hemodynamic response as measured by functional near-infrared spectroscopy (fNIRS) studies in newborns, less than a month old: a systematic review. Front. Hum. Neurosci. 12, 371 (2018).
Dix, L. M., van Bel, F., Baerts, W. & Lemmers, P. M. Comparing near-infrared spectroscopy devices and their sensors for monitoring regional cerebral oxygen saturation in the neonate. Pediatr. Res. 74, 557–563 (2013).
Begum, E. A. et al. Cerebral oxygenation responses during kangaroo care in low birth weight infants. BMC Pediatr. 8, 51 (2008).
Lorenz, L. et al. Skin-to-skin care in preterm infants receiving respiratory support does not lead to physiological instability. Arch. Dis. Child Fetal Neonatal Ed. 102, F339–F344 (2017).
Lorenz, L. et al. Cerebral oxygenation during skin-to-skin care in preterm infants not receiving respiratory support. Arch. Dis. Child Fetal Neonatal Ed. 103, F137–F142 (2018).
Sakatani, K., Chen, S., Lichty, W., Zuo, H. & Wang, Y. P. Cerebral blood oxygenation changes induced by auditory stimulation in newborn infants measured by near infrared spectroscopy. Early Hum. Dev. 55, 229–236 (1999).
Dehaene-Lambertz, G. et al. Language or music, mother or Mozart? Structural and environmental influences on infants’ language networks. Brain Lang. 114, 53–65 (2010).
Arnon, S. et al. Maternal singing during kangaroo care led to autonomic stability in preterm infants and reduced maternal anxiety. Acta Paediatr. 103, 1039–1044 (2014).
Teckenberg-Jansson, P., Huotilainen, M., Pölkki, T., Lipsanen, J. & Järvenpää, A. L. Rapid effects of neonatal music therapy combined with kangaroo care on prematurely-born infants. Nord. J. Music Ther. 20, 22–42 (2011).
York, J. R., Landers, S., Kirby, R. S., Arbogast, P. G. & Penn, J. S. Arterial oxygen fluctuation and retinopathy of prematurity in very-low-birth-weight infants. J. Perinatol. 24, 82–87 (2004).
Cardoso, S., Silva, M. J. & Guimarães, H. Autonomic nervous system in newborns: a review based on heart rate variability. Childs Nerv. Syst. 33, 1053–1063 (2017).
Bohanon, F. J. et al. Heart rate variability analysis is more sensitive at identifying neonatal sepsis than conventional vital signs. Am. J. Surg. 210, 661–667 (2015).
Bahrick, L. E., McNew, M. E., Pruden, S. M. & Castellanos, I. Intersensory redundancy promotes infant detection of prosody in infant-directed speech. J. Exp. Child Psychol. 183, 295–309 (2019).
Filippa, M. et al. Early vocal contact and music in the NICU: new insights into preventive interventions. Pediatr. Res. 87, 249–264 (2020).
Acknowledgements
We wish to thank our statistician Laszlo Szakacs, research student Dr. Eszter Sandor, and cognitive psychologist Anett Rago and Zsuzsanna Varga for their valuable contributions. We would also like to thank our medical and nursing NICU team at the 1st Department of Pediatrics for the professional care and support in facilitating this study. A.J. was supported by the Hungarian Academy of Science, Premium Postdoctoral Fellowship (PPD460004). U.M. was supported by the Higher Education Institutional Excellence Program of the Ministry for Innovation and Technology in Hungary, within the framework of the Neurology thematic program of the Semmelweis University. The funding agencies had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
Author information
Authors and Affiliations
Contributions
Each author has met the Pediatric Research authorship requirements. Substantial contributions to conception and design: U.M., T.H., G.B., M.S., and A.J. Acquisition of data, or analysis and interpretation of data: U.M., E.T., K.K., E.S., A.J.C., T.H., and A.J. Drafting the article or revising it critically for important intellectual content and final approval of the version to be published: U.M., E.T., K.K., E.S., A.J.C., T.H., M.S., G.B., and A.J.
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Ethics approval
The study was approved by the Ethics Committee of the National Medical Research Council (ETT-TUKEB 13030-1/2017/EKU). Written informed parental consent was obtained for all participants.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Meder, U., Tarjanyi, E., Kovacs, K. et al. Cerebral oxygenation in preterm infants during maternal singing combined with skin-to-skin care. Pediatr Res 90, 809–814 (2021). https://doi.org/10.1038/s41390-020-01235-2
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-020-01235-2
This article is cited by
-
Creative music therapy in preterm infants effects cerebrovascular oxygenation and perfusion
Scientific Reports (2024)