Abstract
Background
Chronic lung disease remains a burden for extremely preterm infants. The changes in ventilation over time and optimal ventilatory management remains unknown. Newer, non-invasive technologies provide insight into these patterns.
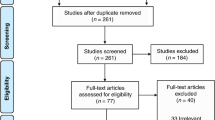
Methods
This single-center prospective cohort study enrolled infants ≤32 0/7 weeks. We obtained epochs of transcutaneous carbon dioxide (TcCO2) measurements twice each week to describe the pattern of hypercarbia throughout their hospitalization.
Results
Patterns of hypercarbia varied based on birth gestational age and post-menstrual age (PMA) (p = 0.03), regardless of respiratory support. Infants receiving the most respiratory support had values 16–21 mmHg higher than those on room air (p < 0.001). Infants born at the youngest gestational ages had the greatest total change but the rate of change was slower (p = 0.049) compared to infants born at later gestational ages. All infants had TcCO2 values stabilize by 31–33 weeks PMA, when values were not significantly different compared to discharge. No rebound was observed when infants weaned off invasive support.
Conclusions
Hypercarbia improves as infants approached 31–33 weeks PMA. Hypercarbia was the highest in the most immature infants and improved with age and growth despite weaning respiratory support.
Impact
-
This study describes the evolution of hypercarbia as very preterm infants grow and develop.
-
The pattern of ventilation is significantly different depending on the gestational age at birth and post-menstrual age.
-
Average transcutaneous carbon dioxide (TCO2) decreased over time as infants became more mature despite weaning respiratory support. This improvement was most significant in infants born at the lowest gestational ages.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Laughon, M. M. et al. Prediction of bronchopulmonary dysplasia by postnatal age in extremely premature infants. Am. J. Respir. Crit. Care Med. 183, 1715–1722 (2011).
Smith, V. C. et al. Trends in severe bronchopulmonary dysplasia rates between 1994 and 2002. J. Pediatr. 146, 469–473 (2005).
Younge, N. et al. Survival and neurodevelopmental outcomes among periviable infants. N. Engl. J. Med. 376, 617–628 (2017).
Younge, N. et al. Improved survival and neurodevelopmental outcomes among extremely premature infants born near the limit of viability. Early Hum. Dev. 95, 5–8 (2016).
Stoll, B. J. et al. Trends in care practices, morbidity, and mortality of extremely preterm neonates, 1993-2012. JAMA 314, 1039–1051 (2015).
Natarajan, G. et al. Outcomes of extremely low birth weight infants with bronchopulmonary dysplasia: impact of the physiologic definition. Early Hum. Dev. 88, 509–515 (2012).
Jobe, A. H. & Steinhorn, R. Can we define bronchopulmonary dysplasia? J. Pediatr. 188, 19–23 (2017).
Cheong, J. L. & Doyle, L. W. An update on pulmonary and neurodevelopmental outcomes of bronchopulmonary dysplasia. Semin. Perinatol. 42, 478–484 (2018).
Stoll, B. J. et al. Neonatal outcomes of extremely preterm infants from the NICHD Neonatal Research Network. Pediatrics 126, 443–456 (2010).
Anderson, P. J. & Doyle, L. W. Neurodevelopmental outcome of bronchopulmonary dysplasia. Semin. Perinatol. 30, 227–232 (2006).
Gibson, A.-M. & Doyle, L. W. Respiratory outcomes for the tiniest or most immature infants. Semin. Fetal Neonatal Med. 19, 105–111 (2014).
Doyle, L. W. & Anderson P. J. Long-term outcomes of bronchopulmonary dysplasia. Semin. Fetal Neonatal Med. 14, 391–395 (2009).
Doyle, L. W. et al. Bronchopulmonary dysplasia in very low birth weight subjects and lung function in late adolescence. Pediatrics 118, 108–113 (2006).
Greenough, A. Long-term pulmonary outcome in the preterm infant. Neonatology 93, 324–327 (2008).
Greenough, A. et al. Health care utilisation of infants with chronic lung disease, related to hospitalisation for RSV infection. Arch. Dis. Child. 85, 463–468 (2001).
Van Marter, L. J. et al. Does bronchopulmonary dysplasia contribute to the occurrence of cerebral palsy among infants born before 28 weeks of gestation? Arch. Dis. Child. Fetal Neonatal Ed. 96, F20–F29 (2011).
Collins, M. P., Lorenz, J. M., Jetton, J. R. & Paneth, N. Hypocapnia and other ventilation-related risk factors for cerebral palsy in low birth weight infants. Pediatr. Res. 50, 712–719 (2001).
Keszler, M. & Sant’Anna, G. Mechanical ventilation and bronchopulmonary dysplasia. Clin. Perinatol. 42, 781–796 (2015).
Carlo, W. Gentle ventilation: the new evidence from the SUPPORT, COIN, VON, CURPAP, Colombian Network, and Neocosur Network trials. Early Hum. Dev. 88, S81–S83 (2012).
Kennedy, K. A., Cotten, C. M., Watterberg, K. L. & Carlo, W. A. Prevention and management of bronchopulmonary dysplasia: lessons learned from the Neonatal Research Network. Semin. Perinatol. 40, 348–355 (2016).
Davis, P. G., Morley, C. J. & Owen, L. S. Non-invasive respiratory support of preterm neonates with respiratory distress: continuous positive airway pressure and nasal intermittent positive pressure ventilation. Semin. Fetal Neonatal Med. 14, 14–20 (2009).
Thome, U. H. & Ambalavanan, N. Permissive hypercapnia to decrease lung injury in ventilated preterm neonates. Semin. Fetal Neonatal Med. 14, 21–27 (2009).
Thome, U. H. & Carlo, W. A. Permissive hypercapnia. Semin. Neonatol. 7, 409–419 (2002).
Thome, U. H. et al. Permissive hypercapnia in extremely low birthweight infants (PHELBI): a randomised controlled multicentre trial. Lancet Respir. Med. 3, 534–543 (2015).
Mariani, G., Cifuentes, J. & Carlo, W. A. Randomized trial of permissive hypercapnia in preterm infants. Pediatrics 104, 1082–1088 (1999).
Ambalavanan, N. et al. PaCO2 in surfactant, positive pressure, and oxygenation randomised trial (SUPPORT). Arch. Dis. Child. Fetal Neonatal Ed. 100, F145–F149 (2015).
Fabres, J., Carlo, W. A., Phillips, V., Howard, G. & Ambalavanan, N. Both extremes of arterial carbon dioxide pressure and the magnitude of fluctuations in arterial carbon dioxide pressure are associated with severe intraventricular hemorrhage in preterm infants. Pediatrics 119, 299–305 (2007).
McKee, L. A. et al. PaCO2 and neurodevelopment in extremely low birth weight infants. J. Pediatr. 155, 217–221. e211 (2009).
Hagen, E. W., Sadek-Badawi, M., Carlton, D. P. & Palta, M. Permissive hypercapnia and risk for brain injury and developmental impairment. Pediatrics 122, e583–e589 (2008).
Toms, R. & Ambalavanan, N. Permissive hypercapnia during mechanical ventilation of neonates. Indian Pediatr. 41, 775–778 (2004).
Varughese, M., Patole, S., Shama, A. & Whitehall, J. Permissive hypercapnia in neonates: the case of the good, the bad, and the ugly. Pediatr. Pulmonol. 33, 56–64 (2002).
Chonghaile, M. N., Higgins, B. & Laffey, J. G. Permissive hypercapnia: role in protective lung ventilatory strategies. Curr. Opin. Crit. Care 11, 56–62 (2005).
Miller, J. D. & Carlo, W. A. Safety and effectiveness of permissive hypercapnia in the preterm infant. Curr. Opin. Pediatr. 19, 142–144 (2007).
Berardesca, E. & Maibach, H. Transcutaneous CO2 and O2 diffusion. Ski. Pharmacol. Physiol. 6, 3–9 (1993).
Domingo, C. et al. Transcutaneous measurement of partial pressure of carbon dioxide and oxygen saturation: validation of the SenTec monitor. Arch. Bronconeumol. 42, 246–251 (2006).
Hejlesen, O. K., Cichosz, S. L., Vangsgaard, S., Andresen, M. F. & Madsen, L. P. Clinical implications of a quality assessment of transcutaneous CO2 monitoring in preterm infants in neonatal intensive care. Stud. Health Technol. Inf. 150, 490–494 (2009).
Tobias, J. D. Transcutaneous carbon dioxide monitoring in infants and children. Pediatr. Anesth. 19, 434–444 (2009).
Hochwald, O. et al. Continuous noninvasive carbon dioxide monitoring in neonates: from theory to standard of care. Pediatrics 144, e20183640 (2019).
Mukhopadhyay, S., Maurer, R. & Puopolo, K. M. Neonatal transcutaneous carbon dioxide monitoring—effect on clinical management and outcomes. Respir. Care 61, 90–97 (2016).
Rhein, L. et al. Optimizing noninvasive respiratory support in the delivery room and early caffeine initiation to decrease bronchopulmonary dysplasia amongst infants born ≤32 & 0/7 weeks gestational age. Am. J. Respir. Crit. Care Med. 197, A6124 (2018).
Thome, U. H. et al. Neurodevelopmental outcomes of extremely low birthweight infants randomised to different PCO2 targets: the PHELBI follow-up study. Arch. Dis. Child. Fetal Neonatal Ed. 102, F376–F382 (2017).
Lam, R. et al. The effect of extended continuous positive airway pressure on changes in lung volumes in stable premature infants: a randomized controlled trial. J. Pediatr. 217, 66–72. e61 (2020).
Thomson, M. A. et al. Treatment of immature baboons for 28 days with early nasal continuous positive airway pressure. Am. J. Respir. Crit. Care Med. 169, 1054–1062 (2004).
Zhang, S., Garbutt, V. & McBride, J. T. Strain-induced growth of the immature lung. J. Appl. Physiol. 81, 1471–1476 (1996).
Friedrich, L. et al. Growth rate of lung function in healthy preterm infants. Am. J. Respir. Crit. Care Med. 176, 1269–1273 (2007).
Jones, M. Effect of preterm birth on airway function and lung growth. Paediatr. Respir. Rev. 10, 9–11 (2009).
Panagiotounakou, P. et al. Very preterm neonates receiving “aggressive” nutrition and early nCPAP had similar long-term respiratory outcomes as term neonates. Pediatr. Res. 86, 742–748 (2019).
Maritz, G. S., Cock, M. L., Louey, S., Suzuki, K. & Harding, R. Fetal growth restriction has long-term effects on postnatal lung structure in sheep. Pediatr. Res. 55, 287–295 (2004).
Jobe, A. H. An Unknown: Lung Growth and Development after Very Preterm Birth (American Thoracic Society, 2002).
Ali, K. et al. Prediction of prolonged ventilator dependence in preterm infants. Eur. J. Pediatr. 178, 1063–1068 (2019).
O’Reilly, M., Sozo, F. & Harding, R. Impact of preterm birth and bronchopulmonary dysplasia on the developing lung: long-term consequences for respiratory health. Clin. Exp. Pharmacol. Physiol. 40, 765–773 (2013).
Acknowledgements
No financial assistance was received in support of this study. SenTec loaned several transcutaneous carbon dioxide monitors for use in this prospective cohort study.
Author information
Authors and Affiliations
Contributions
Each author has met the Pediatric Research authorship requirements. All authors made substantial contributions to the conception and design, acquisition of data, and/or analysis and interpretation of data. K.P.S. drafted the article. K.P.S., L.M.R., and H.O.W. revised it critically for important intellectual content. L.M.R., H.O.W., L.E.G., J.J.N., and A.F.L. all gave final approval of the version to be submitted for publication.
Corresponding author
Ethics declarations
Competing interests
None of the authors have any financial ties to the products used in the study.
Consent statement
Informed consent was obtained from the parents or guardians prior to enrollment.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sullivan, K.P., White, H.O., Grover, L.E. et al. Transcutaneous carbon dioxide pattern and trend over time in preterm infants. Pediatr Res 90, 840–846 (2021). https://doi.org/10.1038/s41390-020-01308-2
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-020-01308-2