Abstract
Background
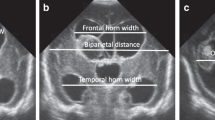
The aims of this study were to find the normal value of fronto-temporal horn ratio (FTHR) as a marker of ventriculomegaly on cranial ultrasound (CUS) in premature newborns and the relation to white matter injury (WMI) and cerebral palsy (CP).
Methods
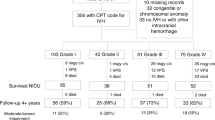
This is a retrospective study of newborns admitted between 2011 and 2014. Inclusion criteria were: (1) gestation <29 weeks, (2) birth weight ≤1500 g, (3) referred within 7 days of life, (4) at least two CUS preformed, (5) brain magnetic resonance imaging (MRI) at term age-equivalent. Intraventricular hemorrhage (IVH) grade was identified and FTHR was measured on all CUS. WMI on MRI was evaluated through (1) injury score (Kidokoro 2013) and (2) fractional anisotropy (FA) on the MRI diffusion tensor imaging. CP was estimated using the gross motor function classification system (GMFCS).
Results
One hundred neonates met the inclusion criteria: 37 with no IVH, 36 with IVH grade 1–2, and 27 with IVH grade 3–4. The FTHR cut-point of 0.51 had the highest sensitivity and specificity for moderate-to-severe WMI. In the IVH grade 3–4 group, the elevated FTHR correlated with lower FA and higher GMFCS.
Conclusions
FTHR is a useful quantitative biomarker of ventriculomegaly in preterm newborns. It may help standardize ventricular measurement and direct intervention.
Impact
-
The fronto-temporal horn ratio has the potential to become a standardized tool that can provide an actionable measure to direct intervention for post-hemorrhagic ventricular dilation.
-
This current study will provide the basis of a future clinical trial to optimize intervention timing to decrease the risk of white matter injury in this vulnerable population.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Winter, S., Autry, A., Boyle, C. & Yeargin-Allsopp, M. Trends in the prevalence of cerebral palsy in a population-based study. Pediatrics 110, 1220–1225 (2002).
Shankaran, S. et al. Outcome after posthemorrhagic ventriculomegaly in comparison with mild hemorrhage without ventriculomegaly. J. Pediatr. 114, 109–114 (1989).
Hintz, S. R. et al. Neuroimaging and neurodevelopmental outcome in extremely preterm infants. Pediatrics 135, e32–e.42 (2015).
Srinivasakumar, P. et al. Posthemorrhagic ventricular dilatation-impact on early neurodevelopmental outcome. Am. J. Perinatol. 30, 207–214 (2013).
Dyet, L. E. et al. Natural history of brain lesions in extremely preterm infants studied with serial magnetic resonance imaging from birth and neurodevelopmental assessment. Pediatrics 118, 536–548 (2006).
Del Bigio, M. R., Kanfer, J. N. & Zhang, Y. W. Myelination delay in the cerebral white matter of immature rats with kaolin-induced hydrocephalus is reversible. J. Neuropathol. Exp. Neurol. 56, 1053–1066 (1997).
Del Bigio, M. R., Wilson, M. J. & Enno, T. Chronic hydrocephalus in rats and humans: white matter loss and behavior changes. Ann. Neurol. 53, 337–346 (2003).
Ment, L. R. et al. Practice parameter: neuroimaging of the neonate: report of the Quality Standards Subcommittee of the American Academy of Neurology and the Practice Committee of the Child Neurology Society. Neurology 58, 1726–1738 (2002).
Riva-Cambrin, J. et al. Center effect and other factors influencing temporization and shunting of cerebrospinal fluid in preterm infants with intraventricular hemorrhage. J. Neurosurg. Pediatr. 9, 473–481 (2012).
Brouwer, M. J. et al. New reference values for the neonatal cerebral ventricles. Radiology 262, 224–233 (2012).
de Vries, L. S. et al. Treatment thresholds for intervention in posthaemorrhagic ventricular dilation: a randomised controlled trial. Arch. Dis. Child. Fetal Neonatal Ed. 104, F70–F75 (2019).
Cizmeci, M. N. et al. Periventricular hemorrhagic infarction in very preterm infants: characteristic sonographic findings and association with neurodevelopmental outcome at age 2 years. J. Pediatr. 217, 79.e1–85.e1 (2020).
Cizmeci, M. N. et al. Randomized controlled early versus late ventricular intervention study in posthemorrhagic ventricular dilatation: outcome at 2 years. J. Pediatr. 226, 28.E3–35.E3 (2020).
Antes, S. et al. The frontal and temporal horn ratio to assess dimension of paediatric hydrocephalus: a comparative volumetric study. Acta Neurochir. Suppl. 118, 211–214 (2013).
Radhakrishnan, R. et al. Frontal occipital and frontal temporal horn ratios: comparison and validation of head ultrasound-derived indexes with mri and ventricular volumes in infantile ventriculomegaly. AJR Am. J. Roentgenol. 213, 925–931 (2019).
Wellons, J. C. 3rd et al. Shunting outcomes in posthemorrhagic hydrocephalus: results of a Hydrocephalus Clinical Research Network prospective cohort study. J. Neurosurg. Pediatr. 20, 19–29 (2017).
Papile, L. A. et al. Posthemorrhagic hydrocephalus in low-birth-weight infants: treatment by serial lumbar punctures. J. Pediatr. 97, 273–277 (1980).
Kidokoro, H., Neil, J. J. & Inder, T. E. New MR imaging assessment tool to define brain abnormalities in very preterm infants at term. AJNR Am. J. Neuroradiol. 34, 2208–2214 (2013).
Palisano, R. J., Copeland, W. P. & Galuppi, B. E. Performance of physical activities by adolescents with cerebral palsy. Phys. Ther. 87, 77–87 (2007).
Akbari, S. H. et al. Periventricular hyperintensity in children with hydrocephalus. Pediatr. Radiol. 45, 1189–1197 (2015).
Zhang, S. et al. Alterations in cortical thickness and white matter integrity in mild-to-moderate communicating hydrocephalic school-aged children measured by whole-brain cortical thickness mapping and DTI. Neural Plast. 2017, 5167973 (2017).
Olopade, F. E., Shokunbi, M. T. & Siren, A. L. The relationship between ventricular dilatation, neuropathological and neurobehavioural changes in hydrocephalic rats. Fluids Barriers CNS 9, 19 (2012).
Yuan, W. et al. Diffusion tensor imaging properties and neurobehavioral outcomes in children with hydrocephalus. AJNR Am. J. Neuroradiol. 34, 439–445 (2013).
Cardoso, E. J., Lachat, J. J., Lopes, L. S., Santos, A. C. & Colli, B. O. Changes caused by hydrocephalus, induced by kaolin, in the corpus callosum of adult dogs. Acta Cir. Bras. 26, 8–14 (2011).
Liu, F. et al. Ultrasound measurement of the corpus callosum and neural development of premature infants. Neural Regen. Res. 8, 2432–2440 (2013).
Malavolti, A. M. et al. Association between corpus callosum development on magnetic resonance imaging and diffusion tensor imaging, and neurodevelopmental outcome in neonates born very preterm. Dev. Med. Child Neurol. 59, 433–440 (2017).
de Vries, L. S. et al. Early versus late treatment of posthaemorrhagic ventricular dilatation: results of a retrospective study from five neonatal intensive care units in The Netherlands. Acta Paediatr. 91, 212–217 (2002).
Leijser, L. M. et al. Posthemorrhagic ventricular dilatation in preterm infants: when best to intervene? Neurology 90, e698–e706 (2018).
Cizmeci, M. N. et al. Assessment of brain injury and brain volumes after posthemorrhagic ventricular dilatation: a nested substudy of the randomized controlled ELVIS trial. J. Pediatr. 208, 191.e2–197.e2 (2019).
Acknowledgements
This work was funded by an Early Career Award through the Thrasher Foundation.
Author information
Authors and Affiliations
Contributions
R.O. conceptualized and designed the study and acquired the data, including the chart review and the technical analysis of the cranial ultrasound and brain MRI images. He drafted the article and revised it multiple times. He approved the final version for publication. T.C. conceptualized and designed the study and helped drafting the manuscript and revising it for important intellectual content. She approved the final version for publication. E.B. helped in acquiring and managing the data in Redcap. She also helped in analyzing the data. She critically reviewed and approved the final version of the manuscript for publication. J.G.M. helped conceptualize and design the study. He contributed significantly to the data acquisition by reviewing the brain imaging (brain MRI). He also helped critically revising the final manuscript for important intellectual content and approved the final version to be published. D.B. conceptualized and designed the study, helped in reviewing the cranial ultrasound images, reviewed the manuscript critically for important intellectual content, and approved the final version to be published. A.B. contributed to the acquisition of the data, reviewed the cranial ultrasound images, helped in revising the article for important intellectual content, and approved the final version to be published. C.O. conceptualized and designed the study and reviewed the manuscript for important intellectual content. He reviewed the manuscript and approved the final version to be published. M.J. conceptualized and designed the study, performed the statistical analysis and helped in interpreting the data. She reviewed the manuscript and approved the final version for publication. A.N.M. conceptualized and designed the study, planned the statistical analysis, helped significantly in interpreting the data, reviewed the manuscript critically, and approved the final version to be published. A.A.P. conceptualized and designed the study, mentored the primary investigator, planned the statistical analysis, helped with data interpretation, critically reviewed the manuscript, and approved the final version to be published. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Patient consent statement
Patient consent was not required.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Obeid, R., Jacobs, M., Chang, T. et al. The utility of the fronto-temporal horn ratio on cranial ultrasound in premature newborns: a ventriculomegaly marker. Pediatr Res 89, 1715–1723 (2021). https://doi.org/10.1038/s41390-020-01337-x
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-020-01337-x
This article is cited by
-
Prediction of short- and long-term outcomes using pre-operative ventricular size in infants with post-hemorrhagic ventricular dilation
Child's Nervous System (2024)
-
Post-hemorrhagic ventricular dilatation affects white matter maturation in extremely preterm infants
Pediatric Research (2022)
-
Degree of ventriculomegaly predicts school-aged functional outcomes in preterm infants with intraventricular hemorrhage
Pediatric Research (2022)
-
Ventriculomegaly thresholds for prediction of symptomatic post-hemorrhagic ventricular dilatation in preterm infants
Pediatric Research (2022)