Abstract
Background
Very low birth weight (VLBW) infants may be at risk for late-onset circulatory collapse (LCC) where otherwise stable infants develop hypotension resistant to vasoactive agents. The risk factors for LCC development are poorly defined, and it has been theorized that it may be in part due to withdrawal from exogenous prenatal steroids. The goal of this study was to define the clinical characteristics of LCC and investigate its association with antenatal steroid administration.
Methods
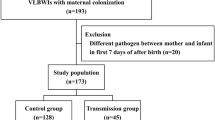
This is a retrospective cohort study of infants born ≤1500 g. LCC was retrospectively diagnosed in infants requiring glucocorticoids for circulatory instability at >1 week of life. Demographic and clinical characteristics were compared between groups using Mann–Whitney test.
Results
Three hundred and ten infants were included; 19 (6.1%) developed LCC. Infants with LCC were born at a median 4.6 weeks’ lower gestation, 509 g lower birth weight than those without LCC. There was no difference in antenatal steroid delivery between the groups.
Conclusions
LCC occurs in a distinct subset of VLBW infants, suggesting the need for monitoring in this high-risk population. Antenatal steroids did not significantly increase the risk of LCC development in this study.
Impact
-
Late-onset circulatory collapse (LCC) is a life-threatening clinical entity occurring in around 6% in VLBW infants and is likely underdiagnosed in the United States.
-
Targeting specific demographic characteristics such as birth weight (<1000 g) and gestational age at birth (<26 weeks) may allow for early identification of high-risk infants, allowing close monitoring and prompt treatment of LCC.
-
No significant association was found between antenatal steroid administration and LCC development, suggesting that the theoretical risks of antenatal steroids on the fetal HPA axis does not outweigh the benefits of antenatal steroids in fetal lung maturity.
-
To date, no studies characterizing LCC have originated outside of Asia. Therefore, providing a description of LCC in a U.S.-based cohort will provide insight into both its prevalence and presentation to inform clinicians about this potentially devastating disorder and foster early diagnosis and treatment.
-
This study validates LCC characteristics and prevalence previously outlined by Asian studies in a single-center U.S.-based cohort while also identifying potential risk factors for LCC development.
-
This manuscript will provide education for U.S. physicians about the risk factors and clinical presentation of LCC to facilitate early diagnosis and treatment, potentially decreasing neonatal mortality.
-
With prompt recognition and treatment of LCC, infants may have decreased exposure to vasoactive medications that have significant systemic effects.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Murphy, S. L., Mathews, T. J., Martin, J. A., Minkovitz, C. S. & Strobino, D. M. Annual summary of vital statistics: 2013–2014. Pediatrics 139, e20163239 (2017).
Platt, M. J. Outcomes in preterm infants. Public Health 128, 399–403 (2014).
Numerato, D. et al. Mortality and length of stay of very low birth weight and very preterm infants: a EuroHOPE study. PLoS ONE 10, e0131685 (2015).
Miwa, M., Kusuda, S. & Ikeda, K. Late-onset circulatory collapse in very low-birthweight infants: a Japanese perspective. NeoReviews 10, e381 (2009).
Ji Lee, W. et al. Clinical features of late-onset circulatory collapse in preterm infants. Korean J. Perinatol. 24, 148–157 (2013).
Suzuki, Y. et al. Neonatal factors related to center variation in the incidence of late-onset circulatory collapse in extremely preterm infants. PLoS ONE 13, e0198518 (2018).
Fernandez, E. F. & Watterberg, K. L. Relative adrenal insufficiency in the preterm and term infant. J. Perinatol. 29, 44 (2009).
Matthews, T. J., MacDorman, M. F. & Thoma, M. E. Infant mortality statistics from the 2013 period linked birth/infant death data set. Natl Vital Stat. Rep. 64, 1–30 (2015).
Wang, C. H. et al. Analysis of in-hospital neonatal death in the tertiary neonatal intensive care unit in China: a multicenter retrospective study. Chin. Med. J. (Engl.) 129, 2652–2658 (2016).
Schraufnagel, D. E. in Breathing in America: Diseases, Progress, and Hope 197–205 (American Thoracic Society, 2010).
El-Sayed, Y. Y., Borders, A. E. & Gyanfi-Bannerman, C. ACOG Committee Opinion: antenatal corticosteroid therapy for fetal maturation. Obstet. Gynecol. 130, 102–109 (2017).
Bunt, J. et al. The effect in premature infants of prenatal corticosteroids on endogenous surfactant synthesis as measured with stable isotopes. Pediatrics 162, 844–849 (2000).
Wapner, R. J. Antenatal corticosteroids for periviable birth. Semin. Perinatol. 37, 410–413 (2013).
Kawai, M. Late‐onset circulatory collapse of prematurity. Pediatr. Int. 59, 391–396 (2017).
Ng, P. C. et al. Transient adrenocortical insufficiency of prematurity and systemic hypotension in very low birthweight infants. Arch. Dis. Child. Fetal Neonatal Ed. 89, F119–F126 (2004).
Davis, E. P. et al. Antenatal betamethasone treatment has a persisting influence on infant HPA axis regulation. J. Perinatol. 26, 147–153 (2006).
Yasuoka, K. et al. Late-onset circulatory collapse and risk of cerebral palsy in extremely preterm infants. J. Pediatr. 212, 117–123 (2019).
Nakanishi, H. et al. Clinical characterization and long-term prognosis of neurological development in preterm infants with late-onset circulatory collapse. J. Perinatol. 30, 751–756 (2010).
Shimokaze, T., Akaba, K. & Saito, E. Late-onset glucocorticoid-responsive circulatory collapse in preterm infants: clinical characteristics of 14 patients. Tohoku J. Exp. Med. 235, 241–248 (2015).
Iijima, S. Late-onset glucocorticoid-responsive circulatory collapse in premature infants. Pediatr. Neonatol. 60, 603–610 (2019).
Koyama, N. et al. Clinical features of late-onset circulatory dysfunction in premature infants. Res. Rep. Neonatol. 4, 139 (2014).
Suzuki, Y. et al. Neonatal factors related to center variation in the incidence of late-onset circulatory collapse in extremely preterm infants. PLoS ONE 13, e0198518 (2018).
Waffarn, F. & Davis, E. P. Effects of antenatal corticosteroids on the hypothalamic-pituitary-adrenocortical axis of the fetus and newborn: experimental findings and clinical considerations. Am. J. Obstet. Gynecol. 207, 446–454 (2012).
Tegethoff, M., Pryce, C. & Meinlschmidt, G. Effects of intrauterine exposure to synthetic glucocorticoids on fetal, newborn, and infant hypothalamic-pituitary-adrenal axis function in humans: a systematic review. Endocr. Rev. 30, 753–789 (2009).
Niwa, F. et al. Limited response to CRH stimulation tests at 2 weeks of age in preterm infants born at less than 30 weeks of gestational age. Clin. Endocrinol. 78, 724–729 (2013).
Acknowledgements
We thank the University of Nebraska Medical Center for funding this research.
Consent
Patient consent was not required for this study.
Author information
Authors and Affiliations
Contributions
E.S.P. contributed to study design, data interpretation, and provided critical revisions to the final manuscript. K.C.M. conducted the literature search and data collection and contributed to the study design, data interpretation, and writing of the final manuscript. E.R.L. contributed to the data analysis and interpretation and provided critical revisions to the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Marinelli, K.C., Lyden, E.R. & Peeples, E.S. Clinical risk factors for the development of late-onset circulatory collapse in premature infants. Pediatr Res 89, 968–973 (2021). https://doi.org/10.1038/s41390-020-0990-7
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-020-0990-7
This article is cited by
-
Total hydrocortisone dosage in extremely low birth weight infants and neurodevelopment up to school age
Pediatric Research (2025)
-
Use of hydrocortisone in extremely preterm infants: emphasis on those born least mature
Journal of Perinatology (2025)
-
Presumed adrenal insufficiency in neonates treated with corticosteroids for the prevention of bronchopulmonary dysplasia
Journal of Perinatology (2022)