Abstract
Numerous studies have examined the potential use of therapeutic gases for the treatment of various neurological disorders. Hydrogen gas, a promising neuroprotective agent, has been a focus of study due to its potent antioxidative properties. In translational research into adult diseases, hydrogen has been shown to be neuroprotective in disorders such as cerebral ischemia and traumatic brain injury, and in neurodegenerative diseases such as Alzheimer’s disease. Animal and human studies have verified the safety and feasibility of molecular hydrogen. However, despite extensive research on its efficacy in adults, only a few studies have investigated its application in pediatric and neonatal medicine. Neonatal hypoxic–ischemic encephalopathy (HIE) is characterized by damage to neurons and other cells of the nervous system. One of the major contributing factors is excessive exposure to oxidative stress. Current research interest in HIE is shifting toward new neuroprotective agents, as single agents or as adjuncts to therapeutic hypothermia. Here, we review therapeutic gases, particularly hydrogen, and their potentials and limitations in the treatment of HIE in newborns.
Impact
-
Translational animal models of neonatal HIE are a current focus of research into the therapeutic usefulness of various gases.
-
Hydrogen ventilation as a single agent or in combination with therapeutic hypothermia shows short- and long-term neuroprotection in neonatal translational HIE models.
-
The optimal target severity for therapeutic interventions should be well established to improve outcomes.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Kajimura, M. et al. Gas biology: tiny molecules controlling metabolic systems. Respir. Physiol. Neurobiol. 184, 139–148 (2012).
Ohsawa, I. et al. Hydrogen acts as a therapeutic antioxidant by selectively reducing cytotoxic oxygen radicals. Nat. Med. 13, 688–694 (2007).
Volpe, J. J. Neurology of the Newborn 6th edn (Elsevier, 2018).
Kriz, J. Inflammation in ischemic brain injury: timing is important. Crit. Rev. Neurobiol. 18, 145–157 (2006).
Hassell, K. J., Ezzati, M., Alonso-Alconada, D., Hausenloy, D. J. & Robertson, N. J. New horizons for newborn brain protection: enhancing endogenous neuroprotection. Arch. Dis. Child Fetal Neonatal Ed. 100, F541–F552 (2015).
Robles, R., Palomino, N. & Robles, A. Oxidative stress in the neonate. Early Hum. Dev. 65(Suppl.), S75–S81 (2001).
Ferriero, D. M. Neonatal brain injury. N. Engl. J. Med. 351, 1985–1995 (2004).
Forman, H. J., Maiorino, M. & Ursini, F. Signaling functions of reactive oxygen species. Biochemistry 49, 835–842 (2010).
Bauer, G. Signaling and proapoptotic functions of transformed cell-derived reactive oxygen species. Prostaglandins Leukot. Essent. Fatty Acids 66, 41–56 (2002).
Gunn, A. J. et al. Therapeutic hypothermia translates from ancient history in to practice. Pediatr. Res. 81, 202–209 (2017).
Hill, A. Pharmacologic considerations in the management of the asphyxiated newborn. Clin. Invest. Med. 8, 355–359 (1985).
Palmer, C. & Vannucci, R. C. Potential new therapies for perinatal cerebral hypoxia–ischemia. Clin. Perinatol. 20, 411–432 (1993).
Jiang, J. Y., Liang, Y. M., Luo, Q. Z. & Zhu, C. Effect of mild hypothermia on brain dialysate lactate after fluid percussion brain injury in rodents. Neurosurgery 54, 713–717 (2004). discussion 717–718.
Erecinska, M., Thoresen, M. & Silver, I. A. Effects of hypothermia on energy metabolism in Mammalian central nervous system. J. Cereb. Blood Flow Metab. 23, 513–530 (2003).
Hagerdal, M., Harp, J., Nilsson, L. & Siesjo, B. K. The effect of induced hypothermia upon oxygen consumption in the rat brain. J. Neurochem. 24, 311–316 (1975).
Kvrivishvili, G. Glycine and neuroprotective effect of hypothermia in hypoxic–ischemic brain damage. NeuroReport 13, 1995–2000 (2002).
Xiong, M., Yang, Y., Chen, G. Q. & Zhou, W. H. Post-ischemic hypothermia for 24h in P7 rats rescues hippocampal neuron: association with decreased astrocyte activation and inflammatory cytokine expression. Brain Res. Bull. 79, 351–357 (2009).
Edwards, A. D. et al. Specific inhibition of apoptosis after cerebral hypoxia–ischaemia by moderate post-insult hypothermia. Biochem. Biophys. Res. Commun. 217, 1193–1199 (1995).
Ohmura, A. et al. Prolonged hypothermia protects neonatal rat brain against hypoxic–ischemia by reducing both apoptosis and necrosis. Brain Dev. 27, 517–526 (2005).
Hasegawa, M., Ogihara, T., Tamai, H. & Hiroi, M. Hypothermic inhibition of apoptotic pathways for combined neurotoxicity of iron and ascorbic acid in differentiated PC12 cells: reduction of oxidative stress and maintenance of the glutathione redox state. Brain Res. 1283, 1–13 (2009).
Truettner, J. S., Alonso, O. F. & Dietrich, W. D. Influence of therapeutic hypothermia on matrix metalloproteinase activity after traumatic brain injury in rats. J. Cereb. Blood Flow Metab. 25, 1505–1516 (2005).
Edwards, A. D. et al. Neurological outcomes at 18 months of age after moderate hypothermia for perinatal hypoxic ischaemic encephalopathy: synthesis and meta-analysis of trial data. BMJ 340, c363 (2010).
Jacobs, S. E. et al. Cooling for newborns with hypoxic–ischaemic encephalopathy. Cochrane Database Syst. Rev. CD003311, https://doi.org/10.1002/14651858.CD003311.pub3 (2013).
Low, E. et al. Cooling and seizure burden in term neonates: an observational study. Arch. Dis. Child Fetal Neonatal Ed. 97, F267–F272 (2012).
Azzopardi, D. et al. Effects of hypothermia for perinatal asphyxia on childhood outcomes. N. Engl. J. Med. 371, 140–149 (2014).
Guillet, R. et al. Seven- to eight-year follow-up of the CoolCap trial of head cooling for neonatal encephalopathy. Pediatr. Res. 71, 205–209 (2012).
Ohta, S. Molecular hydrogen is a novel antioxidant to efficiently reduce oxidative stress with potential for the improvement of mitochondrial diseases. Biochim. Biophys. Acta 1820, 586–594 (2012).
Gardette, B. & Delauze, H. G. Techniques of underwater intervention: means, methods, research and outlook. Bull. Acad. Natl Med. 180, 975–983 (1996).
Ichihara, M. et al. Beneficial biological effects and the underlying mechanisms of molecular hydrogen—comprehensive review of 321 original articles. Med. Gas Res. 5, 12 (2015).
Ohta, S. Molecular hydrogen as a preventive and therapeutic medical gas: initiation, development and potential of hydrogen medicine. Pharm. Ther. 144, 1–11 (2014).
Tamura, T., Hayashida, K., Sano, M., Onuki, S. & Suzuki, M. Efficacy of inhaled HYdrogen on neurological outcome following BRain Ischemia During post-cardiac arrest care (HYBRID II trial): study protocol for a randomized controlled trial. Trials 18, 488 (2017).
Ono, H. et al. A basic study on molecular hydrogen (H2) inhalation in acute cerebral ischemia patients for safety check with physiological parameters and measurement of blood H2 level. Med. Gas Res. 2, 21 (2012).
Rice, J. E. 3rd, Vannucci, R. C. & Brierley, J. B. The influence of immaturity on hypoxic–ischemic brain damage in the rat. Ann. Neurol. 9, 131–141 (1981).
Lingam, I., Avdic-Belltheus, A. & Robertson, N. J. Using animal models to improve care of neonatal encephalopathy. Arch. Dis. Child Educ. Pract. Ed. 101, 271–276 (2016).
Thornton, C., Baburamani, A. A., Kichev, A. & Hagberg, H. Oxidative stress and endoplasmic reticulum (ER) stress in the development of neonatal hypoxic–ischaemic brain injury. Biochem. Soc. Trans. 45, 1067–1076 (2017).
Koehler, R. C., Yang, Z. J., Lee, J. K. & Martin, L. J. Perinatal hypoxic–ischemic brain injury in large animal models: relevance to human neonatal encephalopathy. J. Cereb. Blood Flow Metab. 38, 2092–2111 (2018).
Cai, J. et al. Hydrogen therapy reduces apoptosis in neonatal hypoxia–ischemia rat model. Neurosci. Lett. 441, 167–172 (2008).
Matchett, G. A. et al. Hydrogen gas is ineffective in moderate and severe neonatal hypoxia–ischemia rat models. Brain Res. 1259, 90–97 (2009).
Dobbing, J. & Sands, J. Comparative aspects of the brain growth spurt. Early Hum. Dev. 3, 79–83 (1979).
Kusaka, T. et al. Relationship between cerebral oxygenation and phosphorylation potential during secondary energy failure in hypoxic–ischemic newborn piglets. Pediatr. Res. 65, 317–322 (2009).
Cady, E. B., Iwata, O., Bainbridge, A., Wyatt, J. S. & Robertson, N. J. Phosphorus magnetic resonance spectroscopy 2 h after perinatal cerebral hypoxia–ischemia prognosticates outcome in the newborn piglet. J. Neurochem. 107, 1027–1035 (2008).
Iwata, O. et al. Supra- and sub-baseline phosphocreatine recovery in developing brain after transient hypoxia–ischaemia: relation to baseline energetics, insult severity and outcome. Brain 131, 2220–2226 (2008).
Moroz, T., Banaji, M., Robertson, N. J., Cooper, C. E. & Tachtsidis, I. Computational modelling of the piglet brain to simulate near-infrared spectroscopy and magnetic resonance spectroscopy data collected during oxygen deprivation. J. R. Soc. Interface 9, 1499–1509 (2012).
Moroz, T. et al. Modelling blood flow and metabolism in the piglet brain during hypoxia–ischaemia: simulating brain energetics. Adv. Exp. Med. Biol. 789, 339–344 (2013).
Robertson, N. J. et al. Methyl-isobutyl amiloride reduces brain Lac/NAA, cell death and microglial activation in a perinatal asphyxia model. J. Neurochem. 124, 645–657 (2013).
Bainbridge, A. et al. Brain mitochondrial oxidative metabolism during and after cerebral hypoxia–ischemia studied by simultaneous phosphorus magnetic-resonance and broadband near-infrared spectroscopy. Neuroimage 102(Part 1), 173–183 (2014).
Martin, L. J., Brambrink, A., Koehler, R. C. & Traystman, R. J. Primary sensory and forebrain motor systems in the newborn brain are preferentially damaged by hypoxia–ischemia. J. Comp. Neurol. 377, 262–285 (1997).
Tooley, J. R., Satas, S., Porter, H., Silver, I. A. & Thoresen, M. Head cooling with mild systemic hypothermia in anesthetized piglets is neuroprotective. Ann. Neurol. 53, 65–72 (2003).
Alderliesten, T. et al. Neuroprotection by argon ventilation after perinatal asphyxia: a safety study in newborn piglets. PLoS ONE 9, e113575 (2014).
Chakkarapani, E. et al. A closed-circuit neonatal xenon delivery system: a technical and practical neuroprotection feasibility study in newborn pigs. Anesth. Analg. 109, 451–460 (2009).
Chakkarapani, E., Thoresen, M., Liu, X., Walloe, L. & Dingley, J. Xenon offers stable haemodynamics independent of induced hypothermia after hypoxia–ischaemia in newborn pigs. Intens. Care Med. 38, 316–323 (2012).
Faulkner, S. et al. Xenon augmented hypothermia reduces early lactate/N-acetylaspartate and cell death in perinatal asphyxia. Ann. Neurol. 70, 133–150 (2011).
Faulkner, S. D. et al. A xenon recirculating ventilator for the newborn piglet: developing clinical applications of xenon for neonates. Eur. J. Anaesthesiol. 29, 577–585 (2012).
Foster, K. A. et al. An improved survival model of hypoxia/ischaemia in the piglet suitable for neuroprotection studies. Brain Res. 919, 122–131 (2001).
Domoki, F. et al. Hydrogen is neuroprotective and preserves cerebrovascular reactivity in asphyxiated newborn pigs. Pediatr. Res. 68, 387–392 (2010).
Varga, V. et al. Molecular hydrogen alleviates asphyxia-induced neuronal cyclooxygenase-2 expression in newborn pigs. Acta Pharm. Sin. 39, 1273–1283 (2018).
Nemeth, J. et al. Molecular hydrogen affords neuroprotection in a translational piglet model of hypoxic–ischemic encephalopathy. J. Physiol. Pharm. 67, 677–689 (2016).
Olah, O., Toth-Szuki, V., Temesvari, P., Bari, F. & Domoki, F. Delayed neurovascular dysfunction is alleviated by hydrogen in asphyxiated newborn pigs. Neonatology 104, 79–86 (2013).
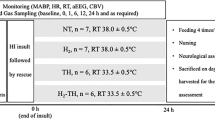
Htun, Y. et al. Hydrogen ventilation combined with mild hypothermia improves short-term neurological outcomes in a 5-day neonatal hypoxia–ischaemia piglet model. Sci. Rep. 9, 4088 (2019).
Thoresen, M., Simmonds, M., Satas, S., Tooley, J. & Silver, I. A. Effective selective head cooling during posthypoxic hypothermia in newborn piglets. Pediatr. Res. 49, 594–599 (2001).
Purushothuman, S. & Stone, J. The reaction of cerebral cortex to a nearby lesion: damage, survival, self-protection. Brain Res. 1601, 52–63 (2015).
Won, M. H. et al. The alterations of N-methyl-d-aspartate receptor expressions and oxidative DNA damage in the CA1 area at the early time after ischemia–reperfusion insult. Neurosci. Lett. 301, 139–142 (2001).
Tao, G., Song, G. & Qin, S. Molecular hydrogen: current knowledge on mechanism in alleviating free radical damage and diseases. Acta Biochim. Biophys. Sin. (Shanghai) 51, 1189–1197 (2019).
Huang, Y. et al. Beneficial effects of hydrogen gas against spinal cord ischemia-reperfusion injury in rabbits. Brain Res. 1378, 125–136 (2011).
Xin, H. G. et al. Consumption of hydrogen-rich water alleviates renal injury in spontaneous hypertensive rats. Mol. Cell. Biochem. 392, 117–124 (2014).
Shi, Q. et al. Hydrogen-rich saline attenuates acute renal injury in sodium taurocholate-induced severe acute pancreatitis by inhibiting ROS and NF-kappaB pathway. Mediat. Inflamm. 2015, 685043 (2015).
Song, G. et al. Molecular hydrogen stabilizes atherosclerotic plaque in low-density lipoprotein receptor-knockout mice. Free Radic. Biol. Med. 87, 58–68 (2015).
Gold, R. et al. Placebo-controlled phase 3 study of oral BG-12 for relapsing multiple sclerosis. N. Engl. J. Med. 367, 1098–1107 (2012).
Ma, Q. Role of nrf2 in oxidative stress and toxicity. Annu. Rev. Pharm. Toxicol. 53, 401–426 (2013).
Liu, L. et al. Inhalation of hydrogen gas attenuates brain injury in mice with cecal ligation and puncture via inhibiting neuroinflammation, oxidative stress and neuronal apoptosis. Brain Res. 1589, 78–92 (2014).
Gharib, B. et al. Anti-inflammatory properties of molecular hydrogen: investigation on parasite-induced liver inflammation. C. R. Acad. Sci. III 324, 719–724 (2001).
Tian, Y. et al. Effects of hydrogen-rich saline on hepatectomy-induced postoperative cognitive dysfunction in old mice. Mol. Neurobiol. 54, 2579–2584 (2017).
Shao, A. et al. Hydrogen-rich saline attenuated subarachnoid hemorrhage-induced early brain injury in rats by suppressing inflammatory response: possible involvement of NF-kappaB pathway and NLRP3 pnflammasome. Mol. Neurobiol. 53, 3462–3476 (2016).
Zhang, G. et al. The anti-inflammatory effect of hydrogen on lung transplantation model of pulmonary microvascular endothelial cells during cold storage period. Transplantation 102, 1253–1261 (2018).
Chen, L. et al. Hydrogen treatment protects mice against chronic pancreatitis by restoring regulatory T cells loss. Cell. Physiol. Biochem. 44, 2005–2016 (2017).
Lin, C. P., Chuang, W. C., Lu, F. J. & Chen, C. Y. Anti-oxidant and anti-inflammatory effects of hydrogen-rich water alleviate ethanol-induced fatty liver in mice. World J. Gastroenterol. 23, 4920–4934 (2017).
Iuchi, K. et al. Molecular hydrogen regulates gene expression by modifying the free radical chain reaction-dependent generation of oxidized phospholipid mediators. Sci. Rep. 6, 18971 (2016).
Jiang, X. et al. FoxO1-mediated autophagy plays an important role in the neuroprotective effects of hydrogen in a rat model of vascular dementia. Behav. Brain Res. 356, 98–106 (2019).
Gao, Y. et al. Hydrogen gas attenuates myocardial ischemia–reperfusion injury independent of postconditioning in rats by attenuating endoplasmic reticulum stress-induced autophagy. Cell. Physiol. Biochem. 43, 1503–1514 (2017).
Ishibashi, T. Therapeutic efficacy of molecular hydrogen: a new mechanistic insight. Curr. Pharm. Des. 25, 946–955 (2019).
Yoritaka, A. et al. Pilot study of H(2) therapy in Parkinson’s disease: a randomized double-blind placebo-controlled trial. Mov. Disord. 28, 836–839 (2013).
Sakai, T. et al. Consumption of water containing over 3.5 mg of dissolved hydrogen could improve vascular endothelial function. Vasc. Health Risk Manag. 10, 591–597 (2014).
Hayashida, K. et al. Inhalation of hydrogen gas reduces infarct size in the rat model of myocardial ischemia–reperfusion injury. Biochem. Biophys. Res. Commun. 373, 30–35 (2008).
Yamamoto, R., Homma, K., Suzuki, S., Sano, M. & Sasaki, J. Hydrogen gas distribution in organs after inhalation: real-time monitoring of tissue hydrogen concentration in rat. Sci. Rep. 9, 1255 (2019).
Rossaint, R. et al. Multicenter randomized comparison of the efficacy and safety of xenon and isoflurane in patients undergoing elective surgery. Anesthesiology 98, 6–13 (2003).
Cullen, S. C. & Gross, E. G. The anesthetic properties of xenon in animals and human beings, with additional observations on krypton. Science 113, 580–582 (1951).
Cullen, S. C. & Pittinger, C. B. Clinical and laboratory observations of the use of xenon for anesthesia. Surg. Forum. 38th Congress 361–366 (1953).
Franks, N. P., Dickinson, R., de Sousa, S. L., Hall, A. C. & Lieb, W. R. How does xenon produce anaesthesia? Nature 396, 324 (1998).
Petzelt, C. P., Kodirov, S., Taschenberger, G. & Kox, W. J. Participation of the Ca(2+)-calmodulin-activated Kinase II in the control of metaphase–anaphase transition in human cells. Cell Biol. Int. 25, 403–409 (2001).
Ma, D. et al. Xenon preconditioning reduces brain damage from neonatal asphyxia in rats. J. Cereb. Blood Flow Metab. 26, 199–208 (2006).
Dingley, J., Tooley, J., Porter, H. & Thoresen, M. Xenon provides short-term neuroprotection in neonatal rats when administered after hypoxia–ischemia. Stroke 37, 501–506 (2006).
Dingley, J., Hobbs, C., Ferguson, J., Stone, J. & Thoresen, M. Xenon/hypothermia neuroprotection regimes in spontaneously breathing neonatal rats after hypoxic–ischemic insult: the respiratory and sedative effects. Anesth. Analg. 106, 916–923 (2008), table of contents.
Liu, X., Dingley, J., Scull-Brown, E. & Thoresen, M. Adding 5 h delayed xenon to delayed hypothermia treatment improves long-term function in neonatal rats surviving to adulthood. Pediatr. Res. 77, 779–783 (2015).
Thoresen, M., Hobbs, C. E., Wood, T., Chakkarapani, E. & Dingley, J. Cooling combined with immediate or delayed xenon inhalation provides equivalent long-term neuroprotection after neonatal hypoxia-ischemia. J. Cereb. Blood Flow Metab. 29, 707–714 (2009).
Hobbs, C. et al. Xenon and hypothermia combine additively, offering long-term functional and histopathologic neuroprotection after neonatal hypoxia/ischemia. Stroke 39, 1307–1313 (2008).
Sabir, H., Osredkar, D., Maes, E., Wood, T. & Thoresen, M. Xenon combined with therapeutic hypothermia is not neuroprotective after severe hypoxia–ischemia in neonatal rats. PLoS ONE 11, e0156759 (2016).
Chakkarapani, E. et al. Xenon enhances hypothermic neuroprotection in asphyxiated newborn pigs. Ann. Neurol. 68, 330–341 (2010).
Dingley, J. et al. Xenon ventilation during therapeutic hypothermia in neonatal encephalopathy: a feasibility study. Pediatrics 133, 809–818 (2014).
Ruegger, C. M., Davis, P. G. & Cheong, J. L. Xenon as an adjuvant to therapeutic hypothermia in near-term and term newborns with hypoxic–ischaemic encephalopathy. Cochrane Database Syst. Rev. 8, CD012753 (2018).
Hollig, A. et al. Argon: systematic review on neuro- and organoprotective properties of an “inert” gas. Int. J. Mol. Sci. 15, 18175–18196 (2014).
Loetscher, P. D. et al. Argon: neuroprotection in in vitro models of cerebral ischemia and traumatic brain injury. Crit. Care 13, R206 (2009).
Broad, K. D. et al. Inhaled 45–50% argon augments hypothermic brain protection in a piglet model of perinatal asphyxia. Neurobiol. Dis. 87, 29–38 (2016).
Koziakova, M. et al. Noble gas neuroprotection: xenon and argon protect against hypoxic–ischaemic injury in rat hippocampus in vitro via distinct mechanisms. Br. J. Anaesth. 123, 601–609 (2019).
Ben-Ari, Y., Khalilov, I., Kahle, K. T. & Cherubini, E. The GABA excitatory/inhibitory shift in brain maturation and neurological disorders. Neuroscientist 18, 467–486 (2012).
Katz, I., Murdock, J., Palgen, M., Pype, J. & Caillibotte, G. Pharmacokinetic analysis of the chronic administration of the inert gases Xe and Ar using a physiological based model. Med. Gas Res. 5, 8 (2015).
Sabir, H. et al. Xenon depresses aEEG background voltage activity whilst maintaining cardiovascular stability in sedated healthy newborn pigs. J. Neurol. Sci. 363, 140–144 (2016).
Amer, A. R. & Oorschot, D. E. Xenon combined with hypothermia in perinatal hypoxic–ischemic encephalopathy: a noble gas, a noble mission. Pediatr. Neurol. 84, 5–10 (2018).
Acknowledgements
This study was financially supported by Grants-in-Aid for Scientific Research (KAKENHI) from the Japan Society for the Promotion of Science (number 16K10092 to T.K., and numbers 19K08253, 16H06276, 16K19685, and 15KK0311 to S.N.), grants from the Kagawa University Faculty of Medicine School of Medicine Alumni Association Sanjukai Research Aid (numbers R1-1 and 25-2), and a scholarship from the Honjo International Scholarship Foundation (to Y.H.).
Author information
Authors and Affiliations
Contributions
Y.H. and T.K. designed the study and drafted the article. Y.H., S.N., and T.K. revised it critically and contributed to the final approval of the version to be published.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Htun, Y., Nakamura, S. & Kusaka, T. Hydrogen and therapeutic gases for neonatal hypoxic–ischemic encephalopathy: potential neuroprotective adjuncts in translational research. Pediatr Res 89, 753–759 (2021). https://doi.org/10.1038/s41390-020-0998-z
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-020-0998-z
This article is cited by
-
Hypoxic-Ischemic Encephalopathy: Pathogenesis and Promising Therapies
Molecular Neurobiology (2025)
-
Hydrogen gas can ameliorate seizure burden during therapeutic hypothermia in asphyxiated newborn piglets
Pediatric Research (2024)
-
Impact of hydrogen gas inhalation during therapeutic hypothermia on cerebral hemodynamics and oxygenation in the asphyxiated piglet
Scientific Reports (2023)
-
Conflicting findings on the effectiveness of hydrogen therapy for ameliorating vascular leakage in a 5-day post hypoxic-ischemic survival piglet model
Scientific Reports (2023)
-
Molecular Hydrogen: an Emerging Therapeutic Medical Gas for Brain Disorders
Molecular Neurobiology (2023)