Abstract
Background
Mechanisms of chemotherapy-associated neurotoxicity are poorly understood, and therefore, prevention strategies have not been developed. We hypothesized that a subgroup of children receiving intrathecal cytarabine develops subclinical vasospasm, which may contribute to long-term neurocognitive sequelae of cancer.
Methods
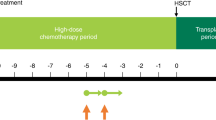
We used transcranial Doppler ultrasound to serially evaluate cerebral blood flow velocities in participants ≤25 years old receiving intrathecal cytarabine for hematologic malignancies.
Results
Four of 18 participants (22%) met the criteria for subclinical vasospasm within 4 days of intrathecal cytarabine administration. The distribution of oncologic diagnoses differed between the vasospasm and non-vasospasm groups (p = 0.02). Acute myeloid leukemia was identified as a potential risk factor for vasospasm. Children with vasospasm were more likely to have received intravenous cytarabine (75% versus 0%, p = 0.01) and less likely to have received steroids (25% versus 100%, p = 0.01).
Conclusions
A subpopulation of children with hematologic malignancies develops subclinical vasospasm after intrathecal cytarabine treatment. Future research is needed to determine the long-term clinical consequences of cerebral vasospasm in this population.
Impact
-
A subset of children with hematologic malignancies who receive intrathecal cytarabine experience subclinical cerebral vasospasm, as measured by transcranial Doppler ultrasound.
-
Of children receiving intrathecal cytarabine, those who develop cerebral vasospasm are more likely to have diagnosis of acute myeloid leukemia, more likely to receive concurrent intravenous cytarabine, and less likely to receive steroids as part of their chemotherapy regimen, as compared with children without vasospasm.
-
Future research is needed to determine if vasospasm during chemotherapy is associated with higher rates of neurocognitive dysfunction, and if so, to focus on prevention of these long-term sequelae of childhood cancer.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Bright, C. et al. Risk of cerebrovascular events in 178 962 five-year survivors of cancer diagnosed at 15 to 39 years of age: The TYACSS (teenage and young adult cancer survivor study). Circulation 135, 1194–1210 (2017).
Armstrong, C. & Sun, L. R. Neurological complications of pediatric cancer. Cancer Metastasis Rev. https://doi.org/10.1007/s10555-020-09847-0 (2020).
Sun, L. R. & Cooper, S. Neurological complications of the treatment of pediatric neoplastic disorders. Pediatr. Neurol. 85, 33–42 (2018).
Baker, W. J., Royer, G. L. & Weiss, R. B. Cytarabine and neurologic toxicity. J. Clin. Oncol. 9, 679–693 (1991).
Resar, L. M. S. et al. Acute neurotoxicity after intrathecal cytosine arabinoside in two adolescents with acute lymphoblastic leukemia of B‐cell type. Cancer 71, 117–123 (1993).
Openshaw, H., Slatkin, N. E., Stein, A. S., Hinton, D. R. & Forman, S. J. Acute polyneuropathy after high dose cytosine arabinoside in patients with leukemia. Cancer 78, 1899–1905 (1996).
Saito, T. et al. Peripheral neuropathy caused by high-dose cytosine arabinoside treatment in a patient with acute myeloid leukemia. J. Infect. Chemother. 12, 148–151 (2006).
Werner, R. A. Paraplegia and quadriplegia after intrathecal chemotherapy. Arch. Phys. Med. Rehabil. 69, 1054 (1988).
Tibussek, D. et al. Severe cerebral vasospasm and childhood arterial ischemic stroke after intrathecal cytarabine. Pediatrics 137, e20152143 (2016).
Pound, C. M., Keene, D. L., Udjus, K., Humphreys, P. & Johnston, D. L. Acute encephalopathy and cerebral vasospasm after multiagent chemotherapy including PEG-asparaginase and intrathecal cytarabine for the treatment of acute lymphoblastic leukemia. J. Pediatr. Hematol. Oncol. 29, 183–186 (2007).
Yoon, J. H. et al. Diffuse cerebral vasospasm with infarct after intrathecal cytarabine in childhood leukemia. Pediatr. Int. 56, 921–924 (2014).
Hiraide, T. et al. Recurrent posterior reversible encephalopathy due to vasospasm and cerebral hypoperfusion in in acute leukemia: a case report. No. To. Hattatsu. 47, 449 (2015).
Henderson, R. D., Rajah, T., Nicol, A. J. & Read, S. J. Posterior leukoencephalopathy following intrathecal chemotherapy with MRA-documented vasospasm. Neurology 60, 326–328 (2003).
Saito, B. et al. Reversible posterior leukoencephalopathy syndrome after repeat intermediate-dose cytarabine chemotherapy in a patient with acute myeloid leukemia. Am. J. Hematol. 82, 304–306 (2007).
Cheung, Y. T. & Krull, K. R. Neurocognitive outcomes in long-term survivors of childhood acute lymphoblastic leukemia treated on contemporary treatment protocols: a systematic review. Neurosci. Biobehav. Rev. 53, 108–120 (2015).
Stenhouse, L. M., Knight, R. G., Longmore, B. E. & Bishara, S. N. Long-term cognitive deficits in patients after surgery on aneurysms of the anterior communicating artery. J. Neurol. Neurosurg. Psychiatry 54, 909–914 (1991).
Richardson, J. T. E. Cognitive performance following rupture and repair of intracranial aneurysm. Acta Neurol. Scand. 83, 110–122 (1991).
Kreiter, K. T. et al. Predictors of cognitive dysfunction after subarachnoid hemorrhage. Stroke 33, 200–209 (2002).
Lee, J. H. et al. Hemodynamically significant cerebral vasospasm and outcome after head injury: a prospective study. J. Neurosurg. 87, 221–233 (1997).
Bartzokis, G. et al. Magnetic resonance imaging evidence of “silent” cerebrovascular toxicity in cocaine dependence. Biol. Psychiatry 45, 1203–1211 (1999).
Bode, H. & Wais, U. Age dependence of flow velocities in basal cerebral arteries. Arch. Dis. Child. 63, 606–611 (1988).
Alsdorf, W. H. et al. Severe and irreversible myelopathy after concurrent systemic and intrathecal nucleoside analogue treatment for refractory diffuse large B-cell lymphoma: a case report and review of the literature. J. Oncol. Pharm. Pract. 22, 523–527 (2016).
Hwang, T. L., Yung, W. K., Lee, Y. Y., Borit, A. & Fields, W. S. High dose ara-C related leukoencephalopathy. J. Neurooncol. 3, 335–339 (1986).
Slevin, M. L. et al. Effect of dose and schedule on pharmacokinetics of high-dose cytosine arabinoside in plasma and cerebrospinal fluid. J. Clin. Oncol. 1, 546–551 (1983).
Honkaniemi, J. et al. Reversible posterior leukoencephalopathy after combination chemotherapy. Neuroradiology 42, 895–899 (2000).
Ghali, M. G. Z., Davanzo, J., Leo, M. & Rizk, E. Posterior reversible encephalopathy syndrome in pediatric patients: pathophysiology, diagnosis, and management. Leuk. Lymphoma 60, 2365–2372 (2019).
Lindegaard, K. F., Nornes, H., Bakke, S. J., Sorteberg, W. & Nakstad, P. Cerebral vasospasm diagnosis by means of angiography and blood velocity measurements. Acta Neurochir. 100, 12–24 (1989).
Kirsch, J. D., Mathur, M., Johnson, M. H., Gowthaman, G. & Scoutt, L. M. Advances in transcranial doppler US: imaging ahead. Radiographics 33, E1–E14 (2013).
Tzeng, Y. C. et al. Cerebrovascular regulation during transient hypotension and hypertension in humans. Hypertension 56, 268–273 (2010).
Doering, T. J., Brix, J., Schneider, B. & Rimpler, M. Cerebral hemodynamics and cerebral metabolism during cold and warm stress. Am. J. Phys. Med. Rehabil. 75, 408–415 (1996).
Bisschops, L. L., van der Hoeven, J. G. & Hoedemaekers, C. W. Effects of prolonged mild hypothermia on cerebral blood flow after cardiac arrest. Crit. Care Med. 40, 2362–2367 (2012).
DeBaun, M. R. et al. Silent cerebral infarcts: a review on a prevalent and progressive cause of neurologic injury in sickle cell anemia. Blood 119, 4587–4596 (2012).
O’Brien, N., Maa, T. & Yeates, K. The epidemiology of vasospasm in children with moderate-to-severe traumatic brain injury. Crit. Care Med. 43, 674–685 (2015).
Croal, P. L. et al. Assessment of cerebral blood flow with magnetic resonance imaging in children with sickle cell disease: a quantitative comparison with transcranial doppler ultrasonography. Brain Behav. 7, e00811 (2017).
Acknowledgements
The authors would like to thank Bobby Ergin and Vladimir Ponomarev for their technical assistance. This study was funded by the Thrasher Research Fund.
Author information
Authors and Affiliations
Contributions
L.R.S. conceived of and designed the study. L.R.S., W.Z., P.B., and A.G.T. acquired the data. L.R.S., W.Z., P.B., S.C., R.F.G., and R.J.F. analyzed and interpreted the data. L.R.S. drafted the manuscript. L.R.S., W.Z., P.B., R.F.G., and R.J.F. critically revised the manuscript of important intellectual content. L.R.S., W.Z., P.B., A.G.T., S.C., R.F.G., and R.J.F. approved of the final version to be published.
Corresponding author
Ethics declarations
Competing interests
R.F.G. is an associate editor for Neurology; otherwise, we have no relevant conflicts of interest or disclosures to report.
Consent and approval
This study was approved by the institutional review board. All families signed informed consent, and all children 7 years of age or older gave verbal assent.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sun, L.R., Ziai, W., Brown, P. et al. Intrathecal chemotherapy-associated cerebral vasospasm in children with hematologic malignancies. Pediatr Res 89, 858–862 (2021). https://doi.org/10.1038/s41390-020-1008-1
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-020-1008-1
This article is cited by
-
Clinical Applications of Point-of-Care and Diagnostic Transcranial Doppler in the Pediatric Acute Care Setting: A Scoping Review
Neurocritical Care (2025)
-
Establishing normal Lindegaard Ratio in healthy children 10–16 years of age
Child's Nervous System (2024)
-
Neuromonitoring in Children with Cerebrovascular Disorders
Neurocritical Care (2023)
-
Cytarabine
Reactions Weekly (2021)