Abstract
Background
The impact of human milk use on racial/ethnic disparities in necrotizing enterocolitis (NEC) incidence is unknown.
Methods
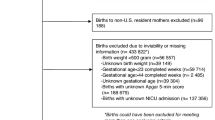
Trends in NEC incidence and human milk use at discharge were evaluated by race/ethnicity among 47,112 very low birth weight infants born in California from 2008 to 2017. We interrogated the association between race/ethnicity and NEC using multilevel regression analysis, and evaluated the effect of human milk use at discharge on the relationship between race/ethnicity and NEC using mediation analysis.
Results
Annual NEC incidence declined across all racial/ethnic groups from an aggregate average of 4.8% in 2008 to 2.6% in 2017. Human milk use at discharge increased over the time period across all racial groups, and non-Hispanic (NH) black infants received the least human milk each year. In multivariable analyses, Hispanic ethnicity (odds ratio (OR) 1.27, 95% confidence interval (CI) 1.02–1.57) and Asian or Pacific Islander race (OR 1.35, 95% CI 1.01–1.80) were each associated with higher odds of NEC, while the association of NH black race with NEC was attenuated after adding human milk use at discharge to the model. Mediation analysis revealed that human milk use at discharge accounted for 22% of the total risk of NEC in non-white vs. white infants, and 44% in black vs. white infants.
Conclusions
Although NEC incidence has declined substantially over the past decade, a sizable racial/ethnic disparity persists. Quality improvement initiatives augmenting human milk use may further reduce the incidence of NEC in vulnerable populations.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Janevic, T. et al. Association of race/ethnicity with very preterm neonatal morbidities. JAMA Pediatr. 172, 1061–1069 (2018).
Anderson, J. G. et al. Racial and ethnic disparities in preterm infant mortality and severe morbidity: a population-based study. Neonatology 113, 44–54 (2018).
Jammeh, M. L. et al. Racial/ethnic differences in necrotizing enterocolitis incidence and outcomes in premature very low birth weight infants. J. Perinatol. 38, 1386–1390 (2018).
Wallace, M. E. et al. Racial/ethnic differences in preterm perinatal outcomes. Am. J. Obstet. Gynecol. 216, 306.e1–306.e12 (2017).
Horbar, J. D. et al. Variation in performance of neonatal intensive care units in the United States. JAMA Pediatr. 171, e164396 (2017).
Stoll, B. J. et al. Trends in care practices, morbidity, and mortality of extremely preterm neonates, 1993–2012. JAMA 314, 1039–1051 (2015).
Kamitsuka, M. D., Horton, M. K. & Williams, M. A. The incidence of necrotizing enterocolitis after introducing standardized feeding schedules for infants between 1250 and 2500 grams and less than 35 weeks of gestation. Pediatrics 105, 379–384 (2000).
Gephart, S. M. et al. NEC-zero recommendations from scoping review of evidence to prevent and foster timely recognition of necrotizing enterocolitis. Matern. Health Neonatol. Perinatol. 3, 23 (2017).
Nathan, A. T. et al. A quality improvement initiative to reduce necrotizing enterocolitis across hospital systems. J. Perinatol. 38, 742–750 (2018).
Patel, A. L. et al. Reducing necrotizing enterocolitis in very low birth weight infants using quality-improvement methods. J. Perinatol. 34, 850–857 (2014).
Alshaikh, B., Kostecky, L., Blachly, N. & Yee, W. Effect of a quality improvement project to use exclusive mother’s own milk on rate of necrotizing enterocolitis in preterm infants. Breastfeed. Med. 10, 355–361 (2015).
Gephart, S. M. & Quinn, M. C. Relationship of necrotizing enterocolitis rates to adoption of prevention practices in US neonatal intensive care units. Adv. Neonatal Care 19, 321–332 (2019).
Kantorowska, A. et al. Impact of donor milk availability on breast milk use and necrotizing enterocolitis rates. Pediatrics 137, e20153123 (2016).
Sisk, P. M., Lovelady, C. A., Dillard, R. G., Gruber, K. J. & O’Shea, T. M. Early human milk feeding is associated with a lower risk of necrotizing enterocolitis in very low birth weight infants. J. Perinatol. 27, 428–433 (2007).
Meinzen-Derr, J. et al. Role of human milk in extremely low birth weight infants’ risk of necrotizing enterocolitis or death. J. Perinatol. 29, 57–62 (2009).
Kimak, K. S., de Castro Antunes, M. M., Braga, T. D., Brandt, K. G. & de Carvalho Lima, M. Influence of enteral nutrition on occurrences of necrotizing enterocolitis in very-low-birth-weight infants. J. Pediatr. Gastroenterol. Nutr. 61, 445–450 (2015).
Cortez, J. et al. Maternal milk feedings reduce sepsis, necrotizing enterocolitis and improve outcomes of premature infants. J. Perinatol. 38, 71–74 (2018).
Pineda, R. G. Predictors of breastfeeding and breastmilk feeding among very low birth weight infants. Breastfeed. Med. 6, 15–19 (2011).
Fleurant, E. et al. Barriers to human milk feeding at discharge of very-low-birth-weight infants: maternal goal setting as a key social factor. Breastfeed. Med. 12, 20–27 (2017).
California Perinatal Quality Care Collaborative. What We Do. https://www.cpqcc.org/about/what-we-do (2018).
Gould, J. B. The role of regional collaboratives: the California Perinatal Quality Care Collaborative model. Clin. Perinatol. 37, 71–86 (2010).
Parker, M. G. et al. Racial and ethnic disparities in the use of mother’s milk feeding for very low birth weight infants in Massachusetts. J. Pediatr. 204, 134–141.e1 (2019).
Vermont Oxford Network. Improving care for infants and their families. https://public.vtoxford.org/ (2018).
American Academy of Pediatrics Committee on Fetus And Newborn. Levels of neonatal care. Pediatrics 130, 587–597 (2012).
Vermont Oxford Network. Manual of operations: part 2 data definitions & infant data forms. https://vtoxford.zendesk.com/hc/en-us (2019).
Valeri, L. & Vanderweele, T. J. Mediation analysis allowing for exposure-mediator interactions and causal interpretation: theoretical assumptions and implementation with SAS and SPSS macros. Psychol. Methods 18, 137–150 (2013).
VanderWeele, T. J. A unification of mediation and interaction: a 4-way decomposition. Epidemiology 25, 749–761 (2014).
Robins, J. M. & Greenland, S. Identifiability and exchangeability for direct and indirect effects. Epidemiology 3, 143–155 (1992).
Dietze, T. R., Rose, F. F. & Moore, T. A. Maternal variables associated with physiologic stress and perinatal complications in preterm infants. J. Neonatal Perinat. Med. 9, 271–277 (2016).
Profit, J. et al. Racial/ethnic disparity in NICU quality of care delivery. Pediatrics 140, e20170918 (2017).
Lake, E. T. et al. Disparities in perinatal quality outcomes for very low birth weight infants in neonatal intensive care. Health Serv. Res. 50, 374–397 (2015).
Lake, E. T., Staiger, D., Edwards, E. M., Smith, J. G. & Rogowski, J. A. Nursing care disparities in neonatal intensive care units. Health Serv. Res. 53(Suppl. 1), 3007–3026 (2018).
McDowell, M. M., Wang, C.-Y. & Kennedy-Stephenson, J. Breastfeeding in the United States: findings from the national health and nutrition examination surveys, 1999–2006. NCHS Data Brief. 5, 1–8 (2008).
DeFranco, E. A., Hall, E. S. & Muglia, L. J. Racial disparity in previable birth. Am. J. Obstet. Gynecol. 214, 394.e1–7 (2016).
Lee, H. C. & Gould, J. B. Factors influencing breast milk versus formula feeding at discharge for very low birth weight infants in California. J. Pediatr. 155, 657–662.e1–2 (2009).
Patel, A. L. et al. Mediators of racial and ethnic disparity in mother’s own milk feeding in very low birth weight infants. Pediatr. Res. 85, 662–670 (2019).
Riley, B. et al. Barriers to human milk feeding at discharge of very low-birthweight infants: evaluation of neighborhood structural factors. Breastfeed. Med. 11, 335–342 (2016).
Merewood, A., Brooks, D., Bauchner, H., MacAuley, L. & Mehta, S. D. Maternal birthplace and breastfeeding initiation among term and preterm infants: a statewide assessment for Massachusetts. Pediatrics 118, e1048–e1054 (2006).
Johnson, T. J., Patel, A. L., Bigger, H. R., Engstrom, J. L. & Meier, P. P. Cost savings of human milk as a strategy to reduce the incidence of necrotizing enterocolitis in very low birth weight infants. Neonatology 107, 271–276 (2015).
Howell, E. A. et al. Differences in morbidity and mortality rates in black, white, and hispanic very preterm infants among New York City Hospitals. JAMA Pediatr. 172, 269–277 (2018).
Cricco-Lizza, R. Black non-Hispanic mothers’ perceptions about the promotion of infant-feeding methods by nurses and physicians. J. Obstet. Gynecol. Neonatal Nurs. 35, 173–180 (2006).
Sigurdson, K., Morton, C., Mitchell, B. & Profit, J. Disparities in NICU quality of care: a qualitative study of family and clinician accounts. J. Perinatol. 38, 600–607 (2018).
Asiodu, I. & Flaskerud, J. H. Got milk? A look at breastfeeding from an African American perspective. Issues Ment. Health Nurs. 32, 544–546 (2011).
O’Brien, K. et al. Effectiveness of family integrated care in neonatal intensive care units on infant and parent outcomes: a multicentre, multinational, cluster-randomised controlled trial. Lancet Child Adolesc. Health 2, 245–254 (2018).
Lion, K. C. & Raphael, J. L. Partnering health disparities research with quality improvement science in pediatrics. Pediatrics 135, 354–361 (2015).
Cooper, L. G. et al. Impact of a family-centered care initiative on NICU care, staff and families. J. Perinatol. 27(Suppl. 2), S32–S37 (2007).
Acknowledgements
This work was supported by the March of Dimes Prematurity Research Center at Stanford University and by the Stanford Maternal and Child Health Research Institute. Drs. J.P., K.S., H.C.L., and J.L. and Mrs. L.B.V. are supported by grants from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (R01 HD083368-01, PI J.P.). Dr. K.S. is also supported by a postdoctoral support award from the Stanford Maternal Child Health Research Institute. Dr. G.P.G. is supported, in part, by a clinical trainee award from the Stanford Maternal Child Health Research Institute. Dr. V.V.P. is supported by a postdoctoral fellowship grant from the National Institutes of Health (F32 HD096778-01). The publication of this article was sponsored by the Necrotizing Enterocolitis (NEC) Society, Patient-Centered Outcomes Research Institute, and National Institutes of Health Eunice Kennedy Shriver National Institute of Child Health and Human Development.
Author information
Authors and Affiliations
Contributions
G.P.G., J.P., J.L., H.C.L., K.G.S., and G.M.S. participated in the planning and design of the study. J.P., J.L., and H.C.L. participated in acquisition of the data. J.L. and G.P.G. analyzed the data. G.P.G. and V.V.P. participated in the primary manuscript writing. All authors participated in editing the manuscript. G.P.G. and J.P. had primary responsibility for the final content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
K.G.S. serves on the advisory board of Evolve, is a paid consultant of Avexegen, received lecture fees from Mednax, and receives grant support from Sera Care. H.C.L. is on the advisory board of Lansinoh Laboratories, Inc. The authors declare no further conflicts of interest.
Ethics approval
This study was approved by the Stanford University Institutional Review Board on Human Subjects Research and the State of California Committee for the Protection of Human Subjects.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Goldstein, G.P., Pai, V.V., Liu, J. et al. Racial/ethnic disparities and human milk use in necrotizing enterocolitis. Pediatr Res 88 (Suppl 1), 3–9 (2020). https://doi.org/10.1038/s41390-020-1073-5
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-020-1073-5
This article is cited by
-
Comparative analysis of necrotizing enterocolitis in preterm infants born in Japan and born to mothers of Japanese ethnicity in California
Scientific Reports (2025)
-
Racial Disparities in Breastmilk Receipt and Extremely Low Gestational Age Neonatal Morbidities in an Asian Pacific Islander Population
Journal of Racial and Ethnic Health Disparities (2023)
-
US state policies for Medicaid coverage of donor human milk
Journal of Perinatology (2022)