Abstract
Background
Pediatric acute-onset neuropsychiatric syndrome (PANS) is an abrupt debilitating psychiatric illness. We anecdotally observed hypoferritinemia and iron deficiency in a subset of patients with PANS, prompting this study.
Methods
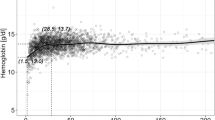
In this IRB-approved prospective cohort study, we included patients seen at the Stanford PANS Clinic who met study criteria. The prevalence of hypoferritinemia (using cut-offs of 7 ng/ml in children ≤ 15 years and 18 ng/ml in adolescents > 15 years) and iron deficiency was estimated. Differences in patients with and without hypoferritinemia during PANS flare were explored.
Results
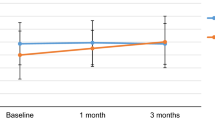
Seventy-nine subjects (mean age of PANS onset of 8.7 years) met study criteria. Hypoferritinemia was observed in 27% and three quarters occurred during a PANS flare. Compared to patients without hypoferritinemia during PANS flare, patients with hypoferritinemia had worse global impairment, more comorbid inflammatory diseases, and exhibited a chronic course of PANS illness. The estimated prevalence of iron deficiency was 3–8% in the PANS cohort, 1.4–2.0-fold higher than in the age- and sex-matched U.S. population. More stringent ferritin level cut-offs than the comparison CDC dataset were used.
Conclusion
Hypoferritinemia and iron deficiency appear to be more common in PANS patients. More research is needed to confirm and understand this association.
Impact
-
Our study suggests hypoferritinemia and iron deficiency are more common in patients with pediatric acute-onset neuropsychiatric syndrome (PANS) than in the sex- and age-matched US population.
-
Hypoferritinemia was commonly observed during a disease flare but not associated with dietary or demographic factors. In patients with PANS and iron deficiency, clinicians should consider possibility of inflammation as the cause especially if iron deficiency cannot be explained by diet and blood loss.
-
Future research should include larger cohorts to corroborate our study findings and consider examining the iron dynamics on MRI brain imaging in order to better understand the pathophysiology of PANS.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Swedo, S., Leckamn, J. & Rose, N. Research subgroup to clinical syndrome: modifying the PANDAS criteria to describe PANS (Pediatric Acute-onset Neuropsychiatric Syndrome). Pediatr. Ther. 2, 113 (2012).
Chang, K. et al. Clinical evaluation of youth with Pediatric Acute-Onset Neuropsychiatric Syndrome (PANS): recommendations from the 2013 PANS Consensus Conference. J. Child Adolesc. Psychopharmacol. 25, 3–13 (2015).
Frankovich, J. et al. Multidisciplinary clinic dedicated to treating youth with pediatric acute-onset neuropsychiatric syndrome: presenting characteristics of the first 47 consecutive patients. J. Child Adolesc. Psychopharmacol. 25, 38–47 (2015).
Calaprice, D., Tona, J., Parker-Athill, E. C. & Murphy, T. K. A survey of pediatric acute-onset neuropsychiatric syndrome characteristics and course. J. Child Adolesc. Psychopharmacol. 27, 607–618 (2017).
Gromark, C. et al. Establishing a pediatric acute-onset neuropsychiatric syndrome clinic: baseline clinical features of the pediatric acute-onset neuropsychiatric syndrome cohort at Karolinska Institutet. J. Child Adolesc. Psychopharmacol. 29, 625–633 (2019).
Hesselmark, E. & Bejerot, S. Clinical features of paediatric acute-onset neuropsychiatric syndrome: findings from a case–control study. Br. J. Psychiatry Open 5, e25 (2019).
Gamucci, A. et al. PANDAS and PANS: clinical, neuropsychological, and biological characterization of a monocentric series of patients and proposal for a diagnostic protocol. J. Child Adolesc. Psychopharmacol. 29, 305–312 (2019).
Johnson, M. et al. Paediatric acute-onset neuropsychiatric syndrome in children and adolescents: an observational cohort study. Lancet Child Adolesc. Health 3, 175–180 (2019).
Zheng, J. et al. Association of pediatric acute-onset neuropsychiatric syndrome with microstructural differences in the deep grey matter. JAMA Netw. Open 3, e204063 (2020).
Giedd, J. N., Rapoport, J. L., Garvey, M. A., Perlmutter, S. & Swedo, S. E. MRI assessment of children with obsessive-compulsive disorder or tics associated with streptococcal infection. Am. J. Psychiatry 157, 281–283 (2000).
Kumar, A., Williams, M. T. & Chugani, H. T. Evaluation of basal ganglia and thalamic inflammation in children with pediatric autoimmune neuropsychiatric disorders associated with streptococcal infection and tourette syndrome: a positron emission tomographic (PET) study using 11C-[R]-PK11195. J. Child Neurol. 30, 749–756 (2015).
Dale, R. C. & Brilot, F. Autoimmune basal ganglia disorders. J. Child Neurol. 27, 1470–1481 (2012).
Cutforth, T., DeMille, M. M., Agalliu, I. & Agalliu, D. CNS autoimmune disease after Streptococcus pyogenes infections: animal models, cellular mechanisms and genetic factors. Future Neurol. 11, 63–76 (2016).
Platt, M. P. et al. Th17 lymphocytes drive vascular and neuronal deficits in a mouse model of postinfectious autoimmune encephalitis. Proc. Natl Acad. Sci. USA 117, 6708–6716 (2020).
Brimberg, L. et al. Behavioral, pharmacological, and immunological abnormalities after streptococcal exposure: a novel rat model of Sydenham chorea and related neuropsychiatric disorders. Neuropsychopharmacology 37, 2076–2087 (2012).
Frick, L. & Pittenger, C. Microglial dysregulation in OCD, Tourette Syndrome, and PANDAS. J. Immunol. Res. 2016, 8606057 (2016).
Lotan, D. et al. Behavioral and neural effects of intra-striatal infusion of anti-streptococcal antibodies in rats. Brain Behav. Immun. 38, 249–262 (2014).
Xu, J. et al. Antibodies from children with PANDAS bind specifically to striatal cholinergic interneurons and alter their activity. Am. J. Psychiatry. (2020).
Yaddanapudi, K. et al. Passive transfer of streptococcus-induced antibodies reproduces behavioral disturbances in a mouse model of pediatric autoimmune neuropsychiatric disorders associated with streptococcal infection. Mol. Psychiatry 15, 712–726 (2010).
Dileepan, T. et al. Group A Streptococcus intranasal infection promotes CNS infiltration by streptococcal-specific Th17 cells. J. Clin. Invest. 126, 303–317 (2016).
Suskind, D. L. Nutritional deficiencies during normal growth. Pediatr. Clin. North Am. 56, 1035–1053 (2009).
CDC. Iron deficiency—United States, 1999−2000. JAMA 288, 2114–2116 (2002).
Camaschella, C. Iron-deficiency anemia. N. Engl. J. Med. 372, 1832–1843 (2015).
Lopez, A., Cacoub, P., Macdougall, L. C. & Peyrin-Biroulet, L. Iron deficiency anaemia. Lancet 387, 907–916 (2016).
Avrahami, M., Barzilay, R., HarGil, M., Weizman, A. & Watemberg, N. Serum ferritin levels are lower in children with tic disorders compared with children without tics: a cross-sectional study. J. Child Adolesc. Psychopharmacol. 27, 192–195 (2016).
Gorman, D. A., Zhu, H., Anderson, G. M., Davies, M. & Peterson, B. S. Ferritin levels and their association with regional brain volumes in Tourette’s syndrome. Am. J. Psychiatry 163, 1264–1272 (2006).
Ghosh, D. & Burkman, E. Relationship of serum ferritin level and tic severity in children with Tourette syndrome. Childs Nerv. Syst. 33, 1373–1378 (2017).
Mader, R., Koton, Y., Buskila, D., Herer, P. & Elias, M. Serum iron and iron stores in non-anemic patients with fibromyalgia. Clin. Rheumatol. 31, 595–599 (2012).
Ortancil, O., Sanli, A., Eryuksel, R., Basaran, A. & Ankarali, H. Association between serum ferritin level and fibromyalgia syndrome. Eur. J. Clin. Nutr. 64, 308–312 (2010).
Shariatpanaahi, M. V., Shariatpanaahi, Z. V., Moshtaaghi, M., Shahbaazi, S. H. & Abadi, A. The relationship between depression and serum ferritin level. Eur. J. Clin. Nutr. 61, 532–535 (2007).
Gottfried, R. J., Gerring, J. P., MacHell, K., Yenokyan, G. & Riddle, M. A. The iron status of children and youth in a community mental health clinic is lower than that of a national sample. J. Child Adolesc. Psychopharmacol. 23, 91–100 (2013).
Chen, M. H. et al. Association between psychiatric disorders and iron deficiency anemia among children and adolescents: a nationwide population-based study. BMC Psychiatry 13, 161 (2013).
Kwak, B. O., Kim, S. N. & Lee, R. Relationship between iron deficiency anemia and febrile seizures in children: a systematic review and meta-analysis. Seizure 52, 27–34 (2017).
Tomoum, H., Habeeb, N., Elagouza, I. & Mobarez, H. Paediatric breath-holding spells are associated with autonomic dysfunction and iron deficiency may play a role. Acta Paediatr. Int. J. Paediatr. 107, 653–657 (2018).
Georgieff, M. K. Iron assessment to protect the developing brain. Am. J. Clin. Nutr. 106, 1588S–1593S (2017).
Barks, A., Fretham, S. J. B., Georgieff, M. K. & Tran, P. V. Early-life neuronal-specific iron deficiency alters the adult mouse hippocampal transcriptome. J. Nutr. 148, 1521–1528 (2018).
Leyshon, B. J., Radlowski, E. C., Mudd, A. T., Steelman, A. J. & Johnson, R. W. Postnatal iron deficiency alters brain development in piglets. J. Nutr. 146, 1420–1427 (2016).
Wiegersma, A. M., Dalman, C., Lee, B. K., Karlsson, H. & Gardner, R. M. Association of prenatal maternal anemia with neurodevelopmental disorders. JAMA Psychiatry 76, 1–12 (2019).
Georgieff, M. K. The role of iron in neurodevelopment: fetal iron deficiency and the developing hippocampus. Biochem. Soc. Trans. 36, 1267–1271 (2008).
Berglund, S. K. et al. The impacts of maternal iron deficiency and being overweight during pregnancy on neurodevelopment of the offspring. Br. J. Nutr. 118, 533–540 (2017).
Wang, W., Knovich, M. A., Coffman, L. G., Torti, F. M. & Torti, S. V. Serum ferritin: past, present and future. Biochim. Biophys. Acta 1800, 760–769 (2010).
Alkhateeb, A. A. & Connor, J. R. The significance of ferritin in cancer: anti-oxidation, inflammation and tumorigenesis. Biochim. Biophys. Acta 1836, 245–254 (2013).
Kernan, K. F. & Carcillo, J. A. Hyperferritinemia and inflammation. Int. Immunol. 29, 401–409 (2017).
Chan, A. L. & Frankovich, J. Infections, antibiotics, and mental health deteriorations. J. Child Adolesc. Psychopharmacol. 29, 647–648 (2019).
Orefici, G, Cardona, F, Cox, C. J. & Cunningham, M. W. in Streptococcus pyogenes: Basic Biology to Clinical Manifestations [Internet]. (University of Oklahoma Health Sciences Center, Oklahoma City, OK, 2016).
Frankovich, J. et al. The burden of caring for a child or adolescent with pediatric acute-onset neuropsychiatric syndrome (PANS): an observational longitudinal study. J. Clin. Psychiatry 80, 17m12091 (2018).
Swedo, S. E., Leckman, J. F. & Rose, N. R. From research subgroup to clinical syndrome: modifying the PANDAS criteria to describe PANS (Pediatric Acute-onset Neuropsychiatric Syndrome). Pediatr. Ther. 2, 1–8 (2012).
Agha, F., Akhter, P. & Khan, R. A. Serum ferritin levels in apparently healthy subjects. J. Pak. Med. Assoc. 37, 63–66 (1987).
Jacobs, A., Miller, F., Worwood, M., Beamish, M. R. & Wardrop, C. A. J. Ferritin in the serum of normal subjects and patients with iron deficiency and iron overload. Br. Med. J. 4, 206–208 (1972).
Siimes, M. A., Addiego, J. E. & Dallman, P. R. Ferritin in serum: diagnosis of iron deficiency and iron overload in infants and children. Blood 43, 581–590 (1974).
Centers for Disease Control and Prevention. Second National Report on Biochemical Indicators of Diet and Nutrition in the US Population [Internet]. https://www.cdc.gov/nutritionreport/pdf/Nutrition_Book_complete508_final.pdf (2012).
Vollmer, S., Bommer, C., Krishna, A., Harttgen, K. & Subramanian, S. V. The association of parental education with childhood undernutrition in low- and middle-income countries: comparing the role of paternal and maternal education. Int. J. Epidemiol. 16, 312–323 (2017).
Leibold, C., Thienemann, M., Farhadian, B., Willett, T. & Frankovich, J. Psychometric properties of the pediatric acute-onset neuropsychiatric syndrome global impairment score in children and adolescents with pediatric acute-onset neuropsychiatric syndrome. J. Child Adolesc. Psychopharmacol. 29, 41–49 (2018).
Novak, M. & Guest, C. Application of a multidimensional caregiver burden inventory. Gerontologist 29, 798–803 (1989).
Farmer, C. et al. Psychometric evaluation of the caregiver burden inventory in children and adolescents with PANS. J. Pediatr. Psychol. 43, 749–757 (2018).
Swedo, S. E. et al. Pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections: clinical description of the first 50 cases. Am. J. Psychiatry 155, 264–271 (1998).
Orlovska, S. et al. Association of streptococcal throat infection with mental disorders: testing key aspects of the PANDAS hypothesis in a nationwide study. JAMA Psychiatry 74, 740–746 (2017).
Nairz, M. et al. Iron and innate antimicrobial immunity—depriving the pathogen, defending the host. J. Trace Elem. Med. Biol. 48, 118–133 (2018).
Quagliariello, A. et al. Gut microbiota profiling and gut-brain crosstalk in children affected by pediatric acute-onset neuropsychiatric syndrome and pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections. Front. Microbiol. 9, 675 (2018).
McCarthy, R. C. et al. Inflammation-induced iron transport and metabolism by brain microglia. J. Biol. Chem. 293, 7853–7863 (2018).
Lane, D. J. R., Ayton, S. & Bush, A. I. Iron and Alzheimer’s disease: an update on emerging mechanisms. J. Alzheimers Dis. 64, S379–S395 (2018).
Bartzokis, G., Tishler, T. A., Shin, I. S., Lu, P. H. & Cummings, J. L. Brain ferritin iron as a risk factor for age at onset in neurodegenerative diseases. Ann. N. Y. Acad. Sci. 1012, 224–236 (2004).
Ropele, S., Enzinger, C. & Fazekas, F. Iron mapping in multiple sclerosis. Neuroimaging Clin. N. Am. 27, 335–342 (2017).
Hayflick, S. J., Kurian, M. A. & Hogarth, P. Neurodegeneration with brain iron accumulation. Handb. Clin. Neurol. 147, 293–305 (2018).
Challacombe, S. J., Scully, C., Keevil, B. & Lehner, T. Serum ferritin in recurrent oral ulceration. J. Oral. Pathol. Med. 12, 290–299 (1983).
Frankovich J., et al. HLA findings in youth with pediatric acute-onset neuropsychiatric syndrome (PANS). In CARRA Annual Meeting 614399 (2019).
Mohammad-Ebrahim, H. et al. Association of killer cell immunoglobulin-like receptor (KIR) genes and their HLA ligands with susceptibility to Behçet’s disease. Scand. J. Rheumatol. 47, 155–163 (2018).
Langkammer, C. et al. Quantitative susceptibility mapping in Parkinson’s disease. PLoS ONE 11, e0162460 (2016).
Langkammer, C., Ropele, S., Pirpamer, L., Fazekas, F. & Schmidt, R. MRI for iron mapping in Alzheimer’s disease. Neurodegener. Dis. 13, 189–191 (2014).
Acknowledgements
We acknowledge Grace Goodwin, Kayla Brown, Gabbi Kamalani, and Dr. Mark Goreman for assistance with data collection. We also acknowledge all the clinicians and staff at the Stanford Immune Behavioral Health Clinic, and Lucile Packard Children’s Hospital for their excellent care of patients with PANS, which allows us to research this disease. J.F. received research funding from the PANDAS Physicians Network and the National Institute of Mental Health, Pediatrics and Developmental Neuroscience Branch. She has also received funding for CME activities through the Foundation for Children with Neuroimmune Disorders. These organizations did not partake in this study.
Author information
Authors and Affiliations
Contributions
J.F. conceptualized and designed the study, supervised research assistants, interpreted data, and provided intellectual review of the manuscript. M.J. provided expertise regarding ferritin, anemia and study design, and revised the manuscript. H.K. conceptualized using the CDC data as a comparison dataset and performed the initial data analysis. Both H.K. and E.S. collected data and prepared the first draft of the manuscript. A.C. contributed to further data acquisition, data analysis and interpretation, and manuscript writing. M.T., T.W., and B.F., FNP-c, provided expert advice on chart reviews/data collection, and revised the manuscript. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent from research subjects
Consent was obtained from parents of minors and adult patients, and assent obtained from patients aged 7–17 years.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chan, A., Karpel, H., Spartz, E. et al. Hypoferritinemia and iron deficiency in youth with pediatric acute-onset neuropsychiatric syndrome. Pediatr Res 89, 1477–1484 (2021). https://doi.org/10.1038/s41390-020-1103-3
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-020-1103-3