Abstract
Background
Late-onset sepsis is an important cause of mortality and morbidity in preterm infants. As these infants rely mostly on their innate immune system to fight off infection, enhancing this immune system by appropriate stimuli may prevent late-onset sepsis. However, it remains unclear which stimuli can enhance the neonatal immune system. This study aims to investigate the influence of intrauterine inflammation on late-onset sepsis.
Methods
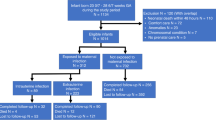
This is a retrospective cohort study in a Neonatal Intensive Care Unit in the Netherlands. Between 2005 and 2016, 1014 infants with ≤32 weeks gestational age and/or with a birth weight ≤1500 g were included. Intrauterine inflammation was subdivided into histological chorioamnionitis, fetal inflammatory response, and funisitis. Logistic and Cox regression analyses were performed to investigate the influence of intrauterine inflammation on late-onset sepsis.
Results
Thirty-six percent of the included infants developed late-onset sepsis; 24% of placentas showed intrauterine inflammation. Late-onset sepsis incidence did not differ between infants with or without exposure to intrauterine inflammation after adjustment for gestational age (histological chorioamnionitis aHR 0.928 [CI: 0.727–1.185], p = 0.551; fetal inflammatory response aHR 1.011 [CI: 0.793–1.288], p = 0.930); funisitis aHR 0.965 [CI: 0.738–1.263], p = 0.797).
Conclusions
Late-onset sepsis in very preterm infants seems not to be associated with intrauterine inflammation.
Impact
-
Intrauterine inflammation is not protective of developing late-onset sepsis in premature infants.
-
A large cohort study on the effect of intrauterine inflammation on neonatal outcome.
-
This study adds to existing knowledge on finding appropriate stimuli to enhance the immune system of premature infants to improve neonatal outcome.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Stoll, B. J. et al. Late-onset sepsis in very low birth weight neonates: the experience of the NICHD Neonatal Research Network. Pediatrics 110, 285–291 (2002).
Lahra, M. M., Beeby, P. J. & Jeffery, H. E. Intrauterine inflammation, neonatal sepsis, and chronic lung disease: a 13-year hospital cohort study. Pediatrics 123, 1314–1319 (2009).
Netea, M. G. & van der Meer, J. W. Trained immunity: an ancient way of remembering. Cell Host Microbe 21, 297–300 (2017).
Kleinnijenhuis, J. et al. Bacille Calmette-Guerin induces NOD2-dependent nonspecific protection from reinfection via epigenetic reprogramming of monocytes. Proc. Natl Acad. Sci. USA 109, 17537–17542 (2012).
Redline, R. W. et al. Amniotic infection syndrome: nosology and reproducibility of placental reaction patterns. Pediatr. Dev. Pathol. 6, 435–448 (2003).
Khong, T. Y. et al. Sampling and definitions of placental lesions: Amsterdam Placental Workshop Group Consensus Statement. Arch. Pathol. Lab. Med. 140, 698–713 (2016).
Goldenberg, R. L., Culhane, J. F., Iams, J. D. & Romero, R. Epidemiology and causes of preterm birth. Lancet 371, 75–84 (2008).
Walsh, M. C. et al. Neonatal outcomes of moderately preterm infants compared to extremely preterm infants. Pediatr. Res. 82, 297–304 (2017).
Arayici, S. et al. The effect of histological chorioamnionitis on the short-term outcome of preterm infants </=32 weeks: a single-center study. J. Matern. Fetal Neonatal Med. 27, 1129–1133 (2014).
Pappas, A. et al. Chorioamnionitis and early childhood outcomes among extremely low-gestational-age neonates. JAMA Pediatr. 168, 137–147 (2014).
Strunk, T. et al. Histologic chorioamnionitis is associated with reduced risk of late-onset sepsis in preterm infants. Pediatrics 129, e134–e141 (2012).
Ahn, H. M., Park, E. A., Cho, S. J., Kim, Y. J. & Park, H. S. The association of histological chorioamnionitis and antenatal steroids on neonatal outcome in preterm infants born at less than thirty-four weeks’ gestation. Neonatology 102, 259–264 (2012).
Pietrasanta, C. et al. Impact of different stages of intrauterine inflammation on outcome of preterm neonates: gestational age-dependent and -independent effect. PLoS ONE 14, e0211484 (2019).
Papile, L. A., Burstein, J., Burstein, R. & Koffler, H. Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1,500 gm. J. Pediatr. 92, 529–534 (1978).
Lee, J. S. & Polin, R. A. Treatment and prevention of necrotizing enterocolitis. Semin. Neonatol. 8, 449–459 (2003).
Erdemir, G. et al. Histological chorioamnionitis: effects on premature delivery and neonatal prognosis. Pediatr. Neonatol. 54, 267–274 (2013).
Lau, J. et al. Chorioamnionitis with a fetal inflammatory response is associated with higher neonatal mortality, morbidity, and resource use than chorioamnionitis displaying a maternal inflammatory response only. Am. J. Obstet. Gynecol. 193, 708–713 (2005).
Arayici, S. et al. The effect of histological chorioamnionitis on the short-term outcome of preterm infants ≤32 weeks: a single-center study. J. Matern. Fetal Neonatal Med. 27, 1129–1133 (2014).
Villamor-Martinez, E. et al. Association of histological and clinical chorioamnionitis with neonatal sepsis among preterm infants: a systematic review, meta-analysis, and meta-regression. Front. Immunol. 11, 972 (2020).
Kramer, B. W. et al. Endotoxin-induced maturation of monocytes in preterm fetal sheep lung. Am. J. Physiol. Lung Cell. Mol. Physiol. 293, L345–L353 (2007).
Kramer, B. W. et al. Endotoxin-induced chorioamnionitis modulates innate immunity of monocytes in preterm sheep. Am. J. Respir. Crit. Care Med. 171, 73–77 (2005).
Kallapur, S. G. et al. Pulmonary and systemic endotoxin tolerance in preterm fetal sheep exposed to chorioamnionitis. J. Immunol. 179, 8491–8499 (2007).
Levy, O. Innate immunity of the human newborn: distinct cytokine responses to LPS and other Toll-like receptor agonists. J. Endotoxin Res. 11, 113–116 (2005).
Namakula, R. et al. Monocytes from neonates and adults have a similar capacity to adapt their cytokine production after previous exposure to BCG and β-glucan. PLoS ONE 15, e0229287 (2020).
Dowling, D. J. & Levy, O. Ontogeny of early life immunity. Trends Immunol. 35, 299–310 (2014).
Levy, O. Innate immunity of the newborn: basic mechanisms and clinical correlates. Nat. Rev. Immunol. 7, 379–390 (2007).
Melville, J. M. & Moss, T. J. The immune consequences of preterm birth. Front. Neurosci. 7, 79 (2013).
Lahra, M. M., Beeby, P. J. & Jeffery, H. E. Maternal versus fetal inflammation and respiratory distress syndrome: a 10-year hospital cohort study. Arch. Dis. Child. Fetal Neonatal Ed. 94, F13–F16 (2009).
Watterberg, K. L., Scott, S. M. & Naeye, R. L. Chorioamnionitis, cortisol, and acute lung disease in very low birth weight infants. Pediatrics 99, E6 (1997).
Thomas, W. & Speer, C. P. Chorioamnionitis: important risk factor or innocent bystander for neonatal outcome? Neonatology 99, 177–187 (2011).
Inder, T. E, Perlman, J. M. & Volpe, J. J. in Volpe’s Neurology of the Newborn (eds Volpe, J. J. et al.) Ch. 24 (Elsevier, 2018).
Lahra, M. M., Gordon, A. & Jeffery, H. E. Chorioamnionitis and fetal response in stillbirth. Am. J. Obstet. Gynecol. 196, 229.e1–229.e4 (2007).
Lahra, M. M. & Jeffery, H. E. A fetal response to chorioamnionitis is associated with early survival after preterm birth. Am. J. Obstet. Gynecol. 190, 147–151 (2004).
Acknowledgements
We would like to thank O. Tjoa and T. Knol for assisting in the completion of the database and C.F. Peeters for support on statistical analyses. Furthermore, we thank the staff of the Department of Neonatology and the Department of Pathology of the VUmc for their assistance in the logistics of this study.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study design and interpretation of the data. M.B.v.D. completed the database, assisted in analysis of placental pathology, performed statistical analyses, drafted the manuscript, and revised it before final approval. J.P.v.d.V. analyzed placental pathology and revised and approved the final version before publication. D.H.V. contributed significantly to the conception of the design of the research, the interpretation of the results, and revising the manuscript before publication. M.M.v.W. contributed to the study design, interpretation of the results, and revision of the manuscript before publication. H.L.T. revised the manuscript and contributed to the interpretation of the results.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
van Doorn, M.B., van der Voorn, J.P., Tanger, H.L. et al. Exposure to intrauterine inflammation and late-onset sepsis in very preterm infants. Pediatr Res 91, 230–234 (2022). https://doi.org/10.1038/s41390-021-01455-0
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-021-01455-0
This article is cited by
-
Intrauterine inflammation exposure may increase the risk of late-onset sepsis in premature infants: a retrospective cohort study
Italian Journal of Pediatrics (2025)