Abstract
Background
The Neonatal Resuscitation Program (NRP) recommends using 100% O2 during chest compressions and adjusting FiO2 based on SpO2 after return of spontaneous circulation (ROSC). The optimal strategy for adjusting FiO2 is not known.
Methods
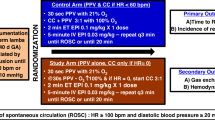
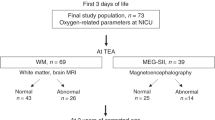
Twenty-five near-term lambs asphyxiated by umbilical cord occlusion to cardiac arrest were resuscitated per NRP. Following ROSC, lambs were randomized to gradual decrease versus abrupt wean to 21% O2 followed by FiO2 titration to achieve NRP SpO2 targets. Carotid blood flow and blood gases were monitored.
Results
Three minutes after ROSC, PaO2 was 229 ± 32 mmHg in gradual wean group compared to 57 ± 13 following abrupt wean to 21% O2 (p < 0.001). PaO2 remained high in the gradual wean group at 10 min after ROSC (110 ± 10 vs. 67 ± 12, p < 0.01) despite similar FiO2 (~0.3) in both groups. Cerebral O2 delivery (C-DO2) was higher above physiological range following ROSC with gradual wean (p < 0.05). Lower blood oxidized/reduced glutathione ratio (suggesting less oxidative stress) was observed with abrupt wean.
Conclusion
Weaning FiO2 abruptly to 0.21 with adjustment based on SpO2 prevents surge in PaO2 and C-DO2 and minimizes oxidative stress compared to gradual weaning from 100% O2 following ROSC. Clinical trials with neurodevelopmental outcomes comparing post-ROSC FiO2 weaning strategies are warranted.
Impact
-
In a lamb model of perinatal asphyxial cardiac arrest, abrupt weaning of inspired oxygen to 21% prevents excessive oxygen delivery to the brain and oxidative stress compared to gradual weaning from 100% oxygen following return of spontaneous circulation.
-
Clinical studies assessing neurodevelopmental outcomes comparing abrupt and gradual weaning of inspired oxygen after recovery from neonatal asphyxial arrest are warranted.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Halling, C., Sparks, J. E., Christie, L. & Wyckoff, M. H. Efficacy of intravenous and endotracheal epinephrine during neonatal cardiopulmonary resuscitation in the delivery room. J. Pediatr 185, 232-236 (2017).
Wyckoff, M. H. et al. Neonatal Life Support: 2020 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations. Circulation 142(Suppl 1), S185–s221 (2020).
Gunn, A. J. et al. Hypothermia: an evolving treatment for neonatal hypoxic ischemic encephalopathy. Pediatrics 121, 648–649 (2008); author reply 9–50.
Black, R. E. et al. Global, regional, and national causes of child mortality in 2008: a systematic analysis. Lancet 375, 1969–1987 (2010).
Vento, M., Escobar, J., Cernada, M., Escrig, R. & Aguar, M. The use and misuse of oxygen during the neonatal period. Clin. Perinatol. 39, 165–176 (2012).
Miller, S. L., Wallace, E. M. & Walker, D. W. Antioxidant therapies: a potential role in perinatal medicine. Neuroendocrinology 96, 13–23 (2012).
Perez-de-Sa, V. et al. High brain tissue oxygen tension during ventilation with 100% oxygen after fetal asphyxia in newborn sheep. Pediatr. Res. 65, 57–61 (2009).
Kumar, V. H. et al. Exposure to supplemental oxygen and its effects on oxidative stress and antioxidant enzyme activity in term newborn lambs. Pediatr. Res. 67, 66–71 (2010).
Kapadia, V. S. et al. Perinatal asphyxia with hyperoxemia within the first hour of life is associated with moderate to severe hypoxic-ischemic encephalopathy. J. Pediatr. 163, 949–954 (2013).
Shankaran, S. et al. Whole-body hypothermia for neonates with hypoxic-ischemic encephalopathy. N. Engl. J. Med. 353, 1574–1584 (2005).
Azzopardi, D. V. et al. Moderate hypothermia to treat perinatal asphyxial encephalopathy. N. Engl. J. Med. 361, 1349–1358 (2009).
Foglia, E. E. et al. Duration of resuscitation at birth, mortality, and neurodevelopment: a systematic review. Pediatrics 146, e20201449 (2020).
Badurdeen, S. et al. Excess cerebral oxygen delivery follows return of spontaneous circulation in near-term asphyxiated lambs. Sci. Rep. 10, 16443 (2020).
American Academy of Pediatrics, Weiner, G. M., American Heart Association & Zaichkin J. Textbook of Neonatal Resuscitation. 7th edn (American Academy of Pediatrics, 2016).
Wyckoff, M. H. et al. Part 13: Neonatal Resuscitation: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 132(Suppl 2), S543–S560 (2015).
Aziz, K. et al. Part 5: Neonatal Resuscitation: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 142(Suppl 2), S524–S550 (2020).
Rawat, M. et al. Oxygenation and hemodynamics during chest compressions in a lamb model of perinatal asphyxia induced cardiac arrest. Children (Basel) 6, 52 (2019).
Kilkenny, C., Browne, W. J., Cuthill, I. C., Emerson, M. & Altman, D. G. Improving bioscience research reporting: the ARRIVE guidelines for reporting animal research. PLoS Biol. 8, e1000412 (2010).
Vali, P. et al. Evaluation of timing and route of epinephrine in a neonatal model of asphyxial arrest. J. Am. Heart Assoc. 6, e004402 (2017).
Isayama, T. et al. The route, dose, and interval of epinephrine for neonatal resuscitation: a systematic review. Pediatrics 146, e20200586 (2020).
Rawat, M. et al. Optimal oxygen targets in term lambs with meconium aspiration syndrome and pulmonary hypertension. Am. J. Respir. Cell Mol. Biol. 63, 510–518 (2020).
Lakshminrusimha, S. & Steinhorn, R. H. Pulmonary vascular biology during neonatal transition. Clin. Perinatol. 26, 601–619 (1999).
Patel, A. et al. Exposure to supplemental oxygen downregulates antioxidant enzymes and increases pulmonary arterial contractility in premature lambs. Neonatology 96, 182–192 (2009).
Soothill, P. W., Nicolaides, K. H., Rodeck, C. H. & Campbell, S. Effect of gestational age on fetal and intervillous blood gas and acid-base values in human pregnancy. Fetal Ther. 1, 168–175 (1986).
Koch, G. & Wendel, H. Adjustment of arterial blood gases and acid base balance in the normal newborn infant during the first week of life. Biol. Neonat. 12, 136–161 (1968).
Saugstad, O. D., Oei, J.-L., Lakshminrusimha, S. & Vento, M. Oxygen therapy of the newborn from molecular understanding to clinical practice. Pediatr. Res. 85, 20–29 (2019).
Østerholt, H. C. et al. Antioxidant protects against increases in low molecular weight hyaluronan and inflammation in asphyxiated newborn pigs resuscitated with 100% oxygen. PLoS ONE 7, e38839 (2012).
Solberg, R., Andresen, J. H., Escrig, R., Vento, M. & Saugstad, O. D. Resuscitation of hypoxic newborn piglets with oxygen induces a dose-dependent increase in markers of oxidation. Pediatr. Res. 62, 559–563 (2007).
Shalak, L. & Perlman, J. M. Hypoxic-ischemic brain injury in the term infant-current concepts. Early Hum. Dev. 80, 125–141 (2004).
Koch, J. D., Miles, D. K., Gilley, J. A., Yang, C.-P. & Kernie, S. G. Brief exposure to hyperoxia depletes the glial progenitor pool and impairs functional recovery after hypoxic-ischemic brain injury. J. Cereb. Blood Flow Metab. 28, 1294–1306 (2008).
Lakshminrusimha, S. et al. Pulmonary hemodynamics and vascular reactivity in asphyxiated term lambs resuscitated with 21 and 100% oxygen. J. Appl Physiol. (1985) 111, 1441–1447 (2011).
Ferguson, L. P., Durward, A. & Tibby, S. M. Relationship between arterial partial oxygen pressure after resuscitation from cardiac arrest and mortality in children. Circulation 126, 335–342 (2012).
Maconochie, I. K. et al. Pediatric Life Support: 2020 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations. Circulation 142(Suppl 1), S140–S84 (2020).
Saugstad, O. D., Ramji, S., Soll, R. F. & Vento, M. Resuscitation of newborn infants with 21% or 100% oxygen: an updated systematic review and meta-analysis. Neonatology 94, 176–182 (2008).
Saugstad, O. D., Rootwelt, T. & Aalen, O. Resuscitation of asphyxiated newborn infants with room air or oxygen: an international controlled trial: the Resair 2 study. Pediatrics 102, e1 (1998).
Ramji, S. et al. Resuscitation of asphyxic newborn infants with room air or 100% oxygen. Pediatr. Res. 34, 809–812 (1993).
Linner, R., Werner, O., Perez-de-Sa, V. & Cunha-Goncalves, D. Circulatory recovery is as fast with air ventilation as with 100% oxygen after asphyxia-induced cardiac arrest in piglets. Pediatr. Res. 66, 391–394 (2009).
Solevag, A. L., Dannevig, I., Nakstad, B. & Saugstad, O. D. Resuscitation of severely asphyctic newborn pigs with cardiac arrest by using 21% or 100% oxygen. Neonatology 98, 64–72 (2010).
Solevåg, A. L. et al. Myocardial perfusion and oxidative stress after 21% vs. 100% oxygen ventilation and uninterrupted chest compressions in severely asphyxiated piglets. Resuscitation 106, 7–13 (2016).
Rosenberg, A. A. Cerebral blood flow and O2 metabolism after asphyxia in neonatal lambs. Pediatr. Res. 20, 778–782 (1986).
Chandrasekharan, P. K. et al. Continuous end-tidal carbon dioxide monitoring during resuscitation of asphyxiated term lambs. Neonatology 109, 265–273 (2016).
Perez, M., Robbins, M. E., Revhaug, C. & Saugstad O. D. Oxygen radical disease in the newborn, revisited: oxidative stress and disease in the newborn period. Free Radic. Biol. Med. 142, 61–72 (2019).
Thornton, C., Baburamani, A. A., Kichev, A. & Hagberg, H. Oxidative stress and endoplasmic reticulum (ER) stress in the development of neonatal hypoxic-ischaemic brain injury. Biochem. Soc. Trans. 45, 1067–1076 (2017).
Giustarini, D., Milzani, A., Dalle-Donne, I. & Rossi, R. Red blood cells as a physiological source of glutathione for extracellular fluids. Blood Cells Mol. Dis. 40, 174–179 (2008).
Vali, P. et al. The perinatal asphyxiated lamb model: a model for newborn resuscitation. J. Vis. Exp. 57553 (2018).
Acknowledgements
The work has been supported by NIH grants HD096299 (to P.V.), HD072929 (to S.L.), American Academy of Pediatrics- Neonatal Resuscitation Program Research Grant (to S.L.), UC Davis Child Health Research Grant and First Tech Federal Credit Union (to D.S.), Children’s Miracle Network at UC Davis Children’s Hospital Research Grant (to D.S.), and NRP Research Grant from Canadian Pediatric Society. Presented in an abstract form at the American Academy of Pediatrics, National Conference and Exhibition (AAP-NCE) 2020 and received the Young Investigator Award (D.S.).
Author information
Authors and Affiliations
Contributions
D.S. and S.L. made substantial contributions to conception and design, acquisition, extraction, analysis and interpretation of data and drafting the manuscript. P.V., P.C., A.L.L., M.E.H., Z.A., M.H.W., and S.W. made substantial contributions to data acquisition and extraction. All authors critically revised and approved the final version for publication.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interest.
Consent
Patient consent was not required
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Sankaran, D., Vali, P., Chen, P. et al. Randomized trial of oxygen weaning strategies following chest compressions during neonatal resuscitation. Pediatr Res 90, 540–548 (2021). https://doi.org/10.1038/s41390-021-01551-1
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-021-01551-1
This article is cited by
-
Neonatal chest compressions: time to act
Pediatric Research (2021)