Abstract
Background
Although electrocardiogram (ECG) can detect heart rate (HR) faster compared to pulse oximetry, it remains unknown if routine use of ECG for delivery room (DR) resuscitation reduces the time to stabilization in preterm infants.
Methods
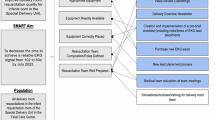
Neonates <31 weeks’ gestation were randomized to either an ECG-displayed or an ECG-blinded HR assessment in the DR. HR, oxygen saturation, resuscitation interventions, and clinical outcomes were compared.
Results
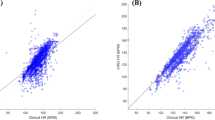
During the study period, 51 neonates were enrolled. The mean gestational age in both groups was 28 ± 2 weeks. The time to stabilization, defined as the time from birth to achieve HR ≥100 b.p.m., as well as oxygen saturation within goal range, was not different between the ECG-displayed and the ECG-blinded groups [360 (269, 435) vs 345 (240, 475) s, p = 1.00]. There was also no difference in the time to HR ≥100 b.p.m. [100 (75, 228) vs 138 (88, 220) s, p = 0.40] or duration of positive pressure ventilation (PPV) [345 (120, 558) vs 196 (150, 273) s, p = 0.36]. Clinical outcomes were also similar between groups.
Conclusions
Although feasible and safe, the use of ECG in the DR during preterm resuscitation did not reduce time to stabilization.
Impact
-
Although feasible and apparently safe, routine use of the ECG in the DR did not decrease time to HR >100 b.p.m., time to stabilization, or use of resuscitation interventions such as PPV for preterm infants <31 weeks’ gestational age.
-
This article adds to the limited randomized controlled trial evidence regarding the impact of routine use of ECG during preterm resuscitation on DR clinical outcomes.
-
Such evidence is important when considering recommendations for routine use of the ECG in the DR worldwide as such a recommendation comes with a significant cost burden.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
Change history
17 December 2021
A Correction to this paper has been published: https://doi.org/10.1038/s41390-021-01835-6
References
Yangthara B, Horrasith, S., Paes, B. & Kitsommart, R. Predictive factors for intensive birth resuscitation in a developing-country: a 5-year, single-center study AU - Yangthara, Buranee. J. Matern. Fetal Neonatal Med. 33, 570–576 (2018).
Kakkilaya, V. et al. Quality improvement project to decrease delivery room intubations in preterm infants. Pediatrics 143, e20180201 (2019).
Wyckoff, M. H. et al. Part 13: neonatal resuscitation. Circulation 132, S543–S560 (2015).
Wyllie, J. et al. Part 7: neonatal resuscitation: 2015 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations. Resuscitation 95, e169–e201 (2015).
Aziz, K. et al. Part 5: neonatal resuscitation: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Pediatrics 147, e2020038505E (2021).
Wyckoff, M. H. et al. Neonatal life support: 2020 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations. Circulation 142, S185–S221 (2020).
Perlman, J. M. et al. Part 7: neonatal resuscitation: 2015 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations. Circulation 132, S204–S241. (2015).
Bajaj, M. et al. Delivery room resuscitation and short-term outcomes in moderately preterm infants. J. Pediatr. 195, 33–38.e32 (2018).
Bashir, A. et al. Neonatal outcomes based on mode and intensity of delivery room resuscitation. J. Perinatol. 37, 1103 (2017).
DeMauro, S. B. et al. Impact of delivery room resuscitation on outcomes up to 18 months in very low birth weight infants. The. J. Pediatr. 159, 546–550.e541 (2011).
Shah, B. A. et al. Impact of electronic cardiac (ECG) monitoring on delivery room resuscitation and neonatal outcomes. Resuscitation 143, 10–16 (2019).
Vali, P. & Lakshminrusimha, S. ECG monitoring: one step closer to the modernization of the delivery room. Resuscitation 98, e4–e5 (2016).
Chitkara, R. et al. The accuracy of human senses in the detection of neonatal heart rate during standardized simulated resuscitation: implications for delivery of care, training and technology design. Resuscitation 84, 369–372 (2013).
Kamlin, C. O., O’Donnell, C. P., Everest, N. J., Davis, P. G. & Morley, C. J. Accuracy of clinical assessment of infant heart rate in the delivery room. Resuscitation 71, 319–321 (2006).
Owen, C. J. & Wyllie, J. P. Determination of heart rate in the baby at birth. Resuscitation 60, 213–217 (2004).
Voogdt, K. G., Morrison, A. C., Wood, F. E., van Elburg, R. M. & Wyllie, J. P. A randomised, simulated study assessing auscultation of heart rate at birth. Resuscitation 81, 1000–1003 (2010).
Kamlin, C. O. et al. Accuracy of pulse oximetry measurement of heart rate of newborn infants in the delivery room. J. Pediatr. 152, 756–760 (2008).
Katheria, A., Rich, W. & Finer, N. Electrocardiogram provides a continuous heart rate faster than oximetry during neonatal resuscitation. Pediatrics 130, e1177–e1181 (2012).
Mizumoto, H. et al. Electrocardiogram shows reliable heart rates much earlier than pulse oximetry during neonatal resuscitation. Pediatr. Int. 54, 205–207 (2012).
van Vonderen, J. J. et al. Pulse oximetry measures a lower heart rate at birth compared with electrocardiography. J. Pediatr. 166, 49–53 (2015).
Narayen, I. C. et al. Low signal quality pulse oximetry measurements in newborn infants are reliable for oxygen saturation but underestimate heart rate. Acta Paediatr. 104, e158–e163 (2015).
Dawson, J. A. et al. Changes in heart rate in the first minutes after birth. Arch. Dis. Child. Fetal Neonatal Ed. 95, F177–F181 (2010).
Katheria, A. et al. A pilot randomized controlled trial of EKG for neonatal resuscitation. PLoS ONE 12, e0187730 (2017).
Iglesias, B. et al. 3-lead electrocardiogram is more reliable than pulse oximetry to detect bradycardia during stabilisation at birth of very preterm infants. Arch. Dis. Child Fetal Neonatal Ed. 103, F233–F237 (2018).
Murphy, M. C., De Angelis, L., McCarthy, L. K. & O’Donnell, C. P. F. Randomised study comparing heart rate measurement in newly born infants using a monitor incorporating electrocardiogram and pulse oximeter versus pulse oximeter alone. Arch. Dis. Child. 104, F547–F550 (2018).
Kapadia, V. S. et al. Resuscitation of preterm neonates with limited versus high oxygen strategy. Pediatrics 132, e1488–e1496 (2013).
Higgins, R. D. et al. Evaluation and management of women and newborns with a maternal diagnosis of chorioamnionitis: Summary of a Workshop. Obstet. Gynecol. 127, 426–436 (2016).
Jobe, A. H. & Bancalari, E. Bronchopulmonary dysplasia. Am. J. Respir. Crit. Care Med. 163, 1723–1729 (2001).
Stoll, B. J. et al. Neonatal outcomes of extremely preterm infants from the NICHD Neonatal Research Network. Pediatrics 126, 443–456 (2010).
Papile, L.-A., Burstein, J., Burstein, R. & Koffler, H. Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1,500 gm. J. Pediatr. 92, 529–534 (1978).
Prematurity* CoRo. The International Classification of Retinopathy of Prematurity Revisited. Arch. Ophthalmol. 123, 991–999 (2005).
Bell, M. J. et al. Neonatal necrotizing enterocolitis - therapeutic decisions based upon clinical staging. Ann. Surg. 187, 1–7 (1978).
Baik, N. et al. Cardiocirculatory monitoring during immediate fetal-to-neonatal transition: a systematic qualitative review of the literature. Neonatology 107, 100–107 (2015).
Hawkes, G. A., O’Toole, J. M., Kenosi, M., Ryan, C. A. & Dempsey, E. M. Perfusion index in the preterm infant immediately after birth. Early Hum. Dev. 91, 463–465 (2015).
Townsel, C. D., Emmer, S. F., Campbell, W. A. & Hussain. N. Gender differences in respiratory morbidity and mortality of preterm neonates. Front. Pediatr. 5, 6 (2017).
Bjorland, P. A. et al. 2020 Changes in heart rate from 5 s to 5 min after birth in vaginally delivered term newborns with delayed cord clamping. Arch. Dis. Child. 106, 311–315 (2020).
Funding
V.K. acknowledges support by K23HD083511 grant from the NIH.
Author information
Authors and Affiliations
Contributions
All authors made substantial contributions to conception and design, acquisition of data, analysis and interpretation of data, and critical revisions for important intellectual content. N.V.A. wrote the first draft of the manuscript. All authors approved the final version of the manuscript as submitted.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent statement
Parental informed consent was obtained postnatally.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: Table 2 has been corrected.
Supplementary information
Rights and permissions
About this article
Cite this article
Abbey, N.V., Mashruwala, V., Weydig, H.M. et al. Electrocardiogram for heart rate evaluation during preterm resuscitation at birth: a randomized trial. Pediatr Res 91, 1445–1451 (2022). https://doi.org/10.1038/s41390-021-01731-z
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-021-01731-z
This article is cited by
-
A portable dry-electrode ECG device for rapid and accurate neonatal heart rate monitoring during resuscitation
Scientific Reports (2025)
-
A validated NICU database: recounting 50 years of clinical growth, quality improvement and research
Pediatric Research (2025)