Abstract
Background
Following preterm birth, the immature kidney is exposed to several harmful conditions, with an increased risk of renal impairment. We aimed to assess urinary biomarkers of renal function in very preterm infants during early nephrotoxic treatments.
Methods
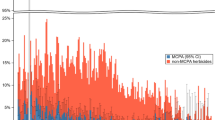
Infants ≤32 weeks’ gestation and ≤1500 g were enrolled in this observational prospective study. Urine samples were collected on day 1(T1), 2–4(T2), 5–7(T3), 8–10(T4), 11–13(T5). The following urinary biomarkers were determined: osteopontin (uOPN), epidermal growth factor (uEGF), neutrophil gelatinase-associated lipocalin (uNGAL), cystatin C (uCysC). The infants were grouped according to their exposure to amikacin or ibuprofen during the study period and a between-group comparison of urinary biomarkers at each time point was performed.
Results
Thirty-six infants were included. Urinary CysC, uOPN, and uNGAL rose significantly during ibuprofen or amikacin treatment, while no difference was observed for uEGF. After adjustment for possible influencing factors, amikacin administration was associated with higher uCysC at T1 (p = 0.007) and T2 (p = 0.016), whereas ibuprofen increased uOPN (p = 0.001) and uNGAL concentration (p = 0.009) at T3.
Conclusion
Nephrotoxic therapies induce molecule-specific change patterns of renal function biomarkers in treated preterm infants. Serial assessments of these biomarkers may aid to identify neonates at risk of renal impairment and to develop tailored therapeutic approaches.
Impact
-
Despite the wide use of nephrotoxic therapies in neonatal settings, little is known on their effect on renal function biomarkers in preterm infants.
-
This study describes molecule-specific change patterns of urinary biomarkers during ibuprofen and amikacin administration, suggesting underlying pathophysiological effects on renal function.
-
Given their low analytical costs and non-invasive collection, the urinary biomarkers investigated in this study represent a promising strategy for serial monitoring of renal function in at-risk neonates and may aid the early detection of renal function impairment at different kidney levels during nephrotoxic treatments.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Harrison, M. S. & Goldenberg, R. L. Global burden of prematurity. Semin. Fetal Neonatal Med. 21, 74–79 (2016).
Frey, H. A. & Klebanoff, M. A. The epidemiology, etiology, and costs of preterm birth. Semin. Fetal Neonatal Med. 21, 68–73 (2016).
Sutherland, M. R. et al. Accelerated maturation and abnormal morphology in the preterm neonatal kidney. J. Am. Soc. Nephrol. 22, 1365–1374 (2011).
Majed, B., Bateman, D. A., Uy, N. & Lin, F. Patent ductus arteriosus is associated with acute kidney injury in the preterm infant. Pediatr. Nephrol. 34, 1129–1139 (2019).
Coggins, S. A. et al. Acute kidney injury associated with late-onset neonatal sepsis: a matched cohort study. J. Pediatr. 231, 185–192.e4 (2021).
Rhone, E. T., Carmody, J. B., Swanson, J. R. & Charlton, J. R. Nephrotoxic medication exposure in very low birth weight infants. J. Matern Neonatal Med. 27, 1485–1490 (2014).
Girardi, A. et al. Drug-induced renal damage in preterm neonates: State of the art and methods for early detection. Drug Saf. 38, 535–551 (2015).
Girardi, A. et al. Pattern of drug use among preterm neonates: results from an Italian neonatal intensive care unit. Ital. J. Pediatr. 43, 37 (2017).
Mian, A., Guillet, R., Ruck, L., Wang, H. & Schwartz, G. Acute kidney injury in premature, very low-birth-weight infants. J. Pediatr. Intensive Care 05, 069–078 (2015).
Shalaby, M. A. et al. Incidence, risk factors, and outcome of neonatal acute kidney injury: a prospective cohort study. Pediatr. Nephrol. 33, 1617–1624 (2018).
Nagaraj, N., Berwal, P. K., Srinivas, A. & Berwal, A. A study of acute kidney injury in hospitalized preterm neonates in NICU. J. Neonatal Perinat. Med. 9, 417–421 (2016).
Gjerde, A., Lillas, B. S., Marti, H. P., Reisaeter, A. V. & Vikse, B. E. Intrauterine growth restriction, preterm birth and risk of end-stage renal disease during the first 50 years of life. Nephrol. Dial. Transpl. 35, 1157–1163 (2020).
Maqsood, S., Fung, N., Chowdhary, V., Raina, R. & Mhanna, M. J. Outcome of extremely low birth weight infants with a history of neonatal acute kidney injury. Pediatr. Nephrol. 32, 1035–1043 (2017).
Crump, C., Sundquist, J., Winkleby, M. A. & Sundquist, K. Preterm birth and risk of chronic kidney disease from childhood into mid-adulthood: national cohort study. BMJ 365, 1346 (2019).
Libório, A. B., Branco, K. M. P. C. & Torres De Melo Bezerra, C. Acute kidney injury in neonates: from urine output to new biomarkers. Biomed. Res. Int. 2014, 601568 (2014).
Kamianowska, M., Szczepański, M. & Wasilewska, A. Tubular and glomerular biomarkers of acute kidney injury in newborns. Curr. Drug Metab. 20, 332–349 (2019).
La Manna, G. et al. Urinary neutrophil gelatinase-associated lipocalin at birth predicts early renal function in very low birth weight infants. Pediatr. Res. 70, 379–383 (2011).
Askenazi, D. J. et al. Acute kidney injury urine biomarkers in very low-birth-weight infants. Clin. J. Am. Soc. Nephrol. 11, 1527–1535 (2016).
Jansen, D. et al. Tubular injury biomarkers to detect gentamicin-induced acute kidney injury in the neonatal intensive care unit. Am. J. Perinatol. 33, 180–187 (2015).
McWilliam, S. J. et al. Mechanism-based urinary biomarkers to identify the potential for aminoglycoside-induced nephrotoxicity in premature neonates: a proof-of-concept study. PLoS ONE 7, e43809 (2012).
Stojanović, V., Barišić, N., Milanović, B. & Doronjski, A. Acute kidney injury in preterm infants admitted to a neonatal intensive care unit. Pediatr. Nephrol. 29, 2213–2220 (2014).
Capelli, I. et al. Biomarkers of kidney injury in very-low-birth-weight preterm infants: Influence of maternal and neonatal factors. Vivo (Brooklyn) 34, 1333–1339 (2020).
Zohdi, V. et al. Low birth weight due to intrauterine growth restriction and/or preterm birth: effects on nephron number and long-term renal health. Int. J. Nephrol. 2012, 136942 (2012).
Jain, A. & Shah, P. S. Diagnosis, evaluation, and management of patent ductus arteriosus in preterm neonates. JAMA Pediatr. 169, 863–872 (2015).
Sweet, D. G. et al. European consensus guidelines on the management of respiratory distress syndrome–2019 Update. Neonatology 115, 432–450 (2019).
Cailes, B. et al. Epidemiology of UK neonatal infections: the neonIN infection surveillance network. Arch. Dis. Child Fetal Neonatal Ed. 103, F547–F553 (2018).
Bell, M. J. et al. Neonatal necrotizing enterocolitis. Therapeutic decisions based upon clinical staging. Ann. Surg. 187, 1–7 (1978).
WHO Collaborating Centre for Drug Statistics Methodology. Guidelines for ATC Classification and DDD Assignment (2021).
Schwartz, G. J., Brion, L. P. & Spitzer, A. The use of plasma creatinine concentration for estimating glomerular filtration rate in infants, children, and adolescents. Pediatr. Clin. North Am. 34, 571–590 (1987).
Nada, A., Bonachea, E. M. & Askenazi, D. J. Acute kidney injury in the fetus and neonate (2017).
Ostermann, M., Karsten, E. & Lumlertgul, N. Biomarker-based management of AKI: fact or fantasy? Nephron 1–7 https://doi.org/10.1159/000518365 (2021).
Herget-Rosenthal, S., van Wijk, J. A. E., Bröcker-Preuss, M. & Bökenkamp, A. Increased urinary cystatin C reflects structural and functional renal tubular impairment independent of glomerular filtration rate. Clin. Biochem. 40, 946–951 (2007).
Hanna, M. et al. Early urinary biomarkers of acute kidney injury in preterm infants. Pediatr. Res. 80, 218–223 (2016).
Kuribayashi, R. et al. Urinary neutrophil gelatinase-associated lipocalin is an early predictor of acute kidney injury in premature infants. Exp. Ther. Med. 12, 3706–3710 (2016).
Jung, Y. H., Han, D., Shin, S. H., Kim, E. K. & Kim, H. S. Proteomic identification of early urinary-biomarkers of acute kidney injury in preterm infants. Sci. Rep. 10, 4057 (2020).
Barbati, A. et al. Urinary Cystatin-C, a marker to assess and monitor neonatal kidney maturation and function: validation in twins. Pediatr. Res. 89, 932–939 (2021).
Askenazi, D. J. et al. Urine biomarkers predict acute kidney injury and mortality in very low birth weight infants. J. Pediatr. 159, 907–912.e1 (2011).
Prusakov, P. et al. A global point prevalence survey of antimicrobial use in neonatal intensive care units: the no-more-antibiotics and resistance (NO-MAS-R) study. EClinicalMedicine 32, 100727 (2021).
Langhendries, J. P. et al. Once-a-day administration of amikacin in neonates: assessment of nephrotoxicity and ototoxicity. Dev. Pharm. Ther. 20, 220–230 (1993).
McWilliam, S. J., Antoine, D. J., Smyth, R. L. & Pirmohamed, M. Aminoglycoside-induced nephrotoxicity in children. Pediatr. Nephrol. 32, 2015–2025 (2017).
Kaseda, R. et al. Megalin-mediated endocytosis of cystatin C in proximal tubule cells. Biochem. Biophys. Res. Commun. 357, 1130–1134 (2007).
van Donge, T., Smits, A., van den Anker, J. & Allegaert, K. Amikacin or vancomycin exposure alters the postnatal serum creatinine dynamics in extreme low birth weight neonates. Int. J. Environ. Res. Public Health 18, 1–11 (2021).
Raaijmakers, A. et al. Ibuprofen exposure in early neonatal life does not affect renal function in young adolescence. Arch. Dis. Child Fetal Neonatal Ed. 103, F107–F111 (2018).
Van Overmeire, B. et al. Prophylactic ibuprofen in premature infants: a multicentre, randomised, double-blind, placebo-controlled trial. Lancet 364, 1945–1949 (2004).
van Donge, T., Allegaert, K., Pfister, M., Smits, A. & van den Anker, J. Creatinine trends to detect ibuprofen-related maturational adverse drug events in neonatal life: a simulation study for the ELBW newborn. Front. Pharmacol. 11, 610294 (2021).
Kent, A. L. et al. Renal glomeruli and tubular injury following indomethacin, ibuprofen, and gentamicin exposure in a neonatal rat model. Pediatr. Res. 62, 307–312 (2007).
Chen, C. Y., Pang, V. F. & Chen, C. S. Pathological and biochemical modifications of renal function in ibuprofen-induced interstitial nephritis. Ren. Fail 18, 31–40 (1996).
Tosse, V. et al. Urinary NT-proBNP, NGAL, and H-FABP may predict hemodynamic relevance of patent ductus arteriosus in very low birth weight infants. Neonatology 101, 260–266 (2012).
Waldherr, S. et al. Urinary acute kidney injury biomarkers in very low-birth-weight infants on indomethacin for patent ductus arteriosus. Pediatr. Res. 85, 678–686 (2019).
Allegaert, K. et al. Effects of co-administration of ibuprofen-lysine on the pharmacokinetics of amikacin in preterm infants during the first days of life. Biol. Neonate 86, 207–211 (2004).
Prieto-García, L. et al. Pathophysiological mechanisms underlying a rat model of triple whammy acute kidney injury. Lab. Investig. 100, 1455–1464 (2020).
Stoops, C. et al. Baby NINJA (Nephrotoxic Injury Negated by Just-in-Time Action): reduction of Nephrotoxic Medication-Associated Acute Kidney Injury in the Neonatal Intensive Care Unit. J. Pediatr. 215, 223–228 (2019).
Salerno, S. N. et al. Association between nephrotoxic drug combinations and acute kidney injury in the neonatal intensive care unit. J. Pediatr. 228, 213–219 (2021).
DeFreitas, M. J. et al. Longitudinal patterns of urine biomarkers in infants across gestational ages. Pediatr. Nephrol. 31, 1179–1188 (2016).
Askenazi, D. J. et al. Baseline values of candidate urine acute kidney injury biomarkers vary by gestational age in premature infants. Pediatr. Res. 70, 302–306 (2011).
Saeidi, B. et al. Impact of gestational age, sex, and postnatal age on urine biomarkers in premature neonates. Pediatr. Nephrol. 30, 2037–2044 (2015).
Huynh, T. K. et al. Reference values of urinary neutrophil gelatinase-associated lipocalin in very low birth weight infants. Pediatr. Res. 66, 528–532 (2009).
Acknowledgements
We thank Anna Girardi and Luca Leonardi for their contribution in data collection, and Maria Cappuccilli for supervising sample analysis.
Funding
This study received financial support by the “Fondazione del Monte” institution (grant no. FdM/3884).
Author information
Authors and Affiliations
Contributions
E.P., I.C., and S.G. designed the study. F.V. enrolled the patients and acquired the data. C.D. analyzed the study samples. S.M. and E.P. performed the statistical analysis. E.R., V.A., F.D.P., and L.C. contributed to data interpretation. S.M. wrote the first draft of the manuscript; E.P., F.V., and I.C. contributed to the draft writing. All the authors critically revised the manuscript for important intellectual content, approved the final version of the manuscript submitted for publication and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All persons designated as authors qualify for authorship, and all those who qualify for authorship are listed.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent to participate
The study protocol was approved by the S. Orsola University Hospital Ethics Committee, Bologna, Italy (protocol no. 154/2015/U/Oss) and written informed consent for study participation was obtained from the parents/legal guardians of each patient.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Martini, S., Vitali, F., Capelli, I. et al. Impact of nephrotoxic drugs on urinary biomarkers of renal function in very preterm infants. Pediatr Res 91, 1715–1722 (2022). https://doi.org/10.1038/s41390-021-01905-9
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-021-01905-9
This article is cited by
-
Urinary biomarkers of acute kidney injury in neonates < 25 weeks’ gestation: a pilot study
Pediatric Nephrology (2026)
-
Advocating for the inclusion of kidney health outcomes in neonatal research: best practice recommendations by the Neonatal Kidney Collaborative
Journal of Perinatology (2024)
-
Gestational age-specific clinical correlates of acute kidney injury in preterm infants with necrotizing enterocolitis
Pediatric Research (2023)
-
Nephrotoxic drugs and renal function in preterm infants: are urinary biomarkers the answer?
Pediatric Research (2022)
-
Ibuprofen
Reactions Weekly (2022)