Abstract
Background
Bronchopulmonary dysplasia (BPD) is the most common morbidity complicating preterm birth and affects long-term respiratory outcomes. The objectives of this study were to establish whether serum periostin at birth, day of life (DOL) 28, and corrected 36 weeks’ gestational age could be potential biomarkers for BPD.
Methods
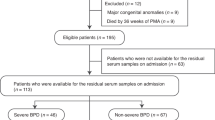
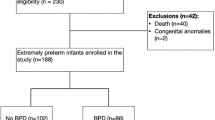
A total of 98 preterm Japanese infants born at <32 weeks and comparing 41 healthy controls born at term, were divided into BPD (n = 44) and non-BPD (n = 54) cohorts. Serum periostin levels were measured using an enzyme-linked immunosorbent assay.
Results
Among 98 preterm infants, the median serum periostin levels at birth were higher with BPD (338.0 ng/mL) than without (275.0 ng/mL, P < 0.001). Multivariate analysis revealed that serum periostin levels at birth were significantly associated with BPD (P = 0.013). Serum periostin levels at birth with moderate/severe BPD (345.0 ng/mL) were significantly higher than those with non-BPD/mild BPD (283.0 ng/mL, P = 0.006).
Conclusions
Serum periostin levels were significantly correlated with birth weight and gestational age, and serum periostin levels at birth in BPD infants were significantly higher than that in non-BPD infants.
Impact
-
This study found higher serum periostin levels at birth in preterm infants subsequently diagnosed with bronchopulmonary dysplasia.
-
It also emerged that serum periostin levels at birth significantly correlated with gestational age and birth weight.
-
The mechanism by which serum periostin is upregulated in BPD infants needs further investigation.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Gough, A., Spence, D., Linden, M., Halliday, H. L. & McGarvey, L. P. A. General and respiratory health outcomes in adult survivors of bronchopulmonary dysplasia: a systematic review. Chest 141, 1554–1567 (2012).
Gough, A. et al. Impaired lung function and health status in adult survivors of bronchopulmonary dysplasia. Eur. Respir. J. 43, 808–816 (2014).
Kinsella, J. P., Greenough, A. & Abman, S. H. Bronchopulmonary dysplasia. Lancet 367, 1421–1431 (2006).
Baraldi, E. & Filippone, M. Chronic lung disease after premature birth. N. Engl. J. Med. 357, 1946–1955 (2007).
Anderson, P. J. & Doyle, L. W. Neurodevelopmental outcome of bronchopulmonary dysplasia. Semin. Perinatol. 30, 227–232 (2006).
Izuhara, K. et al. Periostin in allergic inflammation. Allergol. Int. 63, 143–151 (2014).
Izuhara, K. et al. Periostin: an emerging biomarker for allergic diseases. Allergy 74, 2116–2128 (2019).
Nanri, Y. et al. Cross-talk between transforming growth factor-β and periostin can be targeted for pulmonary fibrosis. Am. J. Respir. Cell Mol. Biol. 62, 204–216 (2020).
Yoshihara, T. et al. Periostin plays a critical role in the cell cycle in lung fibroblasts. Respir. Res. 21, 38 (2020).
Okamoto, M. et al. Periostin, a matrix protein, is a novel biomarker for idiopathic interstitial pneumonias. Eur. Respir. J. 37, 1119–1127 (2011).
Murata, K. et al. Accumulation of periostin in acute exacerbation of familial idiopathic pulmonary fibrosis. J. Thorac. Dis. 10, E587–E591 (2018).
Naik, P. K. et al. Periostin promotes fibrosis and predicts progression in patients with idiopathic pulmonary fibrosis. Am. J. Physiol. Lung Cell Mol. Physiol. 303, L1046–L1056 (2018).
Nakazawa, T. et al. Gene expression of periostin in the early stage of fracture healing detected by cDNA microarray analysis. J. Orthop. Res. 22, 520–525 (2004).
Bozyk, P. D. et al. Neonatal periostin knockout mice are protected from hyperoxia-induced alveolar simplication. PLoS ONE 7, e31336 (2012).
Ahlfeld, S. K., Davis, S. D., Kelley, K. J. & Poindexter, B. B. Early elevation of plasma periostin is associated with chronic ventilator-dependent bronchopulmonary dysplasia. Am. J. Respir. Crit. Care Med. 194, 1430–1433 (2016).
Anderson, H. M. et al. Relationships among aeroallergen sensitization, peripheral blood eosinophils, and periostin in pediatric asthma development. J. Allergy Clin. Immunol. 139, 790–796 (2017).
Fujitani, H. et al. Age-related changes in serum periostin level in allergic and non-allergic children. Allergol. Int. 68, 285–286 (2019).
Jobe, A. H. & Bancalari, E. Bronchopulmonary dysplasia. Am. J. Respir. Crit. Care Med. 163, 1723–1729 (2001).
Itabashi, K., Miura, F., Uehara, R. & Nakamura New Japanese neonatal anthropometric charts for gestational age at birth. Pediatr. Int. 56, 702–708 (2014).
Matsusaka, M. et al. Phenotype of asthma related with high serum periostin levels. Allergol. Int. 64, 175e80 (2015).
Kimura, H. et al. Sinus computed tomographic findings in adult smokers and nonsmokers with asthma. Analysis of clinical indices and biomarkers. Ann. Am. Thorac. Soc. 14, 332e41 (2017).
Oak, P. & Hilgendorff, A. The BPD trio? Interaction of dysregulated PDGF, VEGF, and TGF signaling in neonatal chronic lung disease. Mol. Cell Pediatr. 4, 11 (2017).
Golpe, R. et al. Differences in systemic inflammation between cigarette and biomass smoke-induced COPD. Int. J. Chron. Obstruct. Pulmon. Dis. 12, 2639–2646 (2017).
Pavlidis, S. et al. “T2-high” in severe asthma related to blood eosinophil, exhaled nitric oxide and serum periostin. Eur. Respir. J. 53, 1800938 (2019).
Ahlfeld, S. K. et al. Periostin downregulation is an early marker of inhibited neonatal murine lung alveolar septation. Birth Defects Res. A Clin. Mol. Teratol. 97, 373–385 (2013).
Mokres, L. M. et al. Prolonged mechanical ventilation with air induces apoptosis and causes failure of alveolar septation and angiogenesis in lungs of newborn mice. Am. J. Physiol. Lung Cell Mol. Physiol. 298, L23–L35 (2010).
Hilgendorff, A. et al. Neonatal mice genetically modified to express the elastase inhibitor elafin are protected against the adverse effects of mechanical ventilation on lung growth. Am. J. Physiol. Lung Cell Mol. Physiol. 303, L215–L227 (2012).
Go, H. et al. Extracellular vesicle miRNA-21 is a potential biomarker for predicting chronic lung disease in premature infants. Am. J. Physiol. Lung Cell Mol. Physiol. 318, L845–L851 (2020).
Kanemitsu, Y. et al. Increased periostin associates with greater airflow limitation in patients receiving inhaled corticosteroids. J. Allergy Clin. Immunol. 132, 305e12 (2013).
Kudo, A. Periostin in fibrillogenesis for tissue regeneration: periostin actions inside and outside the cell. Cell Mol. Life Sci. 68, 3201–3207 (2011).
Aly, H. et al. Gestational age, sex and maternal parity correlate with bone turnover in premature infants. Pediatr. Res. 57, 708–711 (2005).
Zein, H. et al. Cord blood cytokine levels correlate with types of placental pathology in extremely preterm infants. Front. Pediatr. 9, 607684 (2021).
Romero, R. et al. Clinical chorioamnionitis at term V: umbilical cord plasma cytokine profile in the context of a systemic maternal inflammatory response. J. Perinat. Med. 44, 53–76 (2016).
Takayama, G. et al. Periostin: a novel component of subepithelial fibrosis of bronchial asthma downstream of IL-4 and IL-13 signals. J. Allergy Clin. Immunol. 118, 98–104 (2006).
Baier, R. J., Loggins, J. & Kruger, T. E. Interleukin-4 and 13 concentrations in infants at risk to develop bronchopulmonary dysplasia. BMC Pediatr. 3, 8 (2003).
Perez, G. F. et al. Rhinovirus-induced airway cytokines and respiratory morbidity in severely premature children. Pediatr. Allergy Immunol. 26, 145–152 (2015).
Kou, K. et al. Periostin levels correlate with disease severity and chronicity in patients with atopic dermatitis. Br. J. Dermatol. 171, 283–291 (2014).
Ono, J., Takai, M., Kamei, A., Azuma, Y. & Izuhara, K. Pathological roles and clinical usefulness of periostin in type 2 inflammation and pulmonary fibrosis. Biomolecules 11, 1084 (2021).
Acknowledgements
Junya Ono is a salaried employee of Shino-Test Co., Ltd., which provided ELISA for periostin without stipulations or influence over the interpretation of test results. The authors have no other potential or actual conflicts of interest pertaining to the contents of this article.
Funding
This work was supported by Grants-in-Aid Scientific Research from the Japan Society for the Promotion of Science, KAKENHI (Grant number: 20K08233).
Author information
Authors and Affiliations
Contributions
H.G. designed the study, carried out the analyses, and drafted multiple iterations of the manuscript. H.O., K.N., S.N., K.I., and M.H. supervised the study and edited the manuscript. J.O. carried out the analyses and reviewed the manuscript. H.M., K.O., M.S., K.S., M.C., Y.K., H.I., Y.K., N.K., and K.H. collected the samples and reviewed the manuscript. All authors concur with the final manuscript are accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
Junya Ono is a salaried employee of Shino-Test Co., Ltd. The remaining authors declare no competing interests.
Patient consent statement
Informed consent was solicited from parents or other legal guardians, and documented in writing.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Go, H., Ono, J., Ohto, H. et al. Can serum periostin predict bronchopulmonary dysplasia in premature infants?. Pediatr Res 92, 1108–1114 (2022). https://doi.org/10.1038/s41390-021-01912-w
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-021-01912-w
This article is cited by
-
Expression of periostin in the epithelium of cholesteatoma with different degrees of ossicular chain destruction and its clinical value in predicting postoperative hearing recovery
BioMedical Engineering OnLine (2024)
-
Functional lung morphometry: another piece in the BPD prediction puzzle?
Pediatric Research (2023)