Abstract
Background
Late and moderate preterm (LMPT) infants are at risk for adverse later life outcomes. We determined the association between feeding method at enrolment and growth and body composition of LMPT infants until 3 months corrected age (3mCA).
Methods
Infants born between 32+0 and 36+6 weeks of gestation (n = 107) were enrolled up to 4 weeks corrected age and stratified according to feeding at enrolment. We performed anthropometric measurements at enrolment, term equivalent age (TEA) and 3mCA, including skinfold measurements and body composition using dual X-ray absorptiometry (DEXA).
Results
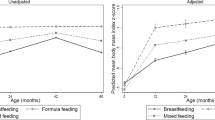
Feeding method at enrolment was associated with fat mass (FM) (breast 554.9 g, mixed 716.8 g, formula 637.7 g, p = 0.048), lean body mass (LM) (2512 g, 2853 g, 2722 g, respectively, p = 0.009) and lean mass index (LMI) (10.6 kg/m2, 11.6 kg/m2,11.2 kg/m2 respectively, p = 0.008) at TEA, but not 3mCA. Breastfed infants demonstrated greater increase in LM (breast 1707 g, mixed 1536 g, formula 1384 g, p = 0.03) and LMI (1.23 kg/m2, 0.10 kg/m2, 0.52 kg/m2, respectively, p = 0.022) between TEA and 3mCA.
Conclusions
Breastfed LMPT infants have lower FM and greater LM increase and LMI increase up to 3mCA compared to formula or mixed-fed infants. These findings stress the importance of supporting breastfeeding in this population.
Impact
-
Infants born late and moderate preterm age who are exclusively breastfed soon after birth gain more lean mass up to 3 months corrected age compared to mixed- or formula-fed infants.
-
Breastfed infants have lower lean and fat mass at term equivalent age compared to mixed- and formula-fed infants.
-
This is the first study exploring this population’s growth and body composition in detail at 3 months corrected age.
-
Our results underline the importance of supporting mothers to initiate and continue breastfeeding at least until 3 months corrected age.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
Data availability
The data sets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Chawanpaiboon, S. et al. Global, regional, and national estimates of levels of preterm birth in 2014: a systematic review and modelling analysis. Lancet Glob. Health 7, e37–e46 (2019).
Karnati, S., Kollikonda, S. & Abu-Shaweesh, J. Late preterm infants - changing trends and continuing challenges. Int. J. Pediatr. Adolesc. Med. 7, 36–44 (2020).
Johnson, S. et al. Differentiating the preterm phenotype: distinct profiles of cognitive and behavioral development following late and moderately preterm birth. J. Pediatr. 193, 85.e1–92.e1 (2018).
Boyle, E. M. et al. Effects of gestational age at birth on health outcomes at 3 and 5 years of age: population based cohort study. BMJ 344, e896 (2012).
Pfister, K. M. et al. Early body composition changes are associated with neurodevelopmental and metabolic outcomes at 4 years of age in very preterm infants. Pediatr. Res. 84, 713–718 (2018).
Belfort, M. B., Gillman, M. W., Buka, S. L., Casey, P. H. & McCormick, M. C. Preterm infant linear growth and adiposity gain: trade-offs for later weight status and intelligence quotient. J. Pediatrics 163, 1564–1569.e2 (2013).
Sammallahti, S. et al. Growth after late-preterm birth and adult cognitive, academic, and mental health outcomes. Pediatr. Res. 81, 767–774 (2017).
Cordova, E. G. et al. Association of poor postnatal growth with neurodevelopmental impairment in infancy and childhood: comparing the fetus and the healthy preterm infant references. J. Pediatr. 225, 37–43.e5 (2020).
Euser, A. M. et al. Associations between prenatal and infancy weight gain and BMI, fat mass, and fat distribution in young adulthood: a prospective cohort study in males and females born very preterm. Am. J. Clin. Nutr. 81, 480–487 (2005).
Reilly, J. J. et al. Early life risk factors for obesity in childhood: cohort study. BMJ 330, 1357 (2005).
de Fluiter, K. S., van Beijsterveldt, I., Breij, L. M., Acton, D. & Hokken-Koelega, A. Association between fat mass in early life and later fat mass trajectories. JAMA Pediatr. 174, 1141–1148 (2020).
Druet, C. et al. Prediction of childhood obesity by infancy weight gain: an individual-level meta-analysis. Paediatr. Perinat. Epidemiol. 26, 19–26 (2012).
Giannì, M. L. et al. Postnatal catch-up fat after late preterm birth. Pediatr. Res. 72, 637–640 (2012).
Gupta, P. et al. Physical growth, morbidity profile and mortality among healthy late preterm neonates. Indian Pediatr. 54, 629–634 (2017).
Santos, I. S. et al. Late preterm birth is a risk factor for growth faltering in early childhood: a cohort study. BMC Pediatr. 9, 71 (2009).
Dotinga, B. M. et al. Longitudinal growth and emotional and behavioral problems at age 7 in moderate and late preterms. PLoS ONE 14, e0211427 (2019).
Bocca-Tjeertes, I. F., Kerstjens, J. M., Reijneveld, S. A., de Winter, A. F. & Bos, A. F. Growth and predictors of growth restraint in moderately preterm children aged 0 to 4 years. Pediatrics 128, e1187–e1194 (2011).
Goyal, N. K., Fiks, A. G. & Lorch, S. A. Persistence of underweight status among late preterm infants. Arch. Pediatr. Adolesc. Med. 166, 424–430 (2012).
Lapillonne, A. et al. Feeding the late and moderately preterm infant: a Position Paper of the European Society for Paediatric Gastroenterology, Hepatology and Nutrition Committee on Nutrition. J. Pediatr. Gastroenterol. Nutr. 69, 259–270 (2019).
Yan, J., Liu, L., Zhu, Y., Huang, G. & Wang, P. P. The association between breastfeeding and childhood obesity: a meta-analysis. BMC Public Health 14, 1267 (2014).
Anderson, J. W., Johnstone, B. M. & Remley, D. T. Breast-feeding and cognitive development: a meta-analysis. Am. J. Clin. Nutr. 70, 525–535 (1999).
Kakaroukas, A. et al. An observational cohort study and nested randomized controlled trial on nutrition and growth outcomes in moderate and late preterm infants (FLAMINGO). Front. Nutr. 8, 561419 (2021).
Ministry of Housing, Communities & Local Government. English indices of deprivation 2019. https://www.gov.uk/government/statistics/english-indices-of-deprivation-2019 (2019).
WHO. WHO Anthro for personal computers [Internet]. Child growth standards. Geneva; 2010. Available from: http://www.who.int/childgrowth/software/en/
Pan, H. & Cole T. LMSgrowth. http://www.healthforallchildren.co.uk/ (2012).
StataCorp. Stata Statistical Software (StataCorp LLC., 2022).
von Elm E. et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. BMJ 335, 806 (2007).
Roggero, P., Giannì, M. L., Liotto, N., Piemontese, P. & Mosca, F. Late preterm infants’ growth and body composition after discharge. Ital. J. Pediatr. 40, A27 (2014).
Giannì, M. L. et al. Postnatal catch-up fat after late preterm birth. Pediatr. Res. 72, 637–640 (2012).
Giannì, M. L. et al. Does human milk modulate body composition in late preterm infants at term-corrected age? Nutrients 8, 664 (2016).
Zhao, Z. et al. Trajectories of length, weight, and bone mineral density among preterm infants during the first 12 months of corrected age in China. BMC Pediatr. 15, 91 (2015).
Maastrup, R. et al. Breastfeeding progression in preterm infants is influenced by factors in infants, mothers and clinical practice: the results of a national cohort study with high breastfeeding initiation rates. PLoS ONE 9, e108208 (2014).
Demirci, J. R., Sereika, S. M. & Bogen, D. Prevalence and predictors of early breastfeeding among late preterm mother-infant dyads. Breastfeed. Med. 8, 277–285 (2013).
Goyal, N. K., Attanasio, L. B. & Kozhimannil, K. B. Hospital care and early breastfeeding outcomes among late preterm, early-term, and term infants. Birth 41, 330–338 (2014).
Jónsdóttir, R. B., Jónsdóttir, H., Skúladóttir, A., Thorkelsson, T. & Flacking, R. Breastfeeding progression in late preterm infants from birth to one month. Matern. Child Nutr. 16, e12893 (2020).
Nagulesapillai, T., McDonald, S. W., Fenton, T. R., Mercader, H. F. & Tough, S. C. Breastfeeding difficulties and exclusivity among late preterm and term infants: results from the all our babies study. Can. J. Public Health 104, e351–e356 (2013).
Giannì, M. L. et al. Facilitators and barriers of breastfeeding late preterm infants according to mothers’ experiences. BMC Pediatr. 16, 179 (2016).
Carpay, N. C., Kakaroukas, A., D Embleton, N. & van Elburg, R. M. Barriers and facilitators to breastfeeding in moderate and late preterm infants: a systematic review. Breastfeed. Med. 16, 370–384 (2021).
Kair, L. R. & Colaizy, T. T. Breastfeeding continuation among late preterm infants: barriers, facilitators, and any association with NICU admission? Hospital Pediatr. 6, 261–268 (2016).
Blackwell, M. T. et al. Interneonatal intensive care unit variation in growth rates and feeding practices in healthy moderately premature infants. J. Perinatol. 25, 478–485 (2005).
Mitha, A. et al. The impact of neonatal unit policies on breast milk feeding at discharge of moderate preterm infants: the EPIPAGE-2 cohort study. Matern. Child Nutr. 15, e12875 (2019).
McCormick, M. C., Escobar, G. J., Zheng, Z. & Richardson, D. K. Place of birth and variations in management of late preterm (“near-term”) infants. Semin. Perinatol. 30, 44–47 (2006).
Stettler, N., Kumanyika, S. K., Katz, S. H., Zemel, B. S. & Stallings, V. A. Rapid weight gain during infancy and obesity in young adulthood in a cohort of African Americans. Am. J. Clin. Nutr. 77, 1374–1378 (2003).
Hamatschek, C. et al. Fat and fat-free mass of preterm and term infants from birth to six months: a review of current evidence. Nutrients 12, 288 (2020).
Ramel, S. E. et al. Greater early gains in fat-free mass, but not fat mass, are associated with improved neurodevelopment at 1 year corrected age for prematurity in very low birth weight preterm infants. J. Pediatr. 173, 108–115 (2016).
Scheurer, J. M. et al. Body composition trajectories from infancy to preschool in children born premature versus full-term. J. Pediatr. Gastroenterol. Nutr. 64, e147–e153 (2017).
Johnson, S. et al. Neurodevelopmental outcomes following late and moderate prematurity: a population-based cohort study. Arch. Dis. Child. Fetal Neonatal Ed. 100, F301–F308 (2015).
Acknowledgements
We are very thankful to the Research Nursing staff of the Royal Victoria Infirmary for assisting with the enrolment and data collection for the study. The data analysis was performed by independent statisticians who have no conflict of interest to declare.
Funding
This research was funded by Danone Nutricia Research via an Investigator Led Clinical Research Funding award to Newcastle Hospitals NHS Foundation Trust.
Author information
Authors and Affiliations
Contributions
M.A.-B., N.D.E. and R.M.v.E. concepted and designed the study. A.K., J.E.B. and N.D.E. acquired data. L.H. and R.J.Q.M.N. performed the statistical analysis and interpretation was done by all authors. A.K., M.A.-B., N.D.E., R.M.v.E. and J.E.B. drafted the article. All authors took part revising the paper. A.K., M.A.-B., N.D.E. and R.M.v.E. had primary responsibility for the final content. All authors read and approved the final version of manuscript.
Corresponding author
Ethics declarations
Competing interests
M.A.-B. is an employee of Danone Nutricia Research. R.M.v.E. was an employee of Danone Nutricia Research during conduct of this study. N.D.E. and J.E.B. declare research funding from Danone Early Life Nutrition and Prolacta Biosciences US and lecture honoraria from Nestle Nutrition Institute. The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Ethics approval and consent to participate
The study was reviewed by the North East–York Research Ethics Committee, approved by the NHS Health Research Authority (IRAS project ID: 237542) and registered at ISRCTN (ISRCTN15469594). The procedures followed were in accordance with the Helsinki Declaration of 1975 as revised in 1983. Consent was sought and obtained according to the standards of ethical research. Parents of eligible infants were approached from the time of birth up to 4 weeks after term equivalent age and given a study leaflet, explained the study and answered questions and approached again at a second stage to answer questions and explore intention for consent.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kakaroukas, A., Abrahamse-Berkeveld, M., Hayes, L. et al. Early infancy growth, body composition and type of feeding in late and moderate preterms. Pediatr Res 93, 1927–1935 (2023). https://doi.org/10.1038/s41390-022-02317-z
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-022-02317-z
This article is cited by
-
Formula with large, milk phospholipid-coated lipid droplets in late-moderate preterm infants: a double-blind RCT
Pediatric Research (2025)
-
Post-Hospital Discharge Nutrition for the Preterm Infant
Current Treatment Options in Pediatrics (2025)
-
Nutritional intake and growth until two years of age in moderate and late preterms
Pediatric Research (2024)