Abstract
Background
We assessed associations between maternal stress, social support, and child resiliency during the COVID-19 pandemic in relation to changes in anxiety and depression symptoms in children in Mexico City.
Methods
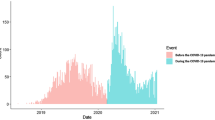
Participants included 464 mother-child pairs from a longitudinal birth cohort in Mexico City. At ages 8–11 (pre-COVID, 2018–2019) and 9–12 (during COVID, May–Nov 2020) years, depressive symptoms were assessed using the child and parent-reported Children’s Depressive Inventory. Anxiety symptoms were assessed using the child-reported Revised Manifest Anxiety Scale. Linear regression models were used to estimate associations between maternal stress, social support, and resiliency in relation to changes in depressive and anxiety symptoms. We additionally assessed outcomes using clinically relevant cut-points. Models were adjusted for child age and sex and maternal socioeconomic status and age.
Results
Higher continuous maternal stress levels during the COVID-19 pandemic were associated with increases in depressive symptoms (β: 0.72; 95% CI: 0.12, 1.31), and higher odds of clinically relevant depressive and anxiety symptoms in the children.
Conclusions
Maternal stress during the pandemic may increase mental health symptoms in pre-adolescent children. Additional studies are needed that examine the long-term pandemic-related impacts on mental health throughout the adolescent years.
Impact
-
In this longitudinal cohort study of children in Mexico City, we observed that depressive symptoms were higher from before to during the pandemic.
-
Maternal stress surrounding the pandemic may increase mental health symptoms in pre-adolescent children.
-
Child resiliency may help to protect against pandemic-related stressors.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
Data availability
The datasets generated during and/or analyzed during the current study are not publicly available due to privacy concerns, but a limited dataset may be available from the corresponding author on reasonable request.
References
Brooks, S. K. et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet 395, 912–920 (2020).
Lee, C. M., Cadigan, J. M. & Rhew, I. C. Increases in loneliness among young adults during the Covid-19 pandemic and association with increases in mental health problems. J. Adolesc. Health 67, 714–717 (2020).
Loades, M. E. et al. Rapid systematic review: the impact of social isolation and loneliness on the mental health of children and adolescents in the context of Covid-19. J. Am. Acad. Child Adolesc. Psychiatry 59, 1218.e3–1239.e3 (2020).
Russell, B. S., Hutchison, M., Tambling, R., Tomkunas, A. J. & Horton, A. L. Initial challenges of caregiving during Covid-19: caregiver burden, mental health, and the parent-child relationship. Child Psychiatry Hum. Dev. 51, 671–682 (2020).
Cost, K. T. et al. Mostly worse, occasionally better: impact of Covid-19 pandemic on the mental health of canadian children and adolescents. Eur. Child Adolesc. Psychiatry 31, 671–684 (2021).
Qin, Z. et al. Prevalence and risk factors associated with self-reported psychological distress among children and adolescents during the Covid-19 pandemic in China. JAMA Netw. Open 4, e2035487 (2021).
Samji, H. et al. Review: Mental health impacts of the Covid-19 pandemic on children and youth - a systematic review. Child Adolesc. Ment. Health 27, 173–189 (2021).
Khambadkone, S. G., Cordner, Z. A. & Tamashiro, K. L. K. Maternal stressors and the developmental origins of neuropsychiatric risk. Front. Neuroendocrinol. 57, 100834 (2020).
Van den Bergh, B. R. H. et al. Prenatal developmental origins of behavior and mental health: the influence of maternal stress in pregnancy. Neurosci. Biobehav. Rev. 117, 26–64 (2020).
Serrano-Villar, M., Huang, K. Y. & Calzada, E. J. Social support, parenting, and social emotional development in young Mexican and Dominican American children. Child Psychiatry Hum. Dev. 48, 597–609 (2017).
Benjet, C., Borges, G., Medina-Mora, M. E., Zambrano, J. & Aguilar-Gaxiola, S. Youth mental health in a populous city of the developing world: results from the Mexican adolescent mental health survey. J. Child Psychol. Psychiatry 50, 386–395 (2009).
Zuccolo, P. F. et al. Children and adolescents’ emotional problems during the Covid-19 pandemic in Brazil. Eur. Child Adolesc. Psychiatry https://doi.org/10.1007/s00787-022-02006-6 (2022).
Bravo-Sanzana, M., Oriol, X. & Miranda, R. Characterization of wellbeing and its relationship with exposure to violence in Mexican and Chilean early and late adolescents during the Covid-19 pandemic. Child Indic. Res. 15, 553–578 (2022).
CDC. The social-ecological model: a framework for prevention. https://www.cdc.gov/violenceprevention/about/social-ecologicalmodel.html (2021).
Meherali, S. et al. Mental health of children and adolescents amidst Covid-19 and past pandemics: a rapid systematic review. Int. J. Environ. Res. Public Health 18, 3432 (2021).
Braun, J. M. et al. Relationships between lead biomarkers and diurnal salivary cortisol indices in pregnant women from Mexico City: a cross-sectional study. Environ. Health 13, 50 (2014).
Davanzo, P. et al. Spanish translation and reliability testing of the child depression inventory. Child Psychiatry Hum. Dev. 35, 75–92 (2004).
Ferrando, P. J. Factorial structure of the Revised Children Manifest Anxiety Scale in a Spanish sample - relations with Eysenck personality dimensions. Pers. Indiv. Differ. 16, 693–699 (1994).
Kovacs, M. & MHS Staff. Children’s Depression Inventory 2nd Edition (Cdi 2) Technical Manual (MHS, Inc., 2011).
Berry, C. A., Quinn, K. A., Portillo, N. & Shalowitz, M. U. Reliability and validity of the Spanish Version of the Crisis in Family Systems-Revised. Psychol. Rep. 98, 123–132 (2006).
Shalowitz, M. U., Berry, C. A., Rasinski, K. A. & Dannhausen-Brun, C. A. A new measure of contemporary life stress: development, validation, and reliability of the Crisys. Health Serv. Res. 33, 1381–1402 (1998).
Myers, H. F. Ethnicity- and socio-economic status-related stresses in context: an integrative review and conceptual model. J. Behav. Med. 32, 9–19 (2009).
Rosa, M. J. et al. Prenatal and postnatal stress and wheeze in Mexican children: sex-specific differences. Ann. Allergy Asthma Immunol. 116, 306–312 e301 (2016).
Tamayo, Y. O. M. et al. Maternal stress modifies the effect of exposure to lead during pregnancy and 24-month old children’s neurodevelopment. Environ. Int. 98, 191–197 (2017).
Mendoza-Núñez, V. M., González-Mantilla, F., Correa-Muñoz, E. & Retana-Ugalde, R. Relationship between social support networks and physical functioning in older community-dwelling Mexicans. Int. J. Environ. Res. Public Health 14, 993 (2017).
Reynolds, C. R. & Kamphaus, R. W. Basc-2: Behavior Assessment System for Children, 2 (Pearson, 2004).
Textor, J., Hardt, J. & Knuppel, S. Dagitty: a graphical tool for analyzing causal diagrams. Epidemiology 22, 745 (2011).
Carrasco, A. J. E. The Amai system of classifying households by socio-economic level: the experience of Mexico and its comparison with Brazil and Argentina. www.esomar.org (2002).
Buckley, J. P., Doherty, B. T., Keil, A. P. & Engel, S. M. Statistical approaches for estimating sex-specific effects in endocrine disruptors research. Environ. Health Perspect. 125, 067013 (2017).
Achenbach, T. M., McConaughy, S. H. & Howell, C. T. Child/adolescent behavioral and emotional problems: implications of cross-informant correlations for situational specificity. Psychol. Bull. 101, 213–232 (1987).
De Los Reyes, A. & Kazdin, A. E. Informant discrepancies in the assessment of childhood psychopathology: a critical review, theoretical framework, and recommendations for further study. Psychol. Bull. 131, 483–509 (2005).
Racine, N. et al. Global prevalence of depressive and anxiety symptoms in children and adolescents during Covid-19: a meta-analysis. JAMA Pediatr. 175, 1142–1150 (2021).
Hawes, M. T., Szenczy, A. K., Klein, D. N., Hajcak, G. & Nelson, B. D. Increases in depression and anxiety symptoms in adolescents and young adults during the Covid-19 pandemic. Psychol. Med. https://doi.org/10.1017/S0033291720005358 (2021).
Tang, S., Xiang, M., Cheung, T. & Xiang, Y. T. Mental health and its correlates among children and adolescents during Covid-19 school closure: the importance of parent-child discussion. J. Affect Disord. 279, 353–360 (2021).
Mohler-Kuo, M., Dzemaili, S., Foster, S., Werlen, L. & Walitza, S. Stress and mental health among children/adolescents, their parents, and young adults during the first Covid-19 lockdown in Switzerland. Int. J. Environ. Res. Public Health 18, 4668 (2021).
Qi, M. et al. The effect of social support on mental health in chinese adolescents during the outbreak of Covid-19. J. Adolesc. Health 67, 514–518 (2020).
Barnett, M., Mortensen, J., Tilley, E. & Gonzalez, H. Global and parenting-specific social support as protective factors for the well-being of Mexican American mothers of toddlers. Fam. Sci. 4, 98–109 (2013).
Masten, A. S., Lucke, C. M., Nelson, K. M. & Stallworthy, I. C. Resilience in development and psychopathology: multisystem perspectives. Annu. Rev. Clin. Psychol. 17, 521–549 (2021).
Ellis, W., Dumas, T. & Forbes, L. Physically isolated but socially connected: psychological adjustment and stress among adolescents during the initial Covid-19 crisis. Can. J. Behav. Sci. 52, 177–187 (2020).
Shrout, P. E. Measurement reliability and agreement in psychiatry. Stat. Methods Med. Res. 7, 301–317 (1998).
Sagiv, S. K., Kalkbrenner, A. E. & Bellinger, D. C. Of decrements and disorders: assessing impairments in neurodevelopment in prospective studies of environmental toxicant exposures. Environ. Health 14, 8 (2015).
Funding
This work was supported by the NIH [grant numbers T32HD049311, R01ES013744, R01ES021357, P30ES023515, R00ES027496, R24ES028522, and K99ES032480].
Author information
Authors and Affiliations
Contributions
We confirm that all coauthors have made substantial contributions to the conception and design, acquisition of data, or analysis and interpretation of data; drafting the article or revising it critically for important intellectual content; and final approval of the version to be published.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
All women provided informed consent and children provided assent.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
McGuinn, L.A., Rivera, N.R., Osorio-Valencia, E. et al. Changes in depressive and anxiety symptoms during COVID-19 in children from the PROGRESS cohort. Pediatr Res 94, 349–355 (2023). https://doi.org/10.1038/s41390-022-02379-z
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-022-02379-z
This article is cited by
-
Caregiver-reported emotional-behavioral symptoms in Spanish youth during the COVID-19 pandemic: a longitudinal study
Pediatric Research (2025)
-
Trajectory of depressive symptoms over adolescence in autistic and neurotypical youth
Molecular Autism (2024)
-
Anxiety increased among children and adolescents during pandemic-related school closures in Europe: a systematic review and meta-analysis
Child and Adolescent Psychiatry and Mental Health (2023)